Anatomy, Abdomen and Pelvis, Femoral Sheath
- Article Author:
- Navid Mahabadi
- Article Author:
- Valerie Lew
- Article Editor:
- Michael Kang
- Updated:
- 7/10/2020 9:31:00 AM
- For CME on this topic:
- Anatomy, Abdomen and Pelvis, Femoral Sheath CME
- PubMed Link:
- Anatomy, Abdomen and Pelvis, Femoral Sheath
Introduction
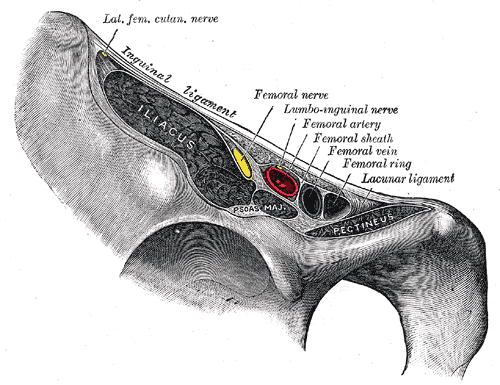
The femoral sheath is a structure within bilateral femoral triangles. The femoral sheath contains the femoral vein, artery, and lymphatics. The femoral nerve lies lateral to the femoral sheath and is not enclosed within the sheath.[1][2]
Anatomy
The femoral sheath attaches superiorly to the inguinal and lacunar ligaments and resides completely in the thigh. The femoral sheath is funnel-shaped, blending distally into the vessels adventitia. The upper end of the femoral sheath lies at the low inguinal level, where the lacunar ligament attaches to the pectineus muscle fascia 1 cm to 1.5 cm below Cooper’s ligament. Also at this low inguinal level lies the inguinal ligament and transversalis fascia (floor of the femoral canal). The inguinal ligament attaches to the upper end of the anterior wall of the femoral sheath.
The three walls of the femoral sheath include:
- The posterior wall is formed by the iliaca fascia, along with a narrow ribbon of pectineus muscle fascia.
- The anterior wall is formed by the transversalis fascia and partially the fascia lata.
- The lacunar ligament forms the medial wall. The transversalis fascia moves laterally from the floor of the femoral canal toward the upper end of the venous compartment forming the medial wall.
Two additional coverings of the sheath include the fascia lata that descends from the inguinal ligament, in front of the femoral sheath, to cover and blend with transversalis fascia of the anterior wall. Scarpa’s fascia covers the femoral sheath superior to that.
The three compartments of the femoral sheath include:
- The lateral compartment, which contains the femoral artery and femoral branch of genitofemoral nerve.
- The middle compartment, which contains the femoral vein.
- The medial compartment, where the femoral canal and lymphatics course through.
The femoral canal (the opening is called the femoral ring) is the most medial portion of the femoral sheath. The femoral canal connects the pelvic cavity to the anteromedial aspect of the thigh. The four borders of the femoral canal include the femoral vein laterally, lacunar ligament medially, inguinal ligament anteriorly, and pectineal ligament posteriorly. Fatty tissue and lymph nodes course through the canal.
Lateral to the femoral sheath is a muscular lacuna, bordered by the inguinal ligament, innominate bones anterior edge, and iliopectineal arch. The femoral nerve and iliopsoas muscle pass through this muscular lacuna.
Structure and Function
The femoral sheath allows for flexible compartments to ensure blood flow continues despite certain movements and increased demands. The femoral canal sits medial to the femoral vein, allowing the femoral vein to increase in size when there is increased venous return (such as in Valsalva). Additionally, the femoral sheath allows vessel mobility during hip flexion.[3]
Blood Supply and Lymphatics
The femoral vein is a thin-walled vessel with a lumen up to 1.5 cm diameter.
The femoral artery is a thick-walled vessel with a lumen less than half that of the vein. This artery lies lateral to the femoral vein.
The common iliac arteries (left and right) bifurcate off the aorta around the L4 level. The common iliac artery bifurcates into the internal and external iliac arteries. As the external iliac artery courses under the inguinal ligament, it becomes the common femoral artery, bifurcating into the superficial and deep femoral artery. Five percent of the time, the lateral femoral circumflex artery (LCFA) branches off the common femoral artery, while 95% of the time, the LCFA branches off the deep femoral artery. The medial circumflex femoral artery also branches off the common femoral artery, supplying the head of the femur. The profunda femoris artery has small vessels that supply the femur shaft.
The femoral canal contains the deep inguinal node of Cloquet, which drains fatty connective tissue, the clitoris, and penis.
Nerves
The femoral branch of the genitofemoral nerve courses through the lateral compartment of the femoral sheath and pierces the anterior surface of the sheath. This nerve innervates the skin of the anterior thigh, just above the femoral sheath.
The femoral nerve sits lateral to the femoral sheath and does not lie within the sheath.
Muscles
The iliacus, psoas major and pectineus muscles run posterior to the femoral sheath. The psoas major muscle runs posterior to the iliacus and pectineus muscle, thus, does not form the posterior wall of the femoral sheath.
Surgical Considerations
In cases of inguinal lymphadenectomy, it is important to preserve the muscular fascia, especially the femoral sheath components such as the fascia lata. This is to ensure the valves of the femoral vein and lymphatics can continue functioning by pumping blood and lymph drainage toward the heart. This can also prevent lymphadenopathy.[4]
Clinical Significance
Femoral hernias comprise 5% to 10% of groin hernias in adults. Elderly females are predisposed to femoral hernias because of the wider pelvis anatomy and loss of fatty tissue in the femoral canal with increasing age. The incidence of femoral hernias in pediatrics is 0.5%. Weakness at the fascial attachments of the upper end of the femoral sheath can allow protrusion of pre-peritoneal fat, omentum, small bowel or other visceral structures. These protrusions can break through the transversalis fascia floor of the femoral canal, emerging through a circular fascial opening and forming a femoral hernia. This opening may begin as only 1 cm in diameter, but expand if not treated properly. Smaller fascial openings may lead to increased risk of an incarcerated femoral hernia (intestines are stuck but still has blood flow) or even strangulation (intestines are stuck with the loss of blood flow). There are multiple locations a femoral hernia can present within the femoral sheath. The femoral type hernia is most common, occurring 98.5% of the time and is easiest to repair. The perivascular Velpeau’s hernia and Scrafeu’s hernia are rare and difficult to repair.[5]
The femoral vein is a relatively safe option for gaining central venous access when more proximal locations are less easily accessible. Ultrasound guidance helps reduce vascular bleeding by 60% when used for femoral vein cannulation. Routine use of ultrasound is not recommended for femoral vein cannulation as there are rare fatal complications as opposed to jugular or subclavian approaches. Also, the anatomical location of the femoral vein is fairly constant, allowing palpation of the femoral artery to be a fairly reliable technique. However, central venous catheter infection risks are increased with femoral vein catheters as opposed to subclavian approach.