Anatomy, Bony Pelvis and Lower Limb, Posterior Thigh
- Article Author:
- Thomas Anderson
- Article Editor:
- Renato Vilella
- Updated:
- 7/31/2020 5:35:06 PM
- For CME on this topic:
- Anatomy, Bony Pelvis and Lower Limb, Posterior Thigh CME
- PubMed Link:
- Anatomy, Bony Pelvis and Lower Limb, Posterior Thigh
Introduction
The posterior thigh is a functional unit of the lower body that helps to connect the pelvis to the knee. It plays a significant role in the lower limb, pelvis, and locomotor system biomechanics.
The posterior thigh has wide functions, such as the dependency of the kinetic chain to perform agonist-antagonist movements. The three muscles of the posterior thigh stabilize the knee and help to stabilize the pelvis.
Structure and Function
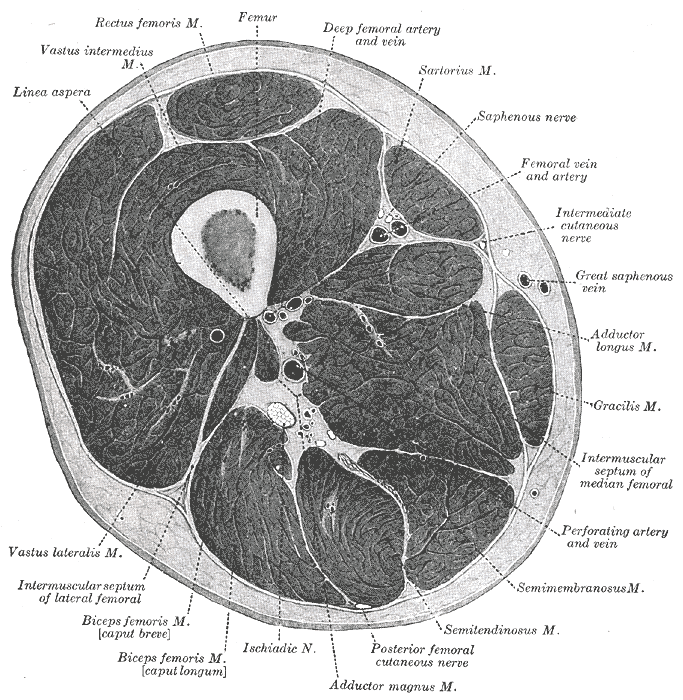
The posterior compartment of the thigh is separated from the anterior compartment by the lateral intermuscular septum and the medial compartment by the posterior intermuscular septum. The femur is the bony structure that provides support to the muscles, nerves, and vasculature in the posterior thigh. The posterior thigh is composed of three muscles: biceps femoris long and short head, semitendinosus, and semimembranosus. These three muscles are collectively referred to as the hamstring muscles. The hamstring muscles in the open kinetic chain allow extension of the hip and flexion of the knee, and when in the closed kinetic chain, allow extension of the knee.[1] Within the posterior thigh, various neurovascular and lymphatic structures aid in moving fluid to and from the lower limb. The nerves of the posterior thigh originate from the lumbar and sacral plexuses. As the sciatic nerve pierces the greater sciatic foramen, it travels down the posterior thigh posterior to the long head of the biceps femoris.[2] The sciatic nerve and its two branches provide all motor innervation to the posterior thigh.
Embryology
Each part of the human body develops from either ectoderm, mesoderm, or endoderm. Muscles, bone, connective tissue, lymphatics, blood, and other structures originate from mesoderm. Limb buds develop from mesenchymal cells that are activated by lateral plate mesoderm around four weeks of gestational age. The limbs become anatomically positioned at birth through the interaction of several growth factors. Essential growth factors include sonic hedgehog (SHH), fibroblast growth factor (FGF), and the homeobox (Hox) genes. SHH allows for the proper growth and development of the limbs and interacts with FGF to ensure the normal development of each limb. FGF and Wnt-7 genes contribute to lengthening and dorsal-ventral positioning of the limbs, respectively. Both are localized at the apical ridge. Hox genes are responsible for segmental development in the craniocaudal direction. Specifically, the posterior thigh muscles derive from the paraxial mesoderm of the lower limb buds. Around week 8 of gestational development, the lower limbs begin to rotate medially. This rotation allows the hamstring muscles to reach their final posterior position.[1][2]
Blood Supply and Lymphatics
The primary blood supply to the lower limb arises from the femoral artery and the inferior gluteal artery. The femoral artery is a continuation of the external iliac artery as it passes under the inguinal ligament. The femoral artery branches into the deep femoral artery. The inferior gluteal artery branches from the internal iliac artery to supply the proximal portions of the muscles.[3] Together, these arteries supply the majority of the posterior thigh. The venous drainage in the lower limb is mainly through the great saphenous and small saphenous veins. All lower limb veins eventually drain into the femoral vein before reaching the external iliac vein. There are two different categories of veins that are described based on their location to the fascial compartments. The veins located deep to the fascia help to drain the muscles while the veins that are superficial to the fascia help to drain the skin. Lymphatic drainage from the posterior thigh travels through various lymphatic vessels before reaching the deep inguinal nodes and, eventually, the external iliac nodes.[4]
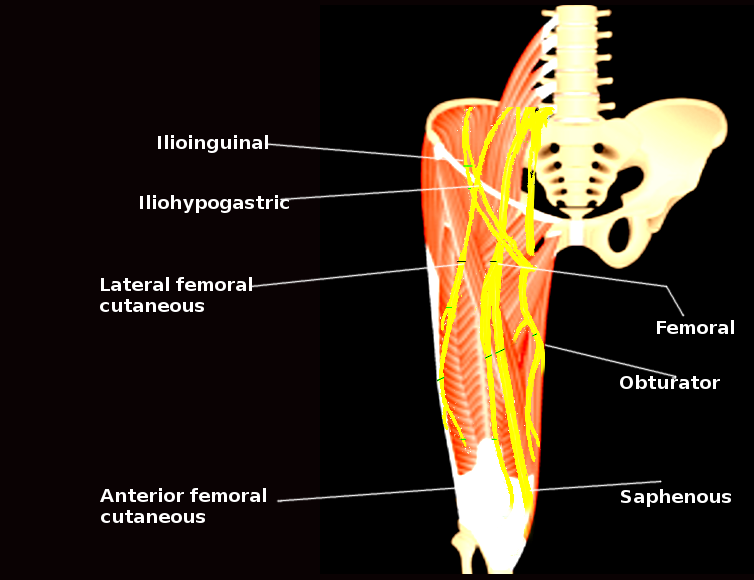
Nerves
Together, the lumbar and sacral plexus supply innervation to the lower extremity. The sacral plexus gives rise to the sciatic nerve (L4-S3), posterior femoral nerve (S1-S3), superior gluteal nerve (L4-S1), and inferior gluteal nerve (L5-S2).[5] All motor innervation to the posterior thigh derives from the tibial division of the sciatic nerve except for the short head of the biceps femoris, which is innervated by the peroneal division of the sciatic nerve.[6] The posterior cutaneous nerve of the thigh supplies sensation to the skin of the perineum and posterior surface of the thigh.[7]
Muscles
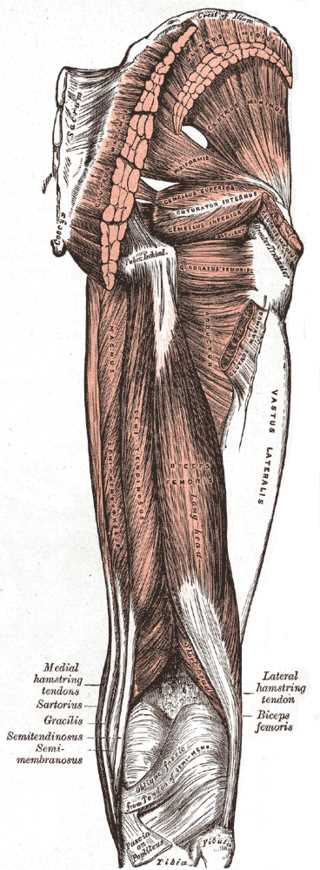
The muscles that make up the posterior compartment of the leg include the biceps femoris, the semitendinosus, and the semimembranosus.[8] Two heads make up the biceps femoris, a short head, and a long head. The semitendinosus and biceps femoris long head muscles sit superficial to the semimembranosus and biceps femoris short head muscles. The perforating branches of the deep femoral artery provide blood supply to all four muscles. The biceps femoris short head originates from the linea aspera and lateral supracondylar line of femur.[9] The biceps femoris long head, semitendinosus, and semimembranosus muscles all originate from the ischial tuberosity. The biceps femoris muscles attach to the lateral side of the head of the fibula. The semitendinosus and semimembranosus attach to the medial surface of the tibia. As a group, the hamstring muscles primarily work to extend the hip and flex the knee. The exception to this rule is the short head of the biceps femoris, which only acts to flex the knee. These movements are an integral part of normal gait and daily function. The hamstrings provide stability while standing by securing the hip joint so the body can remain upright. Additionally, the hamstrings provide slight external or internal rotation based on insertion points distally.[10] The innervation for these muscles is via the sciatic nerve. However, the short head of the biceps femoris receives specific innervation via the common peroneal division of the sciatic nerve. All other hamstrings receive innervation from the tibial division of the sciatic nerve.
Surgical Considerations
One of the most common tendons used in orthopedic surgery is the semitendinous tendon. The use of this tendon can result in negative changes for the locomotor system, also as the knee biomechanics.
After the use of semitendinous tendon in orthopedic surgery, the knee can be more unstable during the rehabilitation phase, and as the semitendinous muscle is a medial rotator, the individual can develop a lateral rotation movement dominance that can lead to overuse of biceps femoris and dysfunctions of near joints, also by overuse.[11]
Clinical Significance
The popliteal fossa is of clinical importance when considering posterior knee dislocation or needing to harvest a vessel for graft. The diamond-shaped fossa is bound by the semimembranosus and semitendinosus superomedially, the lateral and medial heads of the gastrocnemius inferolaterally and inferomedially, the biceps femoris superolaterally, and the skin and popliteal fascia superficially. The most superficial structure in the popliteal fossa is the sciatic nerve, which splits at the apex of the fossa into the tibial and common peroneal nerves. The next deepest structure is the popliteal vein. Finally, the popliteal artery is the deepest neurovascular structure before reaching the knee joint. The popliteal artery gives off five genicular branches that supply the knee capsule and ligaments. If there were a mass or injury that caused occlusion to the popliteal artery, then the blood supply to the knee would be compromised.
Sciatica is a term commonly used to describe radiating leg pain. It refers to inflammation or compression of the sciatic nerve roots. There is no clear definition of sciatica, leading to variation in distinguishing it from other sources of low back pain. Some common signs and symptoms of sciatica are pain that radiates from the lower back down the posterior thigh, knee weakness, difficulty in rotating the ankle, and slow ankle reflexes. There are paresthesia, numbness, and weakness in areas innervated by the sciatic nerve. The etiology of sciatica is multifactorial and can stem from anything related to compression and inflammation of the nerve or its nerve roots. Some common examples are piriformis syndrome, pregnancy, herniated vertebral discs, or lumbar stenosis. An anomaly seen in roughly 10% of the population that is related to piriformis syndrome occurs when the sciatic nerve either penetrates the piriformis muscle or travels superior to the muscle before descending the posterior thigh. These variations lead to an easier mechanism of compression of the sciatic nerve with only slight hypertrophy in the piriformis muscle.[12][13][14]
A common injury among athletes of all levels is a hamstring strain. The injury typically occurs with sudden lengthening of the hamstrings or rapid changes in speed or direction. These actions are common for people involved in high-risk activities like football, track, and rugby. In addition to being highly prevalent, hamstring injuries tend to recur due to poor rehabilitation or premature return to activity. Because the biceps femoris has the greatest musculotendinous stretch, it is the most frequently injured muscle of the hamstrings from running. A typical hamstring strain is characterized by pain in the posterior thigh, which can be exacerbated by passive knee extension, resisted knee flexion, or hip extension. When evaluating anyone with a possible hamstring injury, clinicians must consider other diagnostic possibilities such as tight quadriceps tendon, lumbosacral radiculopathy, piriformis syndrome, strong lumbopelvic muscles, or adductor strain.[15]
(Click Image to Enlarge)
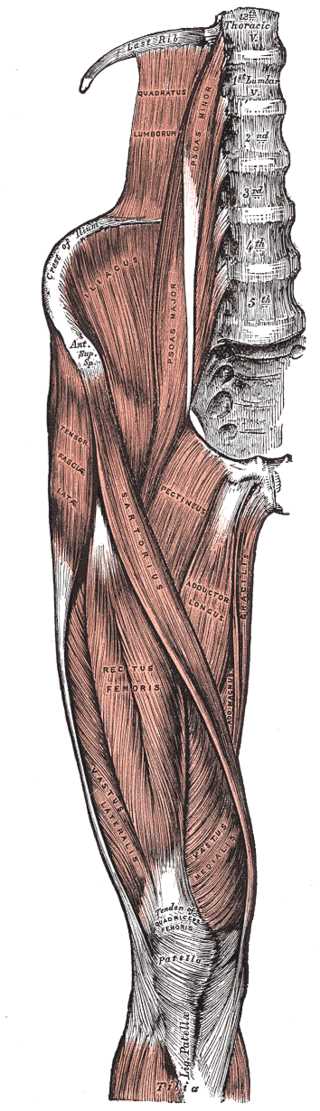
Tensor Fasciae Latae Muscles, Abductor of the Thigh, Thoracic Vertebrae, Quadratus Lumborum, Psoas Minor and Major, Crest of Ilium, Anterior Superior Spine, Iliacus, Tensor Fascia Latae, Sartorius, Pectineus, Adductor Longus, Gracilis, Adductor Magnus, Rectus Femoris, Vastus Lateralis and Medialis, Tibia, Patella, Tendon of Quadriceps
Contributed by Gray's Anatomy Plates
(Click Image to Enlarge)