Anatomy, Abdomen and Pelvis, Internal Iliac Arteries
- Article Author:
- Nicolas Zaunbrecher
- Article Editor:
- Navdeep Samra
- Updated:
- 8/22/2020 7:19:23 PM
- For CME on this topic:
- Anatomy, Abdomen and Pelvis, Internal Iliac Arteries CME
- PubMed Link:
- Anatomy, Abdomen and Pelvis, Internal Iliac Arteries
Introduction
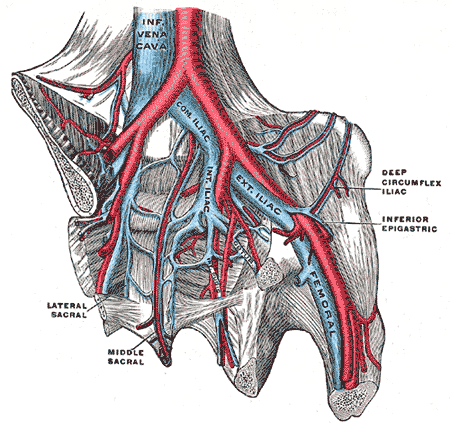
Before discussing the blood supply to the pelvis, one must first know the origin of the larger vessels located upstream. The abdominal aorta travels toward the pelvis and bifurcates into the common iliac arteries which subsequently bifurcate into the internal and external iliac arteries. The internal iliac arteries (IIA) supply the majority of the pelvis and the structures within, and the external iliac artery continues down to supply the lower extremities. The arteries within the pelvis can have numerous variations and these become important during surgery within the pelvis.
Structure and Function
The abdominal aorta bifurcates at the fourth-fifth lumbar vertebra into the right and left common iliac arteries. After about 3 to 4 cm, the common iliac arteries will bifurcate again anterior to the sacroiliac joint, and they become the internal and external iliac arteries.[1][2] The internal iliac artery after the pelvic brim continues down inferomedially and has two parts which split at the upper margin of the greater sciatic foramen into the anterior trunk which supplies the pelvis, visceral organs, and posterior trunk which supplies the parietal structures.[1][2] The origin of the anterior division begins about 2.5-3.5 cm from where the IIA begins, and the posterior branch of IIA takes off before the anterior division.[2]
Embryology
In embryonic development, the cardiovascular system is the first major system to function in the embryo due to the necessity of having an adequate transport vessel for the delivery of oxygen to the growing cells. In the middle of the third week of embryonic development, the primordial heart and vascular system appear. The common iliac arteries bifurcate into internal and external iliac arteries at L5-S1 in adults.[3] In the 1st trimester the bifurcation level is at S1, but at full term, the location of most of the bifurcations is at L5, indicating that in the early fetal period the bifurcation level of the common iliac artery is more inferior compared to adults.[3] During fetal development, the internal iliac artery derives from the umbilical artery. The proximal aspect of the umbilical artery persists throughout development, but the distal end gets obliterated postnatally. Numerous variations can occur in a vascular pattern of the IIA.[4]
Blood Supply and Lymphatics
In general, the IIA supplies the pelvic wall, pelvic viscera, perineum, and the gluteal region. The internal iliac artery (IIA) starts at the level of the sacroiliac joint once the common iliac artery divides into the external and internal iliac branches. The internal iliac artery then divides again near the upper border of the greater sciatic foramen into an anterior and posterior division. The anterior division branches are the superior vesical, obturator, middle rectal, inferior vesical artery and internal pudendal artery. In females, the inferior vesical artery is replaced by the vaginal artery and gives an additional branch which is the uterine artery. Posterior division branches are iliolumbar, lateral sacral, and superior gluteal arteries. Among the various arteries that come from the internal iliac artery, many anomalies can occur.[4]
Extra-pelvic branches of the internal iliac artery supply regions of the thigh located anteromedial and posterior, hip joint, and gluteal region.[5]
Visceral branches of the internal iliac artery in a man supply:
- Rectum
- Urinary bladder
- Seminal vesicles
- Ejaculatory ducts
Visceral branches of the internal iliac artery in a female supply:
- Vagina
- Uterus
- Gonads
- Rectum
- Urinary bladder
- Urethra[5]
The organs that the lymphatic system drains in the pelvis is the digestive tract, urinary organs, and genital organs. These organs have afferent lymph vessels that flow towards the nodes, and once it reaches the nodes, efferent vessels arise and take the lymphatic fluid to lymphatic collectors located superior to the nodes.[6] The lymph nodes and lymphatic vessels travel along the common iliac artery, the internal iliac artery, and external iliac artery.[6]
Muscles
The internal iliac artery supplies the gluteal muscles, pelvic viscera, perineum, and pelvic walls. The anterior division is more involved with territorial blood supply to the pelvic viscera, and the posterior division provides blood flow to the gluteal region and body wall.[4]
Physiologic Variants
One must be aware of the several types of anatomical variations that may present during a surgical procedure. The first significant variance is that the internal iliac artery origin varies and depends on several factors such as the length of the common iliac artery and when the internal iliac artery bifurcates. It can be at the level of the L5-S1 and S1 intervertebral disk and anterior to the sacroiliac joint.[4]
The obturator artery (OA) can arise from:
- the posterior branch of the internal iliac artery
- the inferior epigastric artery
- the inferior vesical artery
Iliolumbar artery can come directly from the trunk of the internal iliac artery.[4]
Surgical Considerations
- When accessing the internal iliac artery in a female one must cut the pelvic peritoneum which is continuous with the broad ligament to visualize the retroperitoneal area. In the retroperitoneum, the internal iliac artery and the other great vessels of the abdomen are visible.[1]
- Two vessels that can give some blood supply to the femoral head is the piriformis branch of the inferior gluteal artery and the obturator artery via the foveal artery. Many anatomical variations occur with the obturator artery with the most common one being the corona mortis (crown of death).[7]
- The corona mortis is an anastomotic branch between the inferior epigastric and obturator vessels in the obturator canal. The other variation involves an accessory obturator artery arising from the external iliac artery and forming a connection with the obturator artery coming off of the internal iliac artery. The accessory OA can traverse over the superior pubic ramus creating a risk of injury during mesh attachment for hernia repair.[8] Another significance of the corona mortis during surgery is that compression of the internal iliac will not wholly stop bleeding from this anomalous artery since it is also receiving blood flow from the external iliac artery. However, compression of the internal iliac artery can still be used to control the contribution of blood flow that is coming from the IIA to the corona mortis.[9]
- During surgery in the pelvis, another critical vessel to be mindful of is the location of the ureter which is located at the medial aspect of the internal iliac artery. The space between the ureter and the IIA is known as the para-rectal space. During a hysterectomy, the surgeon needs to be mindful when ligating the uterine artery (a branch of IIA) because the ureter passes beneath this artery and is at risk for injury.[1]
- It is essential to attempt to ligate the internal iliac artery distal to the posterior branch. Experience shows that proximal ligation of the internal iliac artery can result in claudication of buttocks and also necrosis.[4]
Clinical Significance
In acute situations involving the pelvic region knowledge of the level of the bifurcation of the common iliac artery and the level of division of the internal iliac artery is of paramount importance. Unilateral or bilateral ligation of the internal iliac artery can be lifesaving in a variety of patients, such as massive postpartum hemorrhage, hemorrhage after a vaginal and abdominal hysterectomy, massive broad ligament hematoma, cervical carcinoma, and retroperitoneal bleeding following a pelvic fracture.[4]
When trying to control a bleed in the pelvis, bilateral ligation of the internal iliac arteries will reduce the pelvic arterial blood flow by 49%. Collateral arterial circulation will make up for the blood that was previously being supplied by the internal iliac artery. The main artery that collateral circulation comes from is the deep femoral artery. [2] Various anastomoses aid in re-vascularizing the internal iliac artery area such as superior gluteal artery and lateral femoral circumflex artery, obturator artery and medial femoral circumflex artery. In females, blood flow to the uterus via the ovarian artery and after bilateral internal iliac artery ligation reproduction potential is not affected, and it is still possible to have term pregnancies in many cases.[2]
Knowing the anatomical course of the ureter is vital because during acute situations to control hemorrhage damage to the ureter can occur. The ureter which is usually laying on the surface of the internal iliac artery requires identification before ligation performed.[4]
An anomalous origin of the obturator artery from the posterior division becomes vital because if damage occurs to the anterior branch of the internal iliac artery the blood supply to the head of the femur would not be affected.[4]