Adenopathy
- Article Author:
- Andrew Freeman
- Article Editor:
- Patricia Matto
- Updated:
- 7/10/2020 1:44:57 AM
- For CME on this topic:
- Adenopathy CME
- PubMed Link:
- Adenopathy
Introduction
Lymphadenopathy is a common abnormal finding during the course of the physical exam in general medical practice. Patients and physicians have varying degrees of associated anxiety with the finding of lymphadenopathy as a small number of cases can be caused by neoplasm or infections of consequence, for example, HIV or tuberculosis (TB). However, it is generally recognized that the majority of lymphadenopathy, both localized and generalized, is of benign, self-limited, etiology. A clear understanding of lymph node function, location, description, and the etiologies of their enlargement is important in the clinical decisions of which cases need rapid and aggressive workup, and which need only be observed.[1][2][3]
The lymph node functions as an antigen filter for the reticuloendothelial (RE) system of the body. It consists of a multi-layered sinus that sequentially exposes B-cell lymphocytes, T-cell lymphocytes, and macrophages to an afferent extracellular fluid. In this way, the immune system can recognize and react to foreign proteins and mount an immune response or sequester these proteins as appropriate. In the course of this reaction, there is some multiplication of the responding immune cell line, and thus, the node itself increases in size. It is generally held that a node size is considered enlarged when it is larger than 1 cm. However, the reality is that "normal" and "enlarged" criteria vary depending on the location of the node and the age of the patient. For example, children younger than 10 years of age have more hypertrophic immune systems and nodes up to 2 cm can be considered normal in some clinical situations yet, an epitrochlear node of above 0.5 cm is considered pathological in an adult.
The pattern, distribution, and quality of the lymphadenopathy can provide much clinical information in the diagnostic process. Lymphadenopathy occurs in 2 patterns: generalized and localized. Generalized lymphadenopathy entails lymphadenopathy in 2 or more non-contiguous locations. Localized adenopathy occurs in contiguous groupings of lymph nodes. Lymph nodes are distributed in discrete anatomical areas, and their enlargement reflects the lymphatic drainage of their location. The nodes themselves may be tender or non-tender, fixed or mobile, and discreet or "matted" together. Concomitant symptomatology and the epidemiology of the patient and the illness provide further diagnostic cues. A thorough history of any prodromal illness, fever, chills, night sweats, weight loss, and localizing symptoms can be very revealing. Additionally, the demographic particulars of the patient, including age, gender, exposure to infectious disease, toxins, medications, and their habits may provide further cues.
As evidenced above, the critical step in evaluation for adenopathy is a careful history and focused physical exam. The extent of the history and physical is determined by the clinical presentation of the patient. For example, a patient with posterior cervical adenopathy sore throat and tremendous fatigue needs only a careful history, cursory examination and a mono test, while a person with generalized lymphadenopathy and fatigue would require a much more extensive investigation. Generally, the majority of the lymphadenopathy is localized (some site a 3:1 ratio), with the majority of that being represented in the head and neck region (again some site a 3:1 ratio). It also is accepted, that all generalized lymphadenopathy merits clinical evaluation and the presence of "matted lymphadenopathy" is strongly indicative of significant pathology.Examination of the patient's history, physical examination, and the demographic in which they fall can allow the patient to be placed into 1 of several different accepted algorithms for workup of lymphadenopathy. The use of these cues and selection of the correct arm of the algorithm allows for fairly rapid and cost-effective diagnosis of lymphadenopathy including determination when it is safe to observe.[4][5][6]
Algorithmic Analysis of Lymphadenopathy
After a history and physical examination are completed, lymphadenopathy is placed into 3 categories:
- "Diagnostic" such as strep pharyngitis or upper respiratory tract disease in which case the course of action is to treat the condition
- "Suggestive" such as mononucleosis lymphoma or HIV wherein the history and physical strongly suggestive diagnosis specific testing is performed and if positive the action is to treat the condition
- "Unexplained" where the lymphadenopathy is divided into generalized lymphadenopathy and localized lymphadenopathy
- For unexplained localized lymphadenopathy, a review of history, a regional exam and the epidemiological clues are used to separate patients into lower (no risk of malignancy or serious disease) versus higher risk for serious disease or malignancy categories. If the patient is at no risk for malignancy or serious illness, the reasonable course of action is to observe the patient for 3 to 4 weeks to see if the lymphadenopathy resolves or improves. In which case, the clinician is safely cleared to follow the patient. If the lymphadenopathy does not resolve or improve, the next step is to obtain a biopsy. If the patient is judged to have a risk for malignancy or serious illness the procedure is to proceed immediately to biopsy.
- For unexplained generalized lymphadenopathy, the key to diagnosis is a history to evaluate for suspected causes. Initial search would be questioning for a mononucleosis-type syndrome such as evidenced by fever atypical lymphocytosis and malaise included in these differentials would be Epstein-Barr virus, cytomegalovirus, toxoplasmosis, and (especially in the case of a flu-like illness and her rash) the initial stages of an HIV infection. The second step in the evaluation of unexplained generalized lymphadenopathy involves a careful review of epidemiological cues. Included in the epidemiological cues would be:
- Infectious disease exposure
- Animal exposure
- Insect bites
- Recent travel
- Complete medication history
- Personal habits-smoking, consumption of alcohol, consumption of drugs-special attention to a history of IVTA, high-risk sexual behavior
- Consumption of under-cooked food/untreated water
Although there is no "cookbook" for the laboratory evaluation of generalized unexplained lymphadenopathy, initial steps are to obtain a complete blood count (CBC) with a manual differential and EBV serology. If non-diagnostic, the next steps would be PPD placement, RPR, chest x-ray, ANA, hepatitis B surface antigen, and HIV test. Again if any of the above are positive, appropriate treatment can be initiated. In the presence of negative serological examinations and radiological examinations and or significant symptomology, a biopsy of the abnormal node is the gold standard for diagnosis.Statistics concerning lymphadenopathy are not accurate as the great majority of lymphadenopathy is caused by a non-reportable illness and thus not reported or taken into account. This results in a statistical bias, or skew, toward the reportable causes of lymphadenopathy: malignancies, HIV, tuberculosis, and sexually transmitted infections (STIs). Citations in the recent literature for general medical practice indicate that less than 1% of people with lymphadenopathy have malignant disease most often due to leukemia and younger children Hodgkin disease in adolescence non-Hodgkin disease and chronic lymphocytic leukemia (CLL) in adults. It has been reported the general prevalence of malignancy is 0.4% in patients under 40 years and around 4% in those older than 40 years of age seen in a primary care setting. It is reported that the prevalence rate of neoplastic disease rises to near 20% in referral centers and rises to 50% or more in patients with initial risk factors.
Etiology
The etiology of lymphadenopathy includes the following:
- Infectious disease
- Neoplasm
- Inflammatory disease
- Autoimmune disease
- Inborn metabolic storage disorder
- Exposure to toxic/medication
Infectious disease can be of viral, bacterial, mycobacterial, fungal or parasitic etiology:
- Viral etiologies of lymphadenopathy include HIV, mononucleosis caused by EBV or CMV, roseola, HSV, varicella, and adenovirus.
- Bacterial etiologies of lymphadenopathy include Staphylococcus, Streptococcus, Salmonella, Syphilis, and Yersinia
- Mycobacterial etiology of lymphadenopathy include tuberculosis and Mycobacterium avium intracellulare (MAI)
- Fungal etiology of lymphadenopathy include coccidiomycosis and Candida
- Parasitic etiology of lymphadenopathy include toxoplasmosis, histoplasmosis, Chagas, and many of the ectoparasites
- Neoplastic causes of lymphadenopathy include both primary malignancies and metastatic malignancies: Acute lymphoblastic leukemia (ALL), Hodgkin lymphoma, non-Hodgkin lymphoma, neuroblastoma, pediatric acute myelocytic leukemia, rhabdomyosarcoma, metastatic carcinoma of the lung, metastatic carcinoma of the viscera of the gastrointestinal (GI) tract, metastatic breast cancer, and metastatic thyroid cancer and metastatic renal cancer.
- Autoimmune disease these causes of lymphadenopathy include sarcoidosis, juvenile rheumatoid arthritis (JRA), serum sickness, systemic lupus erythematosus (SLE)
- Exposures to toxins and medications that are common causes of lymphadenopathy include the medications allopurinol, atenolol, captopril, carbamazepine, many of the cephalosporins, gold, hydralazine, penicillin, phenytoin, primidone, para methylamine, quinidine, the sulfonamides, and sulindac. The lifestyle exposures to alcohol, ultraviolet (UV) radiation, and tobacco can cause cancers with secondary lymphadenopathy.
- Inborn metabolic storage disorders (including Niemann-Pick disease and Gaucher disease) are possible additional causes of lymphadenopathy
Epidemiology
Broad generalities can safely be made about the epidemiology of lymphadenopathy.[7][8][9]
First, both generalized and localized lymphadenopathies are fairly equally distributed without regard to gender.
Second, lymphadenopathy is more prevalent in the pediatric population than in the adult population secondary to the greater number of viral infections. It would follow that the majority of the time, lymphadenopathy in the pediatric population is of less consequence again secondary to the prevalence of viral and bacterial infections in that age group. Three-quarters of all lymphadenopathy observed are localized, and of those three-quarters, half of these are localized to the head and neck area. All remaining localized lymphadenopathy is found in the inguinal area, and the remaining lymphadenopathy is found in the axilla in the supraclavicular area. Of note, the differential diagnosis of lymphadenopathy changes significantly with the age of the patient.
Third, the patient's location and circumstance are very revealing and lymphadenopathy. For example, in the developing world (sub-Saharan Africa, Southeast Asia, Indian subcontinent), exposure to parasites, HIV, and miliary TB are far more likely to be causes of generalized lymphadenopathy then in the United States and Europe. Whereas, Epstein-Barr virus, streptococcal pharyngitis, and some neoplastic processes are more likely candidates to cause lymphadenopathy in the United States and the remainder of the localized industrial world. An exposure history is very important for diagnosis.
- Exposure to blood and blood-borne products either through transfusion, unsafe sexual practices, intravenous drug abuse, or vocation
- Exposure to infectious disease whether it be travel, in the workplace, or the home
- Medication exposure-prescription, nonprescription, or supplements
- Exposure to animal-borne illness either via pets or the workplace
- Exposure to arthropod bites
Pathophysiology
Lymphatic fluid represents the totality of the interstitial fluid of the body, and the lymphatic channels conduct this fluid and label antigens with antigen-presenting cells. As the lymphatic channels progress, they converge regionally to form discreet lymph nodes. The function of the lymph node is to evaluate and when possible, process and initiate the immune response to the presented antigens. Lymph nodes can be thought of like a mesh of reticular cells containing lobules wherein the antigens are presented to the immune system. Lobules anatomically contain 3 discreet compartments (cortex, paracortex, and medulla) in which B-cells, T-cells, and macrophages are separately sequestered.
The appropriate cell line responds to the presented antigen by increasing its numbers. Commonly the cell lines can multiply by 3 to 5 times in 6 to 24 hours. The reticular network can stretch to contain the cell-swollen lobules. This increases the size of the lymph node and causes the clinical phenomenon of lymphadenopathy.
Lymph nodules are integrated with afferent and efferent blood vessels which allow a rich interface between intravascular and extravascular spaces. Macroscopically, the result is antigenic "policing" of both intravascular and interstitial fluids and ready immune response to threats. Microscopically, the decentralized hubs of antigen presentation and response allow for prompt action with an economy of lymphoid resources.
History and Physical
A history and physical examination are the cornerstones of time and cost-effective diagnosis of adenopathy. The depth and the extent of the H&P conducted are proportional to the obscurity of the etiology of the adenopathy. The obvious presence of strep pharyngitis and its related localized anterior cervical adenopathy requires far less clinical brain-power than generalized adenopathy secondary to sarcoidosis or a Gaucher disease.
The history itself involves gathering 5 important components: chronicity, localization, concomitant symptoms, patient epidemiology, and pharmacological exposure.
- Chronicity: The accepted definition of "chronic adenopathy" is a duration of greater than 3 weeks and the observation that duration of fewer than 2 weeks or greater than 1 year is usually associated with benign causality.
- Localization: The first determination is if the adenopathy can be viewed as localized or generalized. The accepted definition of generalized lymphadenopathy is clinical lymphadenopathy in 2 or more non-contiguous areas. Generalized adenopathy may be indicative of systemic illness, and the workup is typically more laboratory and imaging-intensive and pursued more rapidly. Localized beds of enlarged nodes reflect possible localized pathology in the areas in which they drain.
- Physical characterization of the node itself
- Concomitant symptoms: The presence or absence of constitutional symptoms is a major cue in the determination of the pace and depth of the workup in lymphadenopathy when taken in the clinical context. For example fever, chills, night sweats, weight loss and fatigue are worrisome in the setting of generalized lymphadenopathy. However, similar symptoms are acceptable in the setting of localized cervical lymphadenopathy and a concomitant Flu or Strep.
- Epidemiology: Included in the epidemiological search for lymphadenopathy, will be questions pertaining to: Dietary exposure, pet exposure, insect bite, recent blood exposure, high risk sexual behavior or intravenous drug use, occupational exposure to animals, and travel related epidemiology especially attention to travel to third world or the Southwest in the United States.
- Pharmacological exposure: A thorough medical history is necessary including prescription medications, over-the-counter medications, supplements and herbal medicines.
Physical examination can be quite revealing especially with the location of the adenopathy and consideration of the lymphatic drainage of the related areas. Once the determination has been made that the lymphadenopathy is either localized or general, strict attention to the localized area must be paid. For example:
- Submandibular nodes typically drain the tongue the lips and the mouth and the conjunctiva
- Submental nodes typically drain the lower lip portions of the oropharynx and the cheek
- Jugular lymphadenopathy typically drains the tongue, the tonsils, the pinna, and the parotid gland
- Posterior cervical adenopathy typically is indicative of scalp, neck, skin of the arms and legs
- Pectoral thoracic cervical and axillary drainage
- Suboccipital nodes reflect drainage of the scalp in the head, and preauricular nodes reflect drainage the eyelids, conjunctiva temporal region, and pinna.
- Postauricular nodes reflect drainage at the scalp in the external auditory meatus.
- The right supraclavicular node represents drainage of the mediastinum the lungs in the esophagus
- Axillary nodes typically creating the arm at the thoracic wall and the breast.
- The epitrochlear nerve roots typically drain the ulnar aspect of the forearm and the hand.
- Inguinal nodes drain the penis, the scrotum, the vulva, vagina, the perineum, the gluteal region, and the lower abdominal wall and portions of the lower anal canal
Characterization of the node morphology itself:
- Tenderness-pain may result from an inflammatory process or perforation and also may result from hemorrhage into the necrotic center of a malignant node. (Presence or absence of pain not a reliable differentiating factor for malignant nodes though.)
- Consistently firm rubbery nodes may suggest lymphoma; softer nodes are usually the result of infection or inflammatory conditions; hard stonelike nodes are typically a sign of cancer more commonly metastatic than primary.
- "Shotty" nodes refers to very small, scattered nodes that feel like shotgun pellets under the skin. This configuration is typically is found in cervical nodes of children with viral illnesses
- The designation of a "matting" configuration of nodes describes the pattern of clustered, seemingly conjoined lymph nodes. This is indicative of, but not pathognomonic, for malignancy.
Evaluation
Laboratory Evaluation of Lymphadenopathy
- CBC with manual differential: This is a foundational test in the diagnosis of both generalized and regional lymphadenopathy. The number and differential of the white blood cells can indicate bacterial, viral, or fungal pathology. In addition, characteristic white blood cell (WBC) patterns are observed with several of the hematological neoplasms producing lymphadenopathy
- EBV serology: Epstein-Barr viral mono is present causing regionalized lymphadenopathy
- Sedimentation rate: A measure of inflammation though not diagnostic, it can contribute to diagnostic reasoning
- Cytomegalovirus titers: This viral serology is indicative of possible of CMV mononucleosis
- HIV serology: This serology can be used to diagnose acute HIV syndrome-related lymphadenopathy or to infer the diagnosis of secondary HIV-elated pathologies causing lymphadenopathy.
- Bartonella henselae serology: Serology that may be indicative of the diagnosis of cat-scratch lymphadenopathy
- FTA\RPR: These tests can establish if syphilis is a cause of lymphadenopathy
- Herpes simplex serology: Serological testing to discern if the herpes-related, mononucleosis-like syndrome is present or if regionalized inguinal adenopathy is secondary to herpes simplex exposure
- Toxoplasmosis serology: These serological tests can lead to a diagnosis of acute toxoplasmosis as a cause of lymphadenopathy
- Hepatitis B serology: Serological tests for hepatitis B to establish it as a contributing factor for lymphadenopathy
- ANA: A serological screening test for SLE that can help establish it as a cause for generalized lymphadenopathy
Diagnostic Radiological Testing
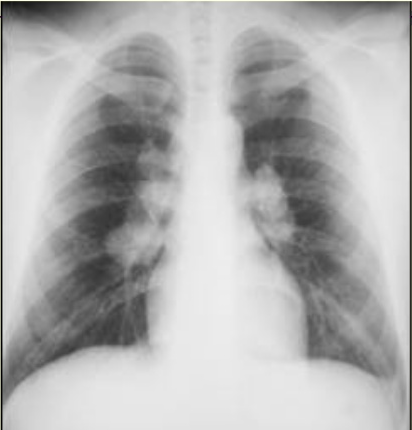
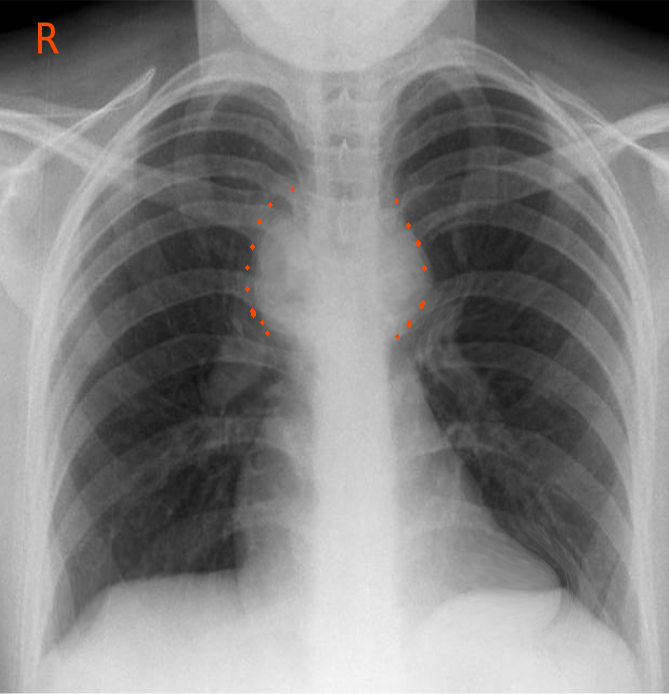
- Chest x-ray: This radiological imaging modality can reveal tuberculosis, pulmonary sarcoidosis, and pulmonary neoplasm.
- Chest CAT scan: This modality of radiological imaging can define the above processes and reveal hilar adenopathy.
- Abdominal and pelvic CAT scan: These images, in combination with chest CAT scan, can be revealing in cases of supraclavicular adenopathy and the diagnosis of secondary neoplasm.
- Ultrasonography: This imaging modality can be used in the assessment of number, size, size, shape, the marginal definition, and internal structures in patients with lymphadenopathy. Of note, color Doppler ultrasonography is of use in distinguishing the vascular pattern between older pre-existing lymphadenopathy and recent (newly active) lymphadenopathy. Studies have indicated that a low long axis to short axis ratio of lymphadenopathy as measured by ultrasound can be a significant indicator of lymphoma and metastatic cancer as a cause of lymphadenopathy.
- MRI scanning: As with CAT scanning, this modality of diagnostic imaging has great utility in the evaluation of thoracic, abdominal, and pelvic masses.
PPD
Tuberculosis is among the leading cause of both regional and generalized adenopathy in the non-industrialized world
Treatment / Management
The management and treatment of lymphadenopathy are dependent on its etiology. For example:
- Lymphadenopathy caused by a primary neoplasm: Treatment of the neoplasm
- Lymphadenopathy caused by metastasis-diagnosis of the primary: Treatment of the metastasis and primary
- Lymphadenopathy caused by bacterial disease: Supportive care, antibiotics, and elimination of nidus of infection if applicable
- Lymphadenopathy caused by viral disease: Observation and supportive care or treatment of the virus if particular antiviral medications exist
- Lymphadenopathy caused by a toxin or medication exposure: Removal of offending medication if possible or avoidance of toxin
Differential Diagnosis
The differential diagnosis of the etiology of lymphadenopathy can be thought of in the following algorithm:After a thorough history and physical examination, lymphadenopathy can be initially categorized as:
- Diagnostic-where in the practitioner has a proximal cause for the lymph nodes and can go on to treat them. Examples would be strep pharyngitis or localized cellulitis.
- The lymphadenopathy pattern history and physical examination can be suggestive an example would be mononucleosis wearing the practitioner has strong clinic index of suspicion can perform a confirmatory test which if positive he can go on and treat the patient.
- Unexplained lymphadenopathy.
- Unexplained lymphadenopathy can be generalized into localized or generalized lymphadenopathy.
Unexplained localized lymphadenopathy (after careful review of the history and epidemiology) is further divided into patterns at no risk for malignancy or serious illness in which case the patient can be observed for 3 to 4 weeks and if response or improvement can be followed. The other alternative is if the patient is found to have a risk for malignancy or serious illness biopsy is indicated
Unexplained generalized lymphadenopathy can be approached after review of epidemiological clues and medications with initial testing with a CBC with manual differential and mononucleosis serology if either is positive and diagnostic proceed to treatment. If both are negative, the second workup approach would be a PPD, and RPR, a chest x-ray, and ANA, hepatitis BS antigen serology, and HIV. Additional testing modalities and lab tests may be indicated depending on clinical cues. If the results of this testing are conclusive, the practitioner can proceed on to diagnosis and treatment at the illness. If the results of the testing are still not clear, proceed onto biopsy of the most abnormal if the nodes.The most functional way to investigate the differential diagnosis of lymphadenopathy is to characterize it by node pattern and location, obtained pertinent history including careful evaluation of epidemiology, and place the patient in the appropriate arm of the algorithm to evaluate lymphadenopathy.
Generalized Lymphadenopathy
Common Infective Causation
- Mononucleosis
- HIV
- Tuberculosis
- Typhoid fever
- Syphilis
- Plague
Malignancies
- Acute leukemia
- Hodgkin's lymphoma
- Non-Hodgkin's lymphoma
Metabolic Storage Disorders
- Gaucher disease
- Niemann-Pick disease
Medication Reactions
- Allopurinol
- Atenolol
- Captopril
- Carbamazepine
- Cephalosporin(s)
- Gold
- Hydralazine
- Penicillin
- Phenytoin
- Primidone
- Pyrimethamine
- Quinidine
- Sulfonamides
- Sulidac
Autoimmune Disease
- Sjogren syndrome
- Sarcoidosis
- Rheumatoid arthritis
- Systemic lupus erythematosus
Localized Peripheral Lymphadenopathy
Head and Neck Lymph Nodes
Viral infection
- Viral URI
- Mononucleosis
- Herpes virus
- Coxsackievirus
- Cytomegalovirus
- HIV
Bacterial infection
- Staphylococcal aureus
- Group A Streptococcus pyogenes
- Mycobacterium
- Dental abscess
- Cat scratch disease
Malignancy
- Hodgkin disease
- Non-Hodgkin lymphoma
- Thyroid cancer
- Squamous cell carcinomas of the head and neck
Inguinal Peripheral Lymphadenopathy
Infection
- STDs
- Cellulitis
Malignancy
- Lymphoma
- Squamous cell carcinoma of genitalia
- Malignant melanoma
Axillary Lymphadenopathy
Infection
- Localized Staphylococcal aureus
- Cat-scratch disease
- Brucellosis
Malignancy
- Lymphoma
- Breast cancer
- Melanoma
Reaction to breast implants
Supraclavicular Adenopathy
Infections
- Mycobacteria
- Fungi
Malignancy
- Thoracic and abdominal neoplasms
- Hodgkin disease
- Non-Hodgkin lymphoma
Prognosis
The prognosis of lymphadenopathy, whether localized or generalized, is entirely dependent on the etiology of the enlarged lymph nodes. Most adenopathy in the general medicine office is caused by a treatable bacterial or treatable viral illness. However, HIV, active tuberculosis, and neoplasm all have more guarded prognoses. Generalities include the majority of localized lymphadenopathy has a better prognosis than the majority of generalized lymphadenopathy secondary to etiologies. Etiologies that are established earlier in a clinical setting will tend to have better prognoses than those established later.
Complications
Pitfalls and pearls of the diagnosis and treatment of lymphadenopathy include:
- There is no substitute for a thorough history and careful physical examination in the workup of lymphadenopathy.
- The majority of both localized and generalized lymphadenopathy have a relatively benign treatable cause.
- All generalized lymphadenopathy merits careful evaluation and workup.
- The gold standard for diagnosis of lymphadenopathy remains tissue diagnosis of the node by incisional biopsy.
- A careful review of the patient's epidemiological and personal medical history provides daily clues as to when lymphadenopathy can be safely observed for change or resolution over the period of 2 to 4 weeks.
- Supraclavicular lymphadenopathy is almost universally indicative of underlying thoracic or abdominal malignancy.
Deterrence and Patient Education
Patient education plays a significant role in the deterrence of the processes that can cause pathological lymphadenopathy.
- Smoking cessation, alcohol moderation, modification of unsafe sexual practices, and avoidance of drug use can significantly decrease the rate of cancers, HIV, hepatitis B and C, and sexually transmitted infections.
- Appropriate vaccination, good hygiene, good public sanitation, and careful infectious disease protocols can significantly decrease the rate of recurrence, and transmission of infections causing lymphadenopathy.
Pearls and Other Issues
- Seventy-five percent of all lymphadenopathies are localized, with more than 50% seen in the head and neck area.
- Most supraclavicular lymphadenopathies are associated with malignancy.
- The most powerful tool in the diagnosis of lymphadenopathy is a careful history and physical examination.
- The gold standard for diagnosis of lymphadenopathy is tissue obtained either by fine-needle aspiration or excisional biopsy.
- All generalized lymphadenopathy needs to be carefully worked up and the diagnosis established.
Enhancing Healthcare Team Outcomes
The primary physician, physician assistant, and nurse practitioner can diagnose a significant number of the causes of lymphadenopathy after a careful workup. However, when the diagnosis is in question varied, consultants can be utilized to clarify the situation to provide the best outcomes. For example:
- Interventional radiology: Examination of the tissue specimen remains the gold standard for the diagnosis of lymphadenopathy.
- General surgery, otorhinolaryngology, urological, thoracic surgery: Clinical circumstance may dictate the need for an excisional biopsy as opposed to a biopsy sample examination
- Infectious disease: For the provision of input on both diagnosis and treatment of infectious causes of lymphadenopathy
- Rheumatology: For the provision of input on both diagnosis and treatment of rheumatologic diseases causing lymphadenopathy
- Allergy and immunology: For the provision of input on both diagnosis and treatment of autoimmune, toxicological exposure, and medication-related exposure causes of lymphadenopathy
- Hematology and oncology: For the provision of input on both diagnosis and treatment of neoplastic causes of lymphadenopathy
(Click Image to Enlarge)

This plague patient is displaying a swollen, ruptured inguinal lymph node, or buboe. After the incubation period of 2-6 days, symptoms of the plague appear including severe malaise, headache, shaking chills, fever, and pain and swelling, or adenopathy, in the affected regional lymph nodes, also known as buboes.
Contributed by The Centers for Disease Control and Prevention (CDC)