Anatomy, Thorax, Mammary Gland
- Article Author:
- Yusuf Khan
- Article Editor:
- Hussain Sajjad
- Updated:
- 7/31/2020 3:18:43 PM
- For CME on this topic:
- Anatomy, Thorax, Mammary Gland CME
- PubMed Link:
- Anatomy, Thorax, Mammary Gland
Introduction
The mammary gland is a highly evolved and specialized organ present in pair, one on each side of the anterior chest wall. The organ's primary function is to secrete milk. Though it is present in both sexes, it is well developed in females and rudimentary in the males. It is also a vital accessory organ of the female reproductive system.
Type: It is an apocrine type of gland. In these glands, the apical part of the cells, along with a part of the cytoplasm, is lost in the secretion.
Situation: The mammary gland is situated in the pectoral region in the superficial fascia. However, a part of it called the axillary tail pierces the deep fascia and lies in the axilla.
Shape: The shape of the mammary gland is hemispherical in young adult females, but becomes pendulous in the later stage of life.
Weight: Though it varies from one person to another, the mammary gland usually weighs between 500 to 1000 grams each.
Extent: The vertical extension of the mammary gland is from the second rib to the sixth rib. The horizontal extension is from the lateral sternal border to the mid-axillary line. A significant part of the organ lies in the superficial fascia. A portion of the breast called axillary tail (of Spence) pierces into the deep fascia and extends to axilla at the level of the third rib.
Deep relations: Deep to the mammary gland tissue is a retro mammary space of loose areolar tissue, which gives free mobility to the mammary gland. Below it is the fascia (pectoral fascia), which covers the pectoralis muscle. Other muscles that lie partly underneath the mammary gland are the serratus anterior muscle and the external oblique muscle of the abdomen.
The study of the mammary gland is best by dividing into four quadrants by a vertical and a horizontal, imaginary line passing through the nipple. The four quadrants are upper lateral, upper medial, lower medial, and lower lateral quadrants.
Structure and Function
Structure:
The structure of the mammary gland is divided into three parts, which include the skin, the parenchyma, and the stroma.
Skin: It consists of a nipple and areola.
- Nipple – It is a conical eminence, present in the fourth intercostal space. 15 to 20 lactiferous ducts pierce the nipple. The nipple contains, circular and longitudinal smooth muscle fibers and is rich in the nerve supply. These smooth muscles help in erecting the nipple upon stimulation. The nipple does not contain any sweat glands, fat, and hairs over it.
- Areola – The dark pinkish-brown pigmented area around the nipple is called the areola. It is rich in modified sebaceous glands (called tubercles of Montgomery in pregnancy and lactation). These glands secrete oily secretion that prevents cracking of the nipple and the areola. Notably, the areola is devoid of fat and hair.
Parenchyma – The glandular tissue of the mammary gland is made up of branching ducts and terminal secretory lobules. There are 15 to 20 lobes, and a lactiferous duct drains each of them. These ducts enlarge to form the lactiferous sinus before they open separately into the nipple. The milk is collected in the lactiferous sinuses and let out on the suckling of the baby. The lactiferous ducts are arranged radially in the nipple. Hence the surgeon needs to take radial incisions to avoid cutting through multiple lactiferous ducts.
Stroma - This is the supporting framework of the breast around the parenchyma.
- Fibrous stroma – This gives rise to septa called suspensory ligaments of Cooper which separates lobes and suspends the mammary gland from the pectoral fascia. In patients with breast cancer, shortening and pulling of these ligaments causes rigidity of the organ and puckering of the skin over it. In association with cutaneous edema, shorting of ligaments give rise to a typical appearance that looks like the peel of an orange. Hence, it is called Peau d' orange appearance.
- Fatty stroma – Even though the nipple and the areola are devoid of fat, the main bulk of the mammary gland is filled with variable amounts of fat.
Till puberty, the development of breasts is minimal and comparable in both the sexes. At puberty, under the influence of spurting estrogen and growth hormones, the breast develops faster in females with a massive development of adipose tissue which gives smooth contour to the breasts. Similarly, in early pregnancy, the breast rapidly increases in size due to the increase in the parenchymal growth and branching in the ductal system. These changes are due to the surge in estrogen, and progesterone hormones. Secretory alveoli start developing at duct terminals and get surrounded by connective tissue. In the later stages of pregnancy, these alveoli are filled with milk under the influence of prolactin. After lactation ends, the secretory alveoli start shrinking and decrease in number and size and subsequently disappear. But the mammary gland never returns to the pre-pubertal stage. In later stages of life, especially after menopause, the breast shows severe regression in size and almost atrophies with a drop in the level of circulating estrogen.
Function:
- The primary purpose is to secrete milk which helps in the breastfeeding of the infants.
- It also plays an essential role in female sexuality.
Embryology
The mammary gland develops from the embryonic Milk Ridge (Milk line) between fourth to the sixth week of intra-uterine life. It is an ectodermal thickening extending from the axilla to the inguinal region. In animals, several mammary glands develop along this ridge, but in the case of the humans, most of the ridge regress and degenerates entirely except for a small part in the pectoral region, which develops as breasts. This area develops into mammary buds and sends off 15 to 20 solid cords. These cords grow in underlying mesenchyme evolving into lactiferous ducts and branches. They later canalize under the influence of maternal sex hormones. The surrounding mesenchyme contributes to the development of fibrous connective tissue and fat. The ectoderm thickens to form nipple and areola.
Congenital Anomalies:
- Ectopic breast - Ectopic breasts present when the mammary gland develops away from its usual site. Its presentation is usually in the chest (other than the regular site), axilla, abdomen, and sometimes even in the vulva.
- Polymastia - A condition where the female presents with more than one breast on each side.
- Polythelia – In this condition, a single breast will have multiple nipples, usually numbering 2 or 3. Often, one of them is functional, and others are rudimentary. Polymastia and polythelia combined occur in almost 0.2% to 5.6% of women.
- Micromastia – In this condition, the mammary gland fails to proliferate and remains small.
- Macromastia – It is a condition where the mammary gland grows much more than the usual size and hypertrophies.
- Gynecomastia – Although the mammary glands are rudimentary in males, in certain conditions, they enlarge to look like a female breast. This condition is known as gynecomastia. Though large, they are non-functional. In the case of Klinefelter syndrome, approximately 80% of patients have gynecomastia.
- Retracted nipple or inverted nipple – This is because of the failure or incomplete development of the nipples.
The most common congenital anomaly of all the above is the ectopic breast. Ectopic breasts usually are seen over the milk line, but in some cases, they can also occur away from the ridge, such as the face, ear, neck, buttocks, knee, lateral thigh, etc.[1][2]
Blood Supply and Lymphatics
Arterial Supply:
Mammary glands are extremely vascular organs. The main arterial supply of the mammary glands is by the following five arteries on each side.
- Perforating branches of Internal thoracic artery coming from the second to the sixth intercostal spaces.
- Lateral thoracic artery
- Superior thoracic artery
- Acromio-thoracic artery
- Lateral branches of posterior intercostal artery
Among the above arteries, the lateral thoracic, the superior thoracic, and the acromiothoracic arteries are the branches coming directly from the axillary artery.
Venous drainage:
Veins that drain the mammary glands follow the arteries in their course and adopt their names.
These veins form an anastomotic venous circle around the nipple which divides into superficial and deep sets
- Superficial veins drain into internal thoracic and superficial veins of the lower neck
- Deep veins drain into internal thoracic, axillary and posterior intercostal veins
Importance: Carcinoma of the breast may spread through deep veins into the Batson plexus of veins that are around the vertebral column. These veins are valveless, allowing a bidirectional flow of venous blood and communicate with the internal vertebral plexus of the veins. Thus metastasis of the carcinoma from the breast can quickly spread to the vertebral column and in turn, to the spinal cord.[3] It can also lead to the collapse of the vertebral bodies, which can injure the spinal cord and thus paresthesia/paralysis of the body below the lesion.
Lymphatic drainage:
Principal lymph nodes: The primary site of lymphatic drainage of the breast is to the following group of lymph nodes.
- Axillary nodes: The axillary group of lymph nodes classifies into the following five groups. They are present in the axillary pad of fat.
- Anterior (Pectoral) group: This group of lymph nodes lies on the lower border of pectoralis minor along the lateral thoracic vessels and drains outer quadrants of the breast.
- Posterior (subscapular) group: This group lies on the posterior wall of the axilla along the lower border of the subscapularis. It drains the lower outer quadrant of the breast
- Lateral group: This group of lymph nodes lies over the lateral wall of axilla besides the humerus and drains a minimal quantity of lymph from the breast.
- Central group: This group lies in the base of the axilla and receives lymph from the anterior, posterior and lateral groups of lymph nodes
- Apical groups: This group of lymph nodes lies deep in the apex of the axilla and receives lymph from all the above groups of lymph nodes. It also directly drains the upper medial quadrant of the breast.
- Internal mammary (parasternal) nodes: These groups of lymph nodes are beside the lateral border of the sternum surrounding the internal mammary artery and drain the medial quadrants of the breast. Some cross to the other side and drain to the opposite group of parasternal nodes; this is precisely the route by which metastasis from one breast (ipsilateral) spreads to the other side and becomes bilateral.
The axillary group of lymph nodes is the primary group of lymph nodes that drain the lymph from the breasts. The axillary group drains almost 75% to 80% of lymph from breasts. Among these, the anterior group is the leading site of drainage. The internal mammary group drains the remaining 20 to 25% of lymph from the breasts.
Other lymph nodes: The other locations where the breast drains a small amount of lymph are as follows.
- Supraclavicular nodes
- Cephalic (deltopectoral) nodes
- Posterior intercostal nodes
- Subdiaphragmatic & subperitoneal lymph plexuses: This is the route by which the metastasis from the breast spreads to the abdomen.
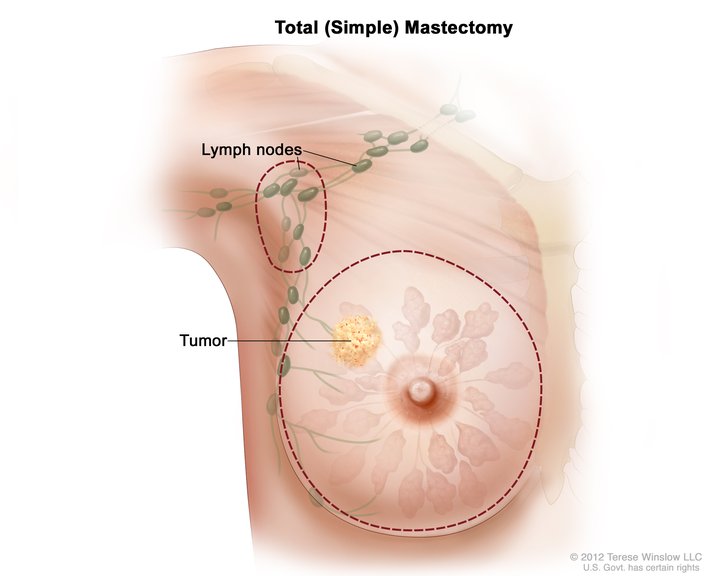
Clinical Importance: Usually, malignancy of the breast metastasizes through the lymphatics, and hence the surgeons need to have complete knowledge of the lymphatic drainage of the mammary gland; this will allow the appropriate removal of lymph nodes during surgical removal of malignant tumors from the breast in case of a radical mastectomy.[4]
Nerves
Vast differences have been reported in the literature about the nerve distribution to the breast tissue, especially with regards to areola and nipple. However, the majority agrees to the fact that the mammary gland receives innervation by anterior and lateral cutaneous branches coming from the second to sixth intercostal nerves and also from the supraclavicular nerves. They form a plexus underneath the areola in the subdermal tissue and supply the nipple and the areola.[5][6] The nipple and areola are highly sensitive to touch, and these sensations are carried mainly by the T4 spinal nerve dermatome.
In the case of surgical reconstruction of the breast, it is essential to preserve the nipple and areola along with its innervation. Hence lots of studies have been done in recent times to understand the nerve supply of the breast, especially concerning nipple and areola.[7][8][9]
Muscles
The mammary gland is said to be a modified sweat gland made up of the parenchyma and the stroma covered by the skin. Underlying this gland are some muscles. The primary muscle, which lies deep underneath this gland is the pectoralis major muscle covered by pectoral fascia. Other muscles that are partly underneath this gland along with the pectoralis major muscle are the serratus anterior muscle and the external oblique muscle of the abdomen.
An intact pectoralis major muscle plays a crucial role in the successful reconstruction of the breast and implant surgeries.[10][11] Surgeons have tried flaps from many different muscles for the restoration of the breasts, but the most successful one has been from the latissimus dorsi muscle.[12][13]
Physiologic Variants
Mammary gland shows physiological variations quite commonly in size, shape, contour, density, spacing, volume, etc. These variations depend upon several factors like age, height, weight, genetic composition, race, nourishment, built, environment, etc. In some females, they are massive while quite small in size in others. In 25% of the females, there is an observable asymmetry in the size and shape of breasts of the same person.
Inversion of the nipples is also quite frequently seen in females, which can be physiological and corrects itself or with slight manipulations during the first pregnancy. But sometimes, it is also an early indicator of underlying pathology.
The mammary glands can also present with multiple breasts or nipples. Some of these were already mentioned under the section covering congenital anomalies.
Surgical Considerations
Surgery is the treatment of choice for lesions of the breast, ranging from lumpectomy to radical mastectomy. As mentioned earlier, malignancy of the breast metastasizes through lymphatics. Hence, the knowledge of lymphatic drainage of the mammary gland is essential for surgeons. Accordingly, all the lymph nodes draining the breasts can be identified and removed during surgical removal of malignant tumors from the breast through radical mastectomy surgeries.
In the case of malignancy, recurrence is quite frequent, and hence adjuvant radiotherapy is necessary to reduce local recurrence. Patients with a higher risk of recurrence also receive adjuvant chemotherapy, which gives the patients a longer disease-free overall survival period. Hormonal therapy is useful in certain conditions where tumors are estrogen and progesterone receptor-positive. Estrogen positive patients who receive adjuvant hormonal therapy with tamoxifen have demonstrated to do very well after treatment.
With a global increase in the carcinoma of the breast, there is a surge in the surgical mastectomy, with a concurrent increase in the demand for surgical reconstructions of the breast, breast implants, and mammaplasty.[14][15] This trend has led to the innovation of new methods of surgical interventions and breast implants, as well as promoting a keen interest in understanding the overall anatomy of the chest wall, its innervation, and vascularity.[16][17][18]
Clinical Significance
Breast cancer is the most common malignancy after lung cancer worldwide and a leading cause of cancer-related deaths among women.[19][20][19] Hence, it has attained full attention among the scientific community and a significant cause of concern among females. Research has observed that the outer upper quadrant of the breast is the most common site for the development of carcinoma of the breast, as seen in almost 60% of the cases.[21]
There are two broader divisions of breast lesions, namely, benign and malignant. Though the benign lesions of the breast are much more prevalent, they gain much less attention as they are usually non-fatal.[1] Fibrocystic changes are widespread among benign non-neoplastic lesions. They constitute almost 40% of all the lesions of the breasts, especially at the premenopausal age. Fibrocystic changes categorize into two types; the proliferative and the nonproliferative. The examples for nonproliferative are cystic and fibrotic changes and proliferative like epithelial hyperplasia and sclerosing adenosis.
Among the neoplastic lesions, the most common of the benign neoplasm is the fibroadenoma. It constitutes almost 7% of all the lesions of the breast. These are quite common among young females. They tend to develop under the influence of estrogen and hence seen more during the pregnancy and late menstrual cycles. They regress and calcify after menopause. The other common types of benign neoplasms are phyllodes tumor and intraductal papilloma.
Some of the risk factors are; age above 40 years, nulliparous, delayed first pregnancy, use of oral contraceptives, obesity, high-fat diet, family history, genetic factors, alcohol consumption, cigarette smoking, and ionizing radiations. It is observed to be more common in the Western world and Afro-American females compared to Asians and Africans.[22][23] Neoplastic lesions divide into two types, noninvasive like ductal carcinoma in situ (DCIS), also known as the Paget disease of the nipple, and lobular carcinoma in situ (LCIS). The invasive (infiltrative) carcinomas are invasive ductal carcinoma, invasive lobular carcinoma, medullary carcinoma, colloid carcinoma, tubular carcinoma, etc. Invasive ductal carcinoma is quite common, accounting for 70%. Prognosis in females with carcinoma of the breast depends on the size of the tumor, the involvement of the lymph nodes, tumor grading, metastasis, and structural features.[20]
In diagnosing and analyzing breast carcinoma, the clinician needs to remember that it is confined to females alone but can also manifest in males.[24]
Screening is one of the best methods for early detection of the lesions of the mammary gland. Screening of breast is generally by mammography, infrared breast thermography, etc.[25] However, research shows that mammography done before 40 years of age is not useful in detecting carcinoma of the breast, and therefore, it is not a recommendation at an early age.[26][27][26] Confirmation of the lesions is done usually by MRI, ultrasound, and needle biopsy.
Other Issues
Even though tuberculosis of the mammary gland is said to be rare, its incidence in developed countries is estimated to be almost 0.1% of all breast lesions.[28] A rare neoplasm that can appear in the mammary gland is the myoepithelioma, which is diagnosed mainly by immunohistochemical and histological features.[29]
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)