Neuroanatomy, Ciliary Ganglion
- Article Author:
- Nikha Bhardwaj
- Article Editor:
- Abhijeet Joshi
- Updated:
- 7/27/2020 9:18:02 PM
- For CME on this topic:
- Neuroanatomy, Ciliary Ganglion CME
- PubMed Link:
- Neuroanatomy, Ciliary Ganglion
Introduction
The smooth functioning of the human body depends on coordination between somatic and visceral parts of the nervous system. Visceral part of the nervous system is commonly known as the autonomic nervous system. It has two components parasympathetic and sympathetic. Visceral efferent has at least two sets of neurons, i.e. preganglionic and postganglionic neurons.
Fibers of cranial parasympathetic ganglion originate from brain stem nuclei. After leaving the brainstem, these fiber synapses in the peripheral parasympathetic ganglion. There are four peripheral parasympathetic ganglia (ciliary ganglion, pterygopalatine ganglion, otic ganglion, and submandibular ganglion) situated in the head and neck region. Postganglionic parasympathetic fibers provide parasympathetic innervation to the target organ.
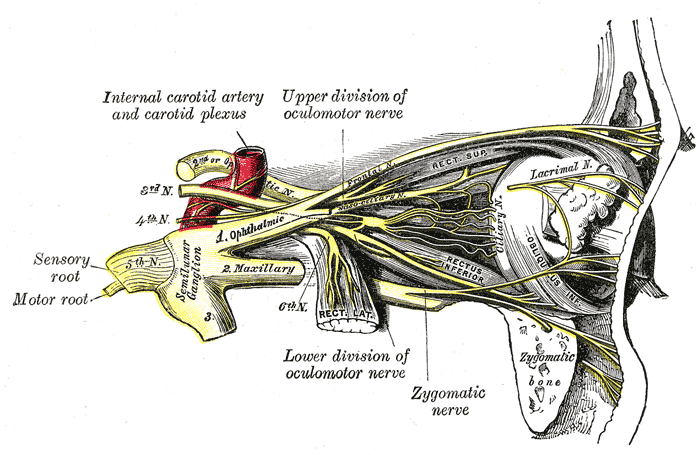
Ciliary ganglion is a peripheral parasympathetic ganglion. It is situated near the apex of orbit between the optic nerve and lateral rectus muscle. It is related medially to the ophthalmic artery and laterally to the lateral rectus muscle.
Structure and Function
It is a small irregular shaped structure; its shape varies from pinhead, irregular, oval to rectangular. It is situated approximately 1 cm in front of the medial end of the superior orbital fissure. Here it is embedded in orbital fat and is connected to the nasociliary nerve. It is a collection of multipolar neurons. Three roots of the ciliary ganglion are attached to its posterior border. These roots are motor root, sensory root, and sympathetic root.
The motor root is parasympathetic. Preganglionic parasympathetic fibers arise from the Edinger Westphal nucleus. Then these fibers pass through the nerve to inferior oblique muscle branch of the oculomotor nerve and reach the ciliary ganglion. At the ciliary ganglion, preganglionic fibers synapse with postganglionic fibers. Postganglionic fibers pass through short ciliary nerve and end by supplying sphincter pupillae and ciliaris muscle.
The sensory root derives from the nasociliary nerve. Sensory fibers from eyeball pass through ganglion uninterrupted. It carries general sensations from the cornea, iris, and ciliary body.
The sympathetic root forms from the plexus of post-ganglionic sympathetic fibers from superior cervical sympathetic ganglion around the internal carotid artery, then it enters into orbit through the common tendinous ring of the superior orbital fissure. Post-ganglionic sympathetic fibers from superior cervical sympathetic ganglion pass through ciliary ganglion uninterrupted and distributed via short ciliary nerves. Sympathetic root supplies blood vessels of the eyeball.[1][2][3]
Embryology
The autonomic nervous system develops from neural crest cells. Precursors of Schwann cells are multipotent cells derived from the neural crest. Precursors of Schwann cells generate Schwann cells, neuroendocrine cells, autonomic neurons, melanocyte, and some other cells. Neural crest cells of the mesencephalon and metencephalon junction contribute to the development of ciliary ganglion.Before the closure of neural tube closure, neural crest cells migrate from midbrain and hindbrain junction. In neural tube, neurons arrange in two lamina- basal lamina and alar lamina. Neurons of the basal lamina are motor in nature and from lateral to medial side arranged in three columns named as somatomotor (somatic efferent), branchio-motor (special visceral efferent) and visceral-motor ( general visceral motor). The dorsal nucleus of the vagus nerve, the inferior salivatory nucleus of the glossopharyngeal nerve, the superior salivatory nucleus of facial and Edinger-Westphal nucleus of oculomotor represent viscera-motor component of the cranial nerve. Viscero-motor component of the cranial nerve is associated with parasympathetic ganglions, and from these nucleus preganglionic parasympathetic fibers of concerned ganglion originates. Folic acid deficiency, infections, exposure to the teratogen, mutation during the early embryonic period can lead to the defect in the development of neural tube, facial defects, ocular defects, etc..[4][5][6][7]
Blood Supply and Lymphatics
It receives vascular supply from branches of the posterior ciliary artery, central retinal arteries, and muscular branches.[8]
Nerves
As described above, three roots (parasympathetic, sympathetic, and sensory) are attached posteriorly to the ciliary ganglion, and it gives 8 to 10 branches from the anterior border. These branches are known as short ciliary nerves. These branches arrange in two bundles and get distributed by 15 to 20 branches. These branches pierce the sclera around the optic nerve and run in grooves present on the internal surface of the sclera. These branches contain all three components (parasympathetic, sympathetic, and sensory fibers). Motor fibers distributed to sphincter pupillae, ciliaris muscles, and choroidal and iridial blood vessels.[9]
Muscles
As mentioned above sphincter pupillae and ciliaris muscles are supplied by the short ciliary nerve.
Physiologic Variants
A study conducted by Janet M et al. examined the variation in receptor density and area among neurite-associated acetylcholine receptor patches (NARPs) induced by chick ciliary ganglion neurons on nearby myotubes in vitro. In this study variation in NARP size and intensity reflects regional variation in the ability of myotubes to respond to the neuronal influence because no gradient in NARP size or intensity with distance from the soma was evident; the intensities and areas of uninnervated receptor clusters (hot spots) were similar to those of NARPs; acetylcholinesterase was present at the same proportion of hot spots and NARPs at all times examined.[10]
Surgical Considerations
The ciliary ganglion can get injured during surgical management of trauma of lateral wall of the orbit, space-occupying lesions of orbit, cavernous sinus angiomas like conditions. Due to its proximity, it can easily get affected by optic or nasociliary neuromas.[11]
During eye surgeries, the clinician gives a peribulbar block above and below the orbit. In this block, ciliary nerves, oculomotor nerve, trochlear nerve get blocked, but the optic nerve is not affected.
Clinical Significance
Ciliary ganglion lesions lead to mydriasis or tonic pupil. In this condition, the pupil is non-reactive to light and slowly accommodating. Adie syndrome or Holmes Adie syndrome is a condition caused by a bacterial or viral infection, and it leads to inflammation and damage of ciliary ganglion. In this condition, the pupil is tonically dilated and slowly reacting to light, but a definite response to accommodation is present.[12] In this disease, there is a sudden denervation of the ciliary body. The re-innervation process is slow. It is usually associated with loss of deep tendon reflex.
In addition to Adie syndrome, a tonic pupil can result from other conditions like Ross syndrome, diabetic neuropathy, infection of ciliary ganglion like Herpes zoster virus infection, trauma to the ciliary ganglion, damage to the short ciliary nerve, intra-orbital tumors, damage to Edinger Westphal nucleus, etc.