Anatomy, Head and Neck, Nasal Concha
- Article Author:
- Bianca Georgakopoulos
- Article Editor:
- Patrick Le
- Updated:
- 8/31/2020 6:48:21 PM
- For CME on this topic:
- Anatomy, Head and Neck, Nasal Concha CME
- PubMed Link:
- Anatomy, Head and Neck, Nasal Concha
Introduction
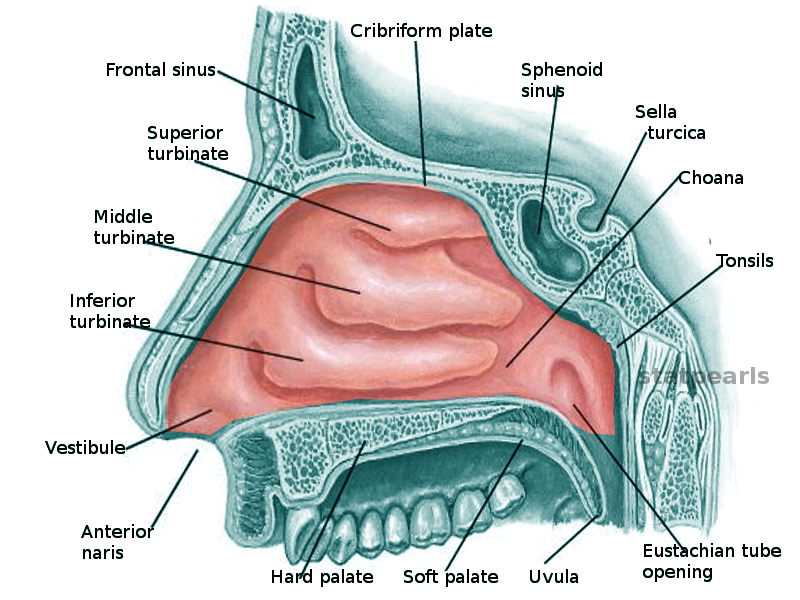
Within the nasal cavity, there are three separate turbinates: superior, middle, and inferior. Turbinates are also called concha. Because the nasal cavity is symmetrical, there are technically pairs of turbinates, leading to 6 in total for an average human. These structures are on the lateral nasal wall. The inferior turbinate is independent of the superior and middle turbinates that extend from the ethmoid bones. The space between each turbinate and the nasal wall is called a meatus.[1] These structures are known classically for aiding warmth of the air from the external environment, as well as possible pathology leading to a common sleep condition known as obstructive sleep apnea.
Structure and Function
All three of the turbinates are responsible for warmth, humidification, and filtration. The inferior turbinate has respiratory and immune functions. Its structure is cartilage under soft tissue covered with respiratory epithelium. The folded structures of the turbinates increase the surface area of the cavity. The inferior turbinate has an immune response because it is the first tissue to come into contact with the outside air. Because of this, it decides pathogenicity and can trigger innate and adaptive immune reactions.[2] The other two turbinates have similar structures in appearance, but stem from the ethmoid bone, and do not an immune function.[1]
Embryology
The cells responsible for the growth of turbinates are the mesenchymal stem cells. They are heterogeneous cells with pluripotent capacity and can become mesodermal as well as non-mesodermal lines of cells.[3] The buds of the turbinates appear at Week 7. At weeks 9 to 10, the maxilla begins to ossify and enlarge. During Weeks 17 to 18, the nasal capsule begins to ossify along with the inferior turbinates. The middle turbinates growth starts in Week 20. After Week 21, the superior turbinates will begin to ossify. The middle turbinates come from the second ethmoturbinal material, while the superior turbinates come from third and fourth ethmoturbinal materials. The turbinates also derive from olfactory fascial units. Their growth directionality is key to the human’s nasal cavity formation.[4]
Blood Supply and Lymphatics
The main supplier of blood to the nasal cavity is via the internal and external carotids and their associated branches. The external carotid’s sphenopalatine artery is the primary vascular source. Regardless of this known information, there is debate over specific blood suppliers of the nasal cavity because many studies do not agree, and name vasculature by unaccepted nomenclature. Regardless of this, MacArthur et al. performed a cadaveric study in 2016 with the following results. The superior turbinate receives supply from the posterior septal artery, The inferior turbinate artery, and the middle turbinate artery is the arterial support for the three turbinates posteriorly. The anterior arterial support of the middle turbinate is from the anterior ethmoid artery. The inferior turbinate is supported anteriorly via the lateral anterior ethmoidal artery and the anterior lateral nasal artery.[5]
Nerves
Parasympathetic and sympathetic nerves supply the turbinates. The parasympathetic neurons come from the superior salivary nucleus located in the midbrain. From there, the parasympathetic neurons join the facial nerve neurons. They will then separate at the geniculate ganglion and become the greater superficial petrosal nerve, then synapsing in the sphenopalatine ganglion, entering the sphenopalatine foramina. The postganglionic parasympathetic fibers separate into the mucosa and submucosa. These postganglionic fibers have acetylcholine, vasoactive intestinal peptide, and secretoneurin. When these fibers become stimulated, the glands secrete, vasodilation occurs, leading to congestion.[2]
The sympathetic neurons originate in the hypothalamus. They exist in the CNS within the cervical spine, and journey to combine with the facial nerve parasympathetic neurons to make the vidian nerve, The sympathetic neurons innervate the mucosa and submucosa. These sympathetic fibers have norepinephrine and neuropeptide Y, leading to vasoconstriction and decreasing airway resistance.[2]
The nasal cycle is an essential asymmetrical process for areas of spontaneous congestion and decongestion of mucosal veins. When there is more blood flow, airflow decreases. The left and right nasal cavities alternate on which gets congested at a particular instant.[2]
Muscles
The paranasal sinuses include the anterior, posterior, and sphenoid. The anterior division includes maxillary, anterior ethmoid, and frontal sinuses. The anterior sinuses drain through the osteomeatal complex located in the middle meatus. The posterior ethmoid sinus drains through the superior meatus. The sphenoid sinus uses the sphenoethmoid recess to drain, located behind the superior turbinate. The paranasal sinuses have a lining of pseudostratified ciliated columnar epithelium. The cilia beat to carry trapped particles from the sinus to the nose.[1]
Physiologic Variants
There are many variants to the turbinates like bifid and concha bullosa. Concha bullosa results from pneumatization of the middle turbinate. There have also been reports of bifid middle or inferior turbinates, but these are quite rare.[6]
Surgical Considerations
Removal of the middle and the superior turbinates, along with the ethmoid air cells leads to more post-operative space and permanent alterations in the flow of air. These typically get removed for intracranial surgery.[7] Other surgeries performed on turbinates are due to hypertrophy and congestion because of allergic/ non-allergic triggers of inflammation.[1] Empty nose syndrome is rare but tends to occur in people who have turbinate surgery; this is not an immediate consequence of surgery, but this syndrome occurs after many years. Most patients will present with persistent nasal obstruction, which is unusual due to their wide and clear nasal cavities. Other symptoms include extreme nasal crusting, malodor originating in the nasal cavity, facial pain, dyspnea, and sleep problems. This syndrome is a diagnosis of exclusion.[8]
Clinical Significance
Nasal obstruction is a prevalent symptom in the practice of an otolaryngologist. It presents most frequently in cases of sleep apnea. Although there are many different causes for obstruction, a common surgery performed include reducing the turbinates. Many different procedures help to do this, including turbinectomy, turbinoplasty, electrocautery, laser, cryotherapy, or resection by radiofrequency. Typically, these procedures include shaving down the turbinates so that there is less physical obstruction above the vestibule. Surgeons usually perform these procedures because of turbinates that have hypertrophied over time and are much larger than their intended size.[9]
Other Issues
There are a few tumors associated with turbinates. One cause, in particular, includes sinonasal osteoblastoma. These are benign growths that rarely develop in the middle turbinates.[10]