Anatomy, Head and Neck, Lingual Nerve
- Article Author:
- Sarah Fagan
- Article Editor:
- William Roy
- Updated:
- 8/24/2020 10:48:24 PM
- For CME on this topic:
- Anatomy, Head and Neck, Lingual Nerve CME
- PubMed Link:
- Anatomy, Head and Neck, Lingual Nerve
Introduction
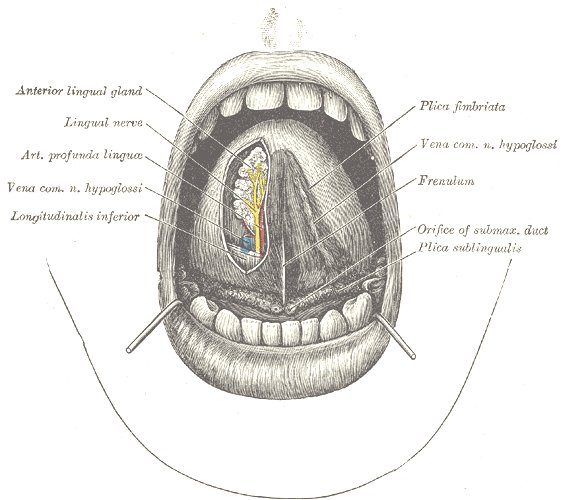
The lingual nerve branches from the mandibular division of the trigeminal nerve. The lingual nerve is often in a common stem with the inferior alveolar nerve after the mandibular division enters the infratemporal fossa through foramen ovale.[1] The lingual nerve separates from the inferior alveolar nerve and then descends anteriorly into the oral cavity. As it does so, it innervates the mucous membrane of the anterior two-thirds of the tongue, the floor of the oral cavity, and the adjacent gum (lingual gingiva).[2]
Structure and Function
After branching from the mandibular nerve high in the infratemporal fossa, the lingual nerve passes between the tensor veli palatini and lateral pterygoid muscles. It then emerges from between the lateral and medial pterygoid muscles anterior to the inferior alveolar nerve.[3] The nerve passes between the lateral surface of the medial pterygoid muscle and the mandibular ramus en route to the oral cavity. As it courses anteriorly adjacent to the mandible, the lingual nerve gives innervation to several structures, including the mandibular gum (gingiva), the mucous membrane of the anterior two-thirds of the tongue, and the floor of the mouth.[4] The nerve loops under the submandibular duct as it passes toward the apex of the tongue.[2]
Nerves
The lingual nerve is one of the sensory branches of the mandibular division of the trigeminal nerve.[5] It contains general somatic afferent nerve fibers and, after chorda tympani joins it, also carries general visceral efferent nerve fibers and special visceral afferent fibers.[6] Other sensory branches of the mandibular nerve are the auriculotemporal nerve, the buccal nerve, and the inferior alveolar nerve; however, the inferior alveolar nerve also gives off a small motor branch, the mylohyoid nerve.
The chorda tympani, a facial nerve branch, joins the lingual nerve near the lower border of the lateral pterygoid muscle within the pterygomandibular space.[3] The chorda tympani carries taste sensation from fungiform papillae on the anterior two-thirds of the tongue. It also carries preganglionic parasympathetic fibers for control of secretion by the sublingual and submandibular salivary glands.[5] These preganglionic fibers synapse in the submandibular ganglion, which is suspended from the lingual nerve, and the postganglionic parasympathetic fibers enter the glands.[7] The lingual nerve also has anterior, middle, and posterior communicating branches with the hypoglossal nerve.[1]
Physiologic Variants
Variations in the termination of the lingual nerve, specifically in its branching pattern, have been described. The lingual nerve has been found to divide into between one and four branches at its terminal end in the tongue.[2] The most common type of branching seen at the termination of the lingual nerve is two branches. Another variation is the distance the lingual nerve travels in the floor of the mouth before turning medially toward the tongue. Most lingual nerves are found to deviate toward the tongue from the floor of the mouth between the mesial of the first molar and the distal of the second molar.[2] The lingual nerve can also have connections with the mylohyoid nerves, occurring in up to 12.50% of cases.[8] When considering surgery in the infratemporal fossa or floor of the oral cavity for a patient, these possible variations in the course of the lingual nerve are extremely important to consider.
Surgical Considerations
The lingual nerve is one of the two nerves most commonly injured during oral surgery with the other being the inferior alveolar nerve.[3] Numerous procedures have been thought to cause lingual nerve damage, including mandibular resection, extraction of a third molar tooth, operations on the salivary glands, excision of tumors, and lingual flap retraction.[9][10] The lingual nerve may also suffer an injury during suspension laryngoscopy, a procedure commonly done in otorhinolaryngology. The risk of damage to the nerve increases during this procedure when there is difficulty during the surgery and longer operating times.[11] An increase in the number of second molar implants has also increased the risk of injury to the nerve.[3] However, the lingual nerve most commonly gets damaged during inferior alveolar nerve block injections and third molar tooth removals.[3][5] Reports indicate that damage to this nerve occurs during the removal of the third molar between 0 and 23% of the time.[12][13] The wide variation in reported frequencies of this injury may be due in part to the variations seen in the course of the lingual nerve. Potential mechanisms for preventing lingual nerve injury during third molar surgery include avoiding lingual flap elevation and conducting tooth sectioning.[10][14] Injury to the lingual nerve most often is temporary, resulting in hyperaesthesia, hypoaesthesia, and/or dysaesthesia in the anterior two-thirds of the tongue.[9] Reports indicate that the nerve typically repairs itself within 6 months of damage.[15] If the nerve is injured during dental work and does not repair itself, treatment can be given, including physiotherapy, pharmacotherapy, and stellate ganglion block.[16] It can sometimes be repaired with a direct epineural repair or indirect (graft) neurorrhaphy, most commonly using the sural nerve[4].
The lingual nerve can also be the target for a nerve block during certain pathological conditions and procedures. Specifically, a lingual nerve block has been found to be useful for procedures and conditions occurring within the soft tissues of the tongue, including minor infections, traumatic lacerations, and pathological lesions.[17] Benefits of a lingual nerve block instead of an inferior alveolar nerve block include avoiding unnecessary anesthesia of the lip, chin, and buccal soft tissues.[17] This difference is an especially important consideration in patients with mental deficits, children, and the elderly, who present with traumatic lip biting.[17]
Clinical Significance
As the lingual nerve travels from the infratemporal fossa to underneath the tongue, it can become entrapped by several structures, including fibers of the lateral pterygoid muscle, pterygospinous or pterygoalar ligaments, and the lateral pterygoid plate. Entrapment of the lingual nerve can cause numbness and loss of taste from the anterior two-thirds of the tongue, loss of sensation from the lingual gingiva, and pain with speech disorders.[18]
Smoking can impact the somatosensory function of the lingual nerve, causing degeneration of the nerve fibers. Studies have indicated that smokers have a loss of non-noxious thermal stimuli, but not loss of sensation of mechanical or painful thermal stimuli.[19] A hypothesis to the cause of this sensory change is the degeneration of the thermoreceptors.[19]