Anatomy, Shoulder and Upper Limb, Wrist Flexor Retinaculum
- Article Author:
- Nathaniel Deak
- Article Editor:
- Bruno Bordoni
- Updated:
- 11/2/2020 7:01:30 AM
- For CME on this topic:
- Anatomy, Shoulder and Upper Limb, Wrist Flexor Retinaculum CME
- PubMed Link:
- Anatomy, Shoulder and Upper Limb, Wrist Flexor Retinaculum
Introduction
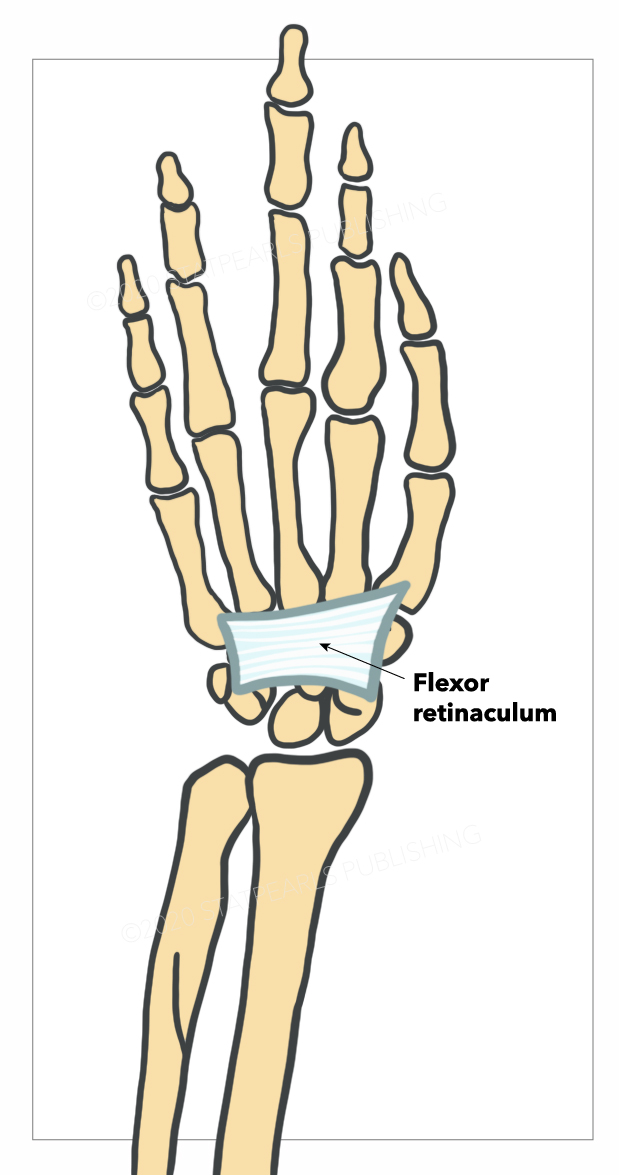
The flexor retinaculum is a fibrous connective tissue band that forms the anterior roof of the carpal tunnel. Many experts consider the flexor retinaculum synonymous with the transverse carpal ligament and the annular ligament; for this discussion, they will be considered the same structure. The flexor retinaculum protects nine of the forearm flexor tendons and median nerve as they pass through the carpal tunnel.[1] If this tissue becomes inflamed, swollen, or fibrotic, the median nerve can become irritated or compressed, leading to carpal tunnel syndrome.
Structure and Function
The flexor retinaculum begins when the longitudinally oriented fibers of the forearm's antebrachial fascia fibers abruptly thicken and change direction. The fibers change orientation to a transverse orientation. The flexor retinaculum thickens proximally to distally, ranging in thickness from 1.5 mm to 6.0 mm.[1] The structure is about 3 centimeters long and about 2.5 centimeters wide. The flexor retinaculum attaches laterally and medially to the carpals bone. Specifically, the flexor retinaculum attaches to the scaphoid tuberosity and trapezial ridge radially and the pisiform and the hook of hamate ulnarly.[2] The flexor retinaculum forms the carpal tunnel's volar boundary, while the carpal bones form the dorsal boundary. Contained below the flexor retinaculum within the carpal tunnel are the four flexor digitorum superficialis tendons, the four flexor digitorum profundus tendons, the single flexor pollicis tendon, as well as the median nerve.[1]
Its front face gives rise to some muscles of the eminence thenar and of the eminence hypothenar and is related to the tendon of the long palmar muscle that adheres to it. The upper margin continues in the palmar carpal ligament, and the lower margin merges with the palmar aponeurosis.
Its principal function is to serve as a pulley for the carpal flexor muscles and stabilize the carpal system's morphology.
Embryology
Its constitution is mainly of collagen fibers, whose embryological origin is the mesodermal leaflet (hypaxial myotome).
Blood Supply and Lymphatics
The ulnar artery is one of the major blood vessels in the upper extremity and is close to the flexor retinaculum. The ulnar artery is a continuation of the brachial artery and is underneath the flexor carpi ulnaris muscle. It lies on top of the flexor retinaculum lateral to the ulnar nerve. The ulnar artery supplies the medial aspect of the forearm and forms the superficial palmar arch providing blood to the hand.[3] In some patients, there is a branch of the ulnar artery that passes over the retinaculum.
Nerves
The flexor retinaculum is best known for sheltering the median nerve in the carpal tunnel. The median nerve originates from the cervical spinal cord roots C5-C7 and C8-T1.[4] These cervical roots merge to form the medial and lateral cords of the brachial plexus, ultimately forming the median nerve. The median nerve then courses down the anterior arm, forearm, and eventually into the hand. While traveling through the forearm between the flexor digitorum superficialis and flexor digitorum profundus, the median nerve passes deep to the flexor retinaculum and through the carpal tunnel.[4] In addition to the median nerve, the ulnar nerve is near the flexor retinaculum. The ulnar nerve, which primarily innervates the intrinsic muscles of the hand, is located superficial to the flexor retinaculum on its medial edge.[5]
Muscles
There are several muscles associated with the flexor retinaculum. Situated deep to the flexor retinaculum are the four tendons of the flexor digitorum superficialis. The flexor digitorum superficialis, which is in the anterior compartment of the forearm, originates at the medial epicondyle of the humerus as well as parts of the radius and ulna. The flexor digitorum superficialis inserts on the base of the second to fifth middle phalanges.[6] The innervation of the flexor digitorum superficialis is the median nerve. The main action of the flexor digitorum superficialis is flexion of the phalanges, primarily at the proximal interphalangeal joints. Deep to the flexor digitorum superficialis is the flexor digitorum profundus. The origin and insertion are the proximal anteromedial surface of the ulna and the distal interphalangeal joints of the phalanges, respectively.[6] The flexor digitorum profundus is innervated medially by the ulnar nerve and laterally by the median nerve. The main action is the flexion of the distal interphalangeal joints, then secondarily flexes proximal interphalangeal joints, metacarpal phalangeal joints, and wrist. Below the flexor retinaculum and lateral to the flexor digitorum superficialis lies the flexor pollicis longus. The origin of the flexor pollicis longus is the middle half of the volar radius, and the insertion is the base of the distal phalanx of the thumb.[6] The innervation of the flexor pollicis longus is a branch of the median nerve, the anterior interosseous nerve.
Physiologic Variants
The main anatomical variations concerning the flexor retinaculum have to do with the median nerve. As previously stated, the median nerve enters the carpal tunnel deep to the flexor retinaculum. A bifid median nerve occurs in some humans, which occurs when the median nerve splits proximally to the flexor retinaculum instead of distally like normal anatomy.[2] Several studies have demonstrated a wide range of variations in the motor branch of the median nerve.[2] These different courses may explain why patients present differently in cases of severe compression of the median nerve.
Surgical Considerations
If conservative management for carpal tunnel does not work, surgical options are available.[1] If the flexor retinaculum is the cause of a patient's carpal tunnel symptoms, surgical release is often necessary. This procedure releases the pressure on the median nerve and can often relieve or eliminate the patient's symptoms. Like any surgery, there are risks involved; knowing the anatomy is key to avoiding damaging any surrounding structures. Because so many vital structures surround the flexor retinaculum, one must be aware of where each tendon, artery, and nerve are relative to the flexor retinaculum.
If the patient suffers from systemic diseases, the recurrence rate after surgery is very high.
Clinical Significance
The flexor retinaculum can entrap and compress the median nerve causing the condition of carpal tunnel.[7] Carpal tunnel is the most common compression neuropathy in the upper extremity. Several causes for compression of the median nerve ranging from repetitive motions, space-occupying lesions, or certain health conditions like diabetes mellitus or hypothyroidism. Clinically patients may present with numbness and tingling in the radial three fingers.[7] Often symptoms are worse at night. Patients may have difficulty holding objects and regularly report dropping items. Clinically patients frequently will have thenar atrophy and weakness. Evaluating sensations in the fingers may show decreased sensation in radial three fingers.[7] Compression of the flexor retinaculum and, therefore, the median nerve may reproduce the patient's symptoms. A classic physical exam maneuver used to diagnose carpal tunnel is the Tinel test. The Tinel test is performed by repeatedly tapping on the flexor retinaculum and seeing if it reproduces the patient's symptoms. Treatments to consider include wrist splinting, work-related ergonomic modification, NSAIDs, steroid injections, and surgical management.
Other Issues
When the retinaculum compresses the underlying nerve, it undergoes a thickening, reducing its elastic capacity. According to a recent study, there is a difference in size between males and females. In women, the retinaculum is smaller; in the female sex, the carpal tunnel syndrome has a higher prevalence.
In carpal tunnel syndrome, in the early stages of the disorder, the proliferation of myofibroblasts seems to play an important role, which not only increases inflammatory responses but reduces tissue elasticity.