Anatomy, Thorax, Subclavian Veins
- Article Author:
- Sara Capobianco
- Article Author:
- Michael Fahmy
- Article Editor:
- Vincent Sicari
- Updated:
- 8/16/2020 2:49:10 AM
- For CME on this topic:
- Anatomy, Thorax, Subclavian Veins CME
- PubMed Link:
- Anatomy, Thorax, Subclavian Veins
Introduction
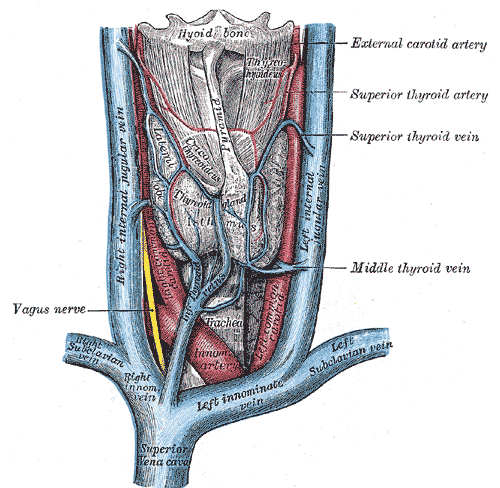
The subclavian vein (SVC) is classified as a deep vein and is the major venous channel that drains the upper extremities. Other deep veins of the upper extremity that accompany the major arteries include the radial, ulnar, brachial, axillary veins. The SVC is a paired deep vein in the normal variant of human anatomy, the left subclavian vein, and right subclavian vein, arising as a continuation of the axillary vein at the lateral border of the first rib on each upper extremity and continues to pass over the first rib in its groove on the rib. The subclavian artery is just posterior to the subclavian vein. The subclavian vein continues its path posterior to the clavicle, toward the sternal notch until the medial border of the anterior scalene muscle behind the sternoclavicular joint. Here, it joins the internal jugular vein, which becomes the brachiocephalic vein (also known as the innominate vein), to enter the superior vena cava, which drains into the right atrium of the heart.
Structure and Function
The subclavian veins are valveless, and the anatomical path of the right and left subclavian veins are not symmetrical. The right subclavian vein forms an angled arc as it merges with the right internal jugular vein, to form the right brachiocephalic vein to enter the superior vena cava. The left subclavian vein is located posterior to the clavicle after crossing the first rib; this region is the only area where the subclavian vein directly is in communication with the clavicle. The subclavian veins both end by joining the internal jugular veins to form the brachiocephalic veins. The angle at which both meets is termed the venous angle. The right subclavian vein is joined by the right lymphatic duct at the right venous angle, which drains lymph from the right upper quadrant of the body (right side of the head, neck, thorax, right upper extremity). The left subclavian vein is joined by the lymphatic duct at the left venous angle, which drains the rest of the body's lymph fluid. The subclavian veins carry deoxygenated venous blood from the axillary vein to the brachiocephalic vein to ultimately return to the right atrium.[1][2][3][4]
Embryology
The subclavian veins are developed in the fourth week of human embryologic development, with the outgrowth of the fore-limb buds. The subclavian veins open into the primitive jugular veins.
Blood Supply and Lymphatics
The subclavian veins are the major venous channel draining the upper extremity, arising from the axillary veins. The deep lymphatic vessels of the upper extremity follow the major deep veins, terminating in the humeral axillary lymph nodes, which function to drain lymphatic fluid from the upper limb's joint capsules, periosteum, tendons, and musculature. The efferent vessels from the apical axillary nodes travel through the cervicoaxillary canal before converging to form the subclavian lymphatic trunk. The left subclavian trunk directly drains into the thoracic duct, and the right subclavian trunk continues to form the right lymphatic duct, which enters at the right venous angle (junction of the internal jugular vein and subclavian vein).
Nerves
Nerves and Muscles
In the normal human anatomy, the phrenic nerve (C3-C5) is located posterior to the subclavian vein. The phrenic nerve passes anterior to the anterior scalene muscle and then courses posterior to the subclavian vein, and anterior to the internal thoracic artery as it enters the thorax to run anterior to the root of the lung and between the fibrous pericardium and mediastinal surface of the parietal pleura. Medial to the subclavian vein is the brachiocephalic trunk, thoracic duct, trachea, and vagal trunks. Lateral to the subclavian vein is the inferior trunk of the brachial plexus. The subclavius muscle and subclavian vein are also closely adherent, with the subclavius muscle lying anterior to the subclavian vein. The subclavius muscle is a small, triangular muscle originating from the first rib and inserting on the inferior surface of the lateral clavicle. The brachial plexus, subclavian artery, and subclavian vein pass below the subclavius muscle.[5][6]
Physiologic Variants
There are anatomical variants of the subclavian vein. The subclavian vein may run on a higher plane than usual, sometimes lying above the subclavian artery. The subclavian vein may also pass with the subclavian artery posterior to the anterior scalene muscle or can run behind the anterior scalene muscle with the subclavian artery anterior to the muscle. The subclavian vein may also split, forming a venous circle surrounding the clavicle, anterior scalene, and/or phrenic nerve, termed a "clavicular loop." Occasionally, the subclavian vein can pass between the clavicle and the subclavius muscle. A rare anatomical variant of the phrenic nerve crossing anterior to the subclavian vein, or the phrenic nerve traversing the anterior wall of the subclavian vein, can be present which could potentially cause phrenic nerve injury during subclavian vein catheterization.
Surgical Considerations
The right and left subclavian veins are often used for central line placement to access the venous system. Central lines are inserted to administer parenteral fluids and medications, and can also be used to measure the central venous pressure. Indications for a central line include hemodynamic instability, the necessity of hyperosmolar agents, and inadequate peripheral IV access. The most common techniques involve the infraclavicular (IC) approach. To perform an infraclavicular subclavian vein central line placement, the patient should be positioned in a Trendelenburg position, with slightly extended shoulders. The proceduralist places the thumb of one hand on the middle part of the clavicle and the index finger on the jugular notch of the patient's manubrium. The needle should enter the skin inferior to the thumb, 1-cm lateral to the curvature of the middle third of the clavicle, with the needle pointing horizontally directed at the sternal notch. The needle is advanced medially toward the tip of the administrator's index finger until the tip of the needle enters the right venous angle posterior the sternoclavicular joint. It is important to ensure that the bevel of the needle is directed towards the SVC; a sterile finger can be placed in the ipsilateral supraclavicular fossa. The other method of subclavian central line placement is in a supraclavicular approach, in which the site of the puncture is the claviculo-sternocleidomastoid angle, just superior to the clavicle and lateral to the insertion of the clavicular head of the sternocleidomastoid muscle. The needle should be advanced toward the contralateral nipple, just inferior to the clavicle. Of anatomic note, the dome of the right lung is located in a lower position than the left lung which may extend above the first rib. If the needle is not inserted correctly, it may puncture the patient's pleural lining and lung resulting in a pneumothorax. If the needle is inserted too far posteriorly, it may enter the subclavian artery instead of the subclavian vein. Other complications of this procedure include hemothorax, chylothorax, catheter malposition, bleeding, infection, arrhythmia, air embolism, nerve injury, catheter malposition, and venous thrombosis.[7][8]
Clinical Significance
Stenosis
Subclavian vein stenosis is a narrowing of the subclavian vein, presenting with variable symptoms ranging from asymptomatic, to arm swelling, pain, paresthesia, neck pain, or an occipital headache. Stenosis of the subclavian vein can arise from many intrinsic or extrinsic causes and can be further complicated by the development of a deep vein thrombosis (DVT) (see below). Intrinsic causes of stenosis include previous intravenous catheterization, such as hemodialysis catheters, central venous catheters, or hemodialysis-related subclavian vein stenosis from intimal hyperplasia secondary to an increase in turbulent blood flow from a created arteriovenous fistula. Extrinsic causes of stenosis include entrapment between the clavicle and first rib (costoclavicular space), termed costoclavicular syndrome, Paget-Schrotter syndrome (PSS), regional tumors, lymphadenopathy, trauma, or mediastinal inflammatory pseudotumor. Costoclavicular syndrome is one of the three types of thoracic outlet syndrome and is the most common site for subclavian vein compression. It can be caused by depression of the clavicle toward the first rib, a tight subclavius muscle, congenital anomalies in the thoracic outlet, trauma, or tight clothing/straps over the area. This condition is characterized by spontaneous swelling of the entire arm, often with cyanotic discoloration, heaviness, and pain. Unilateral upper extremity swelling caused by subclavian vein obstruction without an underlying thrombosis is an uncommon form of thoracic outlet syndrome and should be considered in the patient with unilateral arm swelling in the setting of no lymphatic obstruction. Diagnosis is made with contrast venography, and plain radiography of the neck and chest with the cervical spine or thoracic inlet views can help demonstrate bony abnormalities that can aid in the diagnosis. Treatment depends on the severity of symptoms and physical examination, but conservative treatment with anticoagulation and extremity elevation often results in chronic venous congestion. Therefore, depending on the clinical scenario and presence or absence of an underlying thrombosis in addition to the venous stenosis, surgical thoracic outlet decompression and/or catheter-based thrombolytic therapy are the mainstay of treatment. Surgical treatment comprises trans axillary or para-clavicular first-rib resection, with potential balloon angioplasty or direct venous reconstruction if there is a residual subclavian vein obstruction.[9]
Deep Vein Thrombosis
With the increased use of central venous catheters, DVT of the upper extremities are becoming more prevalent, especially involving the subclavian, brachial, and axillary veins. There is an incidence of about 5% to 10% of upper extremity DVT's out of all DVT's, with the incidence rising each year. There are two subsets of upper extremity DVT's: primary and secondary. The primary DVT subset is known as Paget-Schretter syndrome (PSS) and most typically occurs in the dominant upper extremity of young athletes that perform excessive and repeated motions of the upper extremity (gymnastics, wrestling, swimming, sports that require repetitive ball throwing such as football, baseball, basketball). The secondary subset commonly occurs in patients with central venous catheterization in place or patients with an underlying malignancy. The rate of upper extremity DVT in patients with central venous catheters are about 14% to 23%, and pulmonary embolisms arise in up to 6% of all DVTs affecting the upper extremities. In PSS, the repetitive motions of the upper extremity result in hypertrophy of the scalene muscles, which leads to compression of the neurovascular bundle as it exits the thorax between the cervical rib and musculature. Repetitive compression of the subclavian vein over time leads to venous stasis, microtrauma of the vein activating the intrinsic coagulation pathway, setting up for thrombosis. In the secondary form, the catheterization itself disrupts the endothelial lining, activating the intrinsic coagulation pathway. Most patients with an upper extremity DVT will present with limb swelling, arm discomfort, or arm heaviness. A patient with an upper extremity DVT resulting in a PE may also present with cardinal signs of PE including but not limited to tachycardia, chest pain, or shortness of breath. The physical examination may also show erythema in the upper extremity with visible veins across the chest and upper limb (Urschel's sign). In PSS, patients often will present with more sudden onset of severe limb pain and swelling in the dominant arm. Assessment of the distal pulses bilaterally is important. Limbs that appear pale, cool, or mottled are at an increased risk for limb ischemia. Documentation of any motor or sensory defects is also important components of the physical exam. Diagnosis is confirmed with compression duplex ultrasonography, which has a sensitivity of 97% and a specificity of 96% in diagnosing DVT in the upper extremity and is the gold standard in imaging diagnosis. Magnetic resonance and computed tomographic venography are superior to ultrasonography in diagnosis. However, their clinical utility can be limited by cost, radiation exposure, and/or availability in the facility. In patients suspected of having an underlying hypercoagulable condition, coagulation assays can be ordered. In patients with a low clinical suspicion of DVT, a d-dimer test can rule-out the diagnosis. The treatment of the DVT depends on the clinical scenario and patient. If the patient has a central venous catheter in place, the American College of Chest Physicians recommends the provider determining the necessity of the line, and if it is required, it should remain in place, and anticoagulation therapy should begin. If the catheter is not needed, the patient can undergo removal of the catheter after 3 to 5 days of anticoagulation therapy. Each patient should continue on warfarin for 3 to 6 months after diagnosis and initial bridging with heparin. In PSS, often urgent surgical intervention is needed in the setting of acute thrombosis.[10][11][12]