Anatomy, Abdomen and Pelvis, Female Internal Genitals
- Article Author:
- Brittany Hoare
- Article Editor:
- Yusuf Khan
- Updated:
- 7/31/2020 3:59:09 PM
- For CME on this topic:
- Anatomy, Abdomen and Pelvis, Female Internal Genitals CME
- PubMed Link:
- Anatomy, Abdomen and Pelvis, Female Internal Genitals
Introduction
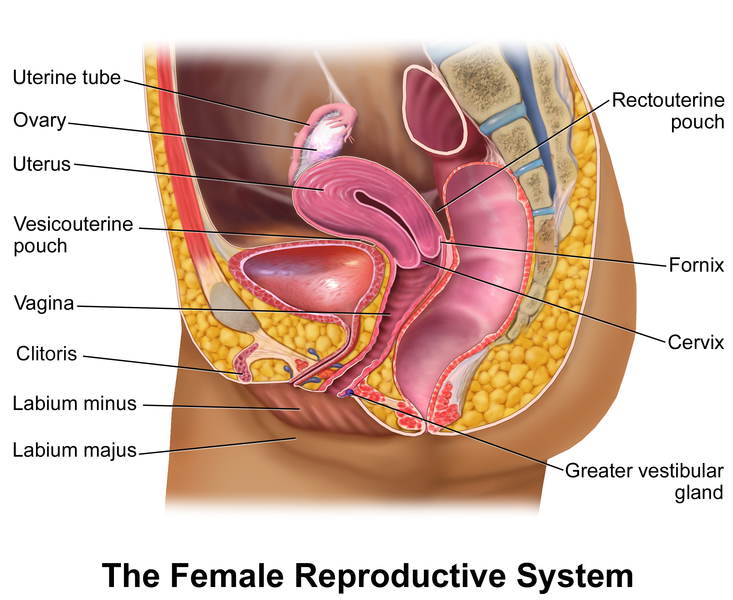
The female reproductive system is an intricate arrangement of structures that can separate into external and internal genitalia. The external genitalia comprises the structures outside of the true pelvis, including the labia majora and minora, vestibule, Bartholin glands, Skene glands, clitoris, mons pubis, perineum, urethral meatus, and periurethral area. The internal genitalia is the structures within the true pelvis, including the vagina, cervix, uterus, fallopian tubes, and ovaries, the latter being the focus of this article. It is vital for medical professionals, especially those in the field of obstetrics and gynecology, studying the female reproductive system to understand anatomy exclusive to females.
Structure and Function
The uterus is the central anatomical landmark of the female internal genitals and pelvic anatomy. It is a highly muscular, childbearing organ in females, approximating 3 x 2 x 1 inches in size in a nulliparous. Even though the uterus is primarily a pelvic organ, but during later stages of pregnancy due to hypertrophy and hyperplasia of the myometrium, it can reach up to the epigastric region. The most common anatomical position of the uterus is anteverted-anteflexed. Anteversion is the angulation between the long axis of the cervix and the vagina, which nears the right angle.[1][2] Anteflexion is the angulation between the long axis of the body and the cervix, which is an obtuse angle around 120 to 125 degrees. In an anteverted-anteflexed position, the uterine body sits within the vesicouterine space. In rare cases, the uterus may be retroverted-retroflexed, causing the uterine body to be within the Douglas pouch. The shape of the uterus has been described as “pyriform” on examination in a sagittal plane. It has four parts: the fundus, body, isthmus, and cervix.[3][4] The uterine body is the largest portion, while the uterine isthmus is the location where the uterine body meets the cervix.[4] The fundus is that part of the uterus, which is above the opening of the fallopian tubes into the uterine cavity. The whole of the uterine cavity has a very special lining membrane called the endometrium. This endometrium will shed during menstruation; inflammation of this membrane is endometritis, which, when chronic, can be lead to infertility.[5]
The ovaries are the primary organs of the female reproductive system. They are oval-shaped gonadal structures, approximately 3 x 1.5 x 1 cm in size, and homologous with the testis in males. They are present in pairs with the long axis oriented downward and forward. The ovaries are within the pelvis, just lateral to the uterus. They lie within the ovarian fossa, in front of the ureters, and behind the external iliac vessels.[3] In nulliparous females, they are pinkish with a smooth outer surface, but in multiparous, they are more greyish with a puckered surface due to repeated ovulations. The ovaries are entirely covered with peritoneum except for the mesovarian (anterior) border through which all the blood vessels, nerves, and lymphatics pass. They contain thousands of follicles. Each month, one follicle will develop into the dominant follicle (Graafian follicle), which releases an ovum during ovulation.[4] On ultrasound, the ovary appears as having an echoic central area and a peripheral region, with the former corresponding to the stroma and the later corresponding to the cortex.[3] The ovaries secrete two steroid hormones, estrogen, and progesterone under the direct control of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) secreted by the pituitary. These hormones play a significant role in many different aspects of the life of a female.[6][7][8][7] The lower, short, but broad cylindrical part extending from the internal os to the external os is the cervix. It has a narrow central lumen, which opens into the uterine cavity as internal os and into the vagina as the external os. The external os is seen as circular opening in nulliparous and as a horizontal slit in multiparous. This horizontal slit divides the cervix into an anterior and posterior lip. The narrow upper third of the cervix is the isthmus, which defines the lower uterine segment and is the site for the lower segment cesarean sections (LSCS).[9]
The ovaries link to the uterus through fallopian tubes, which function to carry the zygote to the uterine cavity for implantation. The fallopian tubes (also known as oviduct, uterine tube) divide into the fimbriated infundibulum, ampulla, isthmus, and intramural parts.[10] The ampullary part is the usual site for fertilization.[11] The fallopian tube also helps in bringing the sperm and ovum to this site of fertilization. The infundibulum is the most later part, that is funnel-shaped with finger-like projections hanging from the sides called fimbriae. This part opens into the peritoneal cavity and is in contact with the ovaries through some of its fimbriae. The intramural is the most narrow and medial part of the fallopian tube that is present within the wall of the uterus. Each region represents characteristic physiologic features. Salpingitis is a bacterial infection of the fallopian tube. It may be acute or chronic inflammation and most commonly results from Neisseria gonorrhoeae or Chlamydia trachomatis. It may lead to scarring of the fallopian tubes and predispose to infertility and ectopic tubal pregnancy. Tubal infertility caused by disruption of the integrity of the fallopian tubes by infusion, endometriosis, or surgical complication is an important consideration when evaluating women with unexplained infertility.[10] Ectopic tubal pregnancy most commonly occurs in the ampulla of the fallopian tube. Common predisposing factors include salpingitis, pelvic surgery, or pelvic inflammatory disease. This diagnosis may be confused with appendicitis in a young woman, and early differentiation of the two diagnoses is crucial.
The vagina is a fibromuscular canal ranging from 6 to 8 cm. in length. It is anatomically located anteriorly to the rectum and posteriorly to the wall of the urinary bladder and the urethra. This canal directs downwards and forwards. Because of the oblique nature of the vagina, the anterior wall is slightly shorter, i.e., about 6 cm compared to the posterior wall, which is about 8 cm. The upper segment of the vaginal forms a vaginal vault by being enclosed within the vaginal portion of the cervix.[12] The cervix extends into the vagina, forming a channel between the two structures. Thus the cervix is divided into a supravaginal and a vaginal part. The narrow space between the cervix and the wall of the vaginal is the fornix. The recess between the anterior lip of the cervix and the anterior wall of the vagina is the anterior fornix. Similarly, the recess between the posterior lip of the cervix and the wall of the vagina is the posterior fornix. The space on either side between the cervix and the lateral wall of the vagina is known as the lateral fornices. The posterior fornix is the deepest and is a common site for ruptures, foreign bodies, and malignancies.[13][14][15][16]
Embryology
Before the determination of phenotypic sex, the gonads are classified as "unisex" and have the potential to develop into testes or ovaries.[17] The embryologic development of the female internal genitals has been a topic of research in recent years. The determination of female sexual differentiation is by the absence of the SRY (sex-determining region on Y) gene, a gene on the short arm of the Y chromosome (Yp11). When present, the SRY gene will cause the indifferent embryo to develop into the male phenotype.
The belief is that the ovaries derive from the gonadal ridge. But the primordial germ cells develop in epiblast and migrate to endoderm cells in the yolk sac. They finally appear in the genital ridges in 6th week. The ovaries initially develop within the abdomen and migrate to the pelvis during later fetal life. Even though they migrate into the pelvis, they still retain their blood supply, nerve supply, and lymphatic drainage back to their site of origin, the upper abdomen.[18] The gubernaculum is involved in the formation of the ovarian ligament and the round ligament of the uterus. In the recent decade, there has been ongoing research to identify a female determining sex gene. So far, the "Z" gene hypothesis, which names FoxL2 as a possible ovary determining factor, has been identified. Other genes believed to be involved, including Dax1 and Wnt4, which may have similar effects; however, many unanswered questions remain in this pathway.[17]
The paramesonephric duct (Mullerian duct) is the embryologic derivative of the genital ducts. The cranial portions form the uterine tubes, while the caudal parts form the uterovaginal primordium. The uterovaginal primordium gives rise to the uterus, cervix, and superior third of the vagina. The vaginal plate is a derivative of the sinovaginal bulbs. It canalizes to form the lower two-thirds of the vagina. All of these derivatives are surrounded by a layer of myometrium that develops from mesenchyme. The outermost covering is the perimetrium that develops from folds of the peritoneum.
Embryologic defects that are important to consider including unicornuate uterus anomalies, where one paramesonephric duct fails to develop, Didelphys anomalies, where there is a complete lack of fusion of the paramesonephric duct and bicornuate uterus anomalies where there is a partial fusion of the paramesonephric duct.[19] Bicornuate uterus anomalies are associated with the highest risk of infertility.
The mesonephric (Wolffian) duct disappears in the case of females, except a small cranial part that remains as epoophoron and paroophoron. The remnant of the mesonephric duct is called the Gartner's duct. A small caudal portion of this duct is seen and referred to as Gartner's duct cyst within the wall of the uterus or vagina.[20]
Blood Supply and Lymphatics
The Ovarian artery is a branch of the abdominal aorta; it reaches the ovary through the suspensory ligament of the ovary. Even though ovaries are pelvic organs, they derive their blood supply from the abdominal aorta indicating their site origin. The uterine artery originates from the anterior division of the internal iliac artery along with the umbilical artery in a common trunk.[21] It serves as the main arterial supply of the uterus. The uterine artery that is highly tortuous travels across the pelvic floor in the cardinal ligament runs anteriorly and superiorly to the ureter close to the lateral fornix of the vagina. It ends by anastomosing with the ovarian artery within the broad ligament of the uterus. Ligation of the uterine artery during a hysterectomy is typically at the level of the internal cervical os.[21] The small, inferior branch of the uterine artery becomes the vaginal artery and supplies the cervix and vagina. The vaginal artery may also arise from the internal iliac artery.
The veins of the female internal genitals usually correspond to the arteries. The uterine vein follows the course of the uterine artery and is also contained within the cardinal ligament; it drains into the internal iliac vein. The ovarian veins receive blood from the ovaries; the right ovarian vein drains directly into the IVC while the left ovarian vein drains into the left renal vein. Malignancies in the pelvis may metastasize to the vertebral column or spinal cord via connections of the pelvic veins.
The lymphatic flow from the uterus, cervix, and vagina drains into the internal and external iliac nodes. Lymph vessels from the ovary and fallopian tube drain directly into the paraaortic nodes.
Nerves
The nerve fibers that feed the pelvis are both parasympathetic and sympathetic. The preganglionic fibers are in the sacral parasympathetics (S2-S4) in the spinal cord. Their processes run into pelvic splanchnic nerves and relay inside the pelvic organs within the intramural plexus (the postganglionic neuron). The sensory fibers from S2-S4 dorsal root ganglia travel with parasympathetic fibers and carry pain sensations from the organs. Sympathetic fibers of preganglionic neurons (T12-L2) form the sacral splanchnic nerves. They contribute to the inferior hypogastric plexus, which is the location of the postganglionic neurons. The pudendal nerve provides sensory innervation to the lower vagina. A pudendal nerve block is an option during early labor to relieve pain for the mother.[22] It may be blocked by piercing the vaginal wall posterolaterally, using the ischial spine as a landmark. It may also be performed percutaneously along the medial side of the ischial tuberosity. However, this method does not affect the pain from uterine contractions and is no longer commonly used.
Muscles
Several muscles of the pelvic diaphragm support the uterus, the urogenital diaphragm, and the round, broad, lateral, and cardinal ligaments. The pelvic diaphragm includes the following muscles: piriformis, coccygeus, iliococcygeus, pubococcygeus, and puborectalis. The pubococcygeus, puborectalis, and iliococcygeus muscles together are known as the levator ani muscles. Vaginal delivery is a major cause of levator ani defects, genital organ prolapse, and urinary incontinence.[23] Studies have shown that during the second stage of labor, the pubococcygeus muscle bears the largest tissue strain compared to other pelvic floor muscles.[23] The upper portion of the posterior vagina is suspended and held in place by several lateral connections. Prolapse of this area can occur if there are defects in the perineal body, which most commonly occurs following vaginal delivery. The role of episiotomy in the prevention of perineal body tears is controversial.[24][25]
The major ligaments that support the uterus include the round ligament, transverse cervical ligament (cardinal ligament), uterosacral ligament, and broad ligament. The cardinal ligament reaches from the cervix to the sidewall of the pelvis and appears at the base of the broad ligament. The uterosacral ligament plays a major role in keeping the uterus in the anteverted position. It extends from the cervix to the sacrum and supports the uterus posteriorly. The pubocervical ligament provides anterior support to the uterus, helping to prevent cystocele. The broad ligament is a double folding of the peritoneum, divided into four regions composed of the mesosalpinx, mesovarium, mesometrium, and the suspensory ligament of the ovary. It overlies the ovaries, uterus and fallopian tubes, and secures the uterus laterally to the sidewall of the pelvis.[23]
When the supportive structures of the pelvis fail, the result is pelvic organ prolapse. It is a common difficulty for women and is usually treated with conservative management, mechanical support using pessaries, or surgical repair. Laparoscopic promontofixation is a surgical option that has excellent long-term results.[26] Additionally, laparoscopic promontofixation is associated with low recurrence and morbidity rates, and improved quality of life in women with pelvic organ prolapse.[26]
Physiologic Variants
A common physiologic variant is the presence of a retroverted uterus. The presence of a retroverted uterus is not associated with a higher incidence of infertility, urinary tract infection, or hyperemesis gravidarum. However, studies have demonstrated that the incidence of early pregnancy bleeding and spontaneous abortion are significantly higher in those with a retroverted gravid uterus.[27] These patients require careful management, and the clinician should not perform bimanual manipulation in those with a retroverted gravid uterus.[27]
Additionally, the origin of the uterine artery may vary in up to 1 of 5 cases.[21] The origin is with the uterine artery beginning directly from the internal iliac artery, superior gluteal, obturator, or internal pudendal artery.[21] A particularly difficult variant is when the uterine artery undertakes a C-shaped configuration, where a second branch originates directly from the internal iliac artery. Medical professionals must anticipate these variants during surgery for successful ligation.
Surgical Considerations
A surgeon needs to be aware of the anatomical relationships when operating on the female internal genitals. Postpartum Hemorrhage is a chief complication, especially after Cesarean Section. Typically, postpartum hemorrhage management is by clamping or embolization of the uterine artery. If bleeding persists, the practitioner should clamp the internal iliac artery below the origin of the superior gluteal artery. Some studies have suggested that several arteries, including the uterine artery, are recruited to respond to the demand from the gravid uterus.[28] In these cases, treatment of recurrent or persistent postpartum hemorrhage after bilateral uterine artery embolization may have treatment with round ligament artery embolization.[28]
Being aware of the position of the ureter during hysterectomy is crucial; it is at the most significant risk of being ligated because of its proximity to the uterine artery and cervix. It travels under the cardinal ligament and is an important clinical association of which to be mindful. Furthermore, during a hysterectomy, the uterine artery is usually isolated to prevent unintentional ligation and massive bleeding. After clamping, it is ligated at the level of the internal cervical os during a hysterectomy.[21]
There have been rare cases of femoral herniation of the internal female genitalia.[29] Femoral hernias may occur in females, but the herniated tissue is usually omentum or bowel. However, in this case, the ovary, fallopian tube, and uterus were contained within the hernia; therefore, it is a possibility that merits consideration when managing these situations.
Clinical Significance
There are several significant clinical correlations to consider while analyzing the female internal genitalia:
- The uterus typically sits in an anteverted, ante flexed position. A retroverted uterus is associated with an increased risk of early bleeding and spontaneous abortion. The caesarian sections have correlated with a retroverted uterus.[30]
- Embryologic defects in the shape of the uterus, such as Bicornuate uterus anomalies, may also lead to infertility and first-trimester spontaneous miscarriages.
- The uterus receives vascular supply from the uterine artery, an anterior division of the internal iliac artery, which travels within the cardinal ligament. Physiologic variants of the uterine artery may be present in many cases, and surgeons must anticipate these cases for appropriate ligation of the artery.[31]
- Moreover, there must be careful consideration of the ureter during surgeries involving the female genitals to avoid unintentional ligation.
- The ovaries are the gonadal structures of females; they derive from the gonadal ridge. The “Z” gene hypothesis names FoxL2, Dax1, and Wnt4 as possible ovary determining factors.[32]
- The ovaries obtain their blood supply from the ovarian arteries, and their lymphatic drainage is directed to the paraaortic nodes.
- The fallopian tubes are the connections from the ovary to the uterus. Salpingitis may lead to scarring of the fallopian tubes and predispose to infertility and ectopic tubal pregnancy. Tubal infertility must be a consideration in young women with infertility of undetermined significance.[33]
- A pudendal nerve block is an option to alleviate the pain of labor. However, they are no longer commonly used since the popularity of epidurals has increased.
- The pubococcygeus muscle bears the largest tissue strain compared to other pelvic floor muscles and is at significant risk of being compromised during vaginal delivery.
- Studies have shown that embolization of the round ligament may help to control recurrent or persistent postpartum hemorrhage.[34] Interventional radiologists need to consider this as an alternative for hard to control bleeds.[35]
- There have been rare cases of femoral herniation containing the ovary, fallopian tube, and uterus.[29][36][37][36][29]
- Pelvic organ prolapse is prevalent among women.[38] There are many treatment strategies, including conservative management, mechanical support, or surgical repair.[39] Laparoscopic promontofixation is a surgical approach that is an option and generally delivers improved long term outcomes.
(Click Image to Enlarge)

female reproductive system blood supply, Tubal Vessels, Anastomosis of uterine and ovarian arteries, Helicine branches, Fallopian tub, Ovarian artery, Uterine venous plexus, Uterosacral ligament, Ureter, Uterine artery and veins, Superior vaginal arteries, Vaginal venous plexus, Os uteri
Contributed by Gray's Anatomy Plates
(Click Image to Enlarge)