Case Study: 60-Year-Old Female Presenting With Shortness of Breath
- Article Author:
- Deepa Rawat
- Article Editor:
- Sandeep Sharma
- Updated:
- 4/19/2020 10:26:29 PM
- For CME on this topic:
- Case Study: 60-Year-Old Female Presenting With Shortness of Breath CME
- PubMed Link:
- Case Study: 60-Year-Old Female Presenting With Shortness of Breath
Case Presentation
The patient is a 60-year-old white female presenting to the emergency department with acute onset shortness of breath. Symptoms began approximately 2 days before and had progressively worsened with no associated, aggravating, or relieving factors noted. She had similar symptoms approximately 1 year ago with an acute, chronic obstructive pulmonary disease (COPD) exacerbation requiring hospitalization. She uses BiPAP ventilatory support at night when sleeping and has requested to use this in the emergency department due to shortness of breath and wanting to sleep.
She denies fever, chills, cough, wheezing, sputum production, chest pain, palpitations, pressure, abdominal pain, abdominal distension, nausea, vomiting, and diarrhea.
She does report difficulty breathing at rest, forgetfulness, mild fatigue, feeling chilled requiring blankets, increased urinary frequency, incontinence, and swelling in her bilateral lower extremities that is new onset and worsening. Subsequently, she has not ambulated from bed for several days except to use the restroom due to feeling weak, fatigued, and short of breath.
There are no known ill contacts at home. Her family history includes significant heart disease and prostate malignancy in her father. Social history is positive for smoking tobacco use at 30 pack years. She quit smoking 2 years ago due to increasing shortness of breath. She denies all alcohol and illegal drug use. There are no known foods, drugs, or environmental allergies.
Past medical history is significant for coronary artery disease, myocardial infarction, COPD, hypertension, hyperlipidemia, hypothyroidism, diabetes mellitus, peripheral vascular disease, tobacco usage, and obesity. Past surgical history is significant for an appendectomy, cardiac catheterization with stent placement, hysterectomy, and nephrectomy.
Her current medications include Breo Ellipta 100-25 mcg inhaled daily, hydralazine 50 mg by mouth, 3 times per day, hydrochlorothiazide 25 mg by mouth daily, Duo-Neb inhaled q4 hr PRN, levothyroxine 175 mcg by mouth daily, metformin 500 mg by mouth twice per day, nebivolol 5 mg by mouth daily, aspirin 81 mg by mouth daily, vitamin D3 1000 units by mouth daily, clopidogrel 75 mg by mouth daily, isosorbide mononitrate 60 mg by mouth daily, and rosuvastatin 40 mg by mouth daily.
Physical Exam
Initial physical exam reveals temperature 97.3 F, heart rate 74 bpm, respiratory rate 24, BP 104/54, BMI 40.2, and O2 saturation 90% on room air.
Constitutional: Extremely obese, acutely ill-appearing female. Well-developed and well-nourished with BiPAP in place. Lying on a hospital stretcher under 3 blankets.
HEENT:
- Head: Normocephalic and atraumatic
- Mouth: Moist mucous membranes
- Macroglossia
- Eyes: Conjunctiva and EOM are normal. Pupils are equal, round, and reactive to light. No scleral icterus. Bilateral periorbital edema present.
- Neck: Neck supple. No JVD present. No masses or surgical scarring.
- Throat: Patent and moist
Cardiovascular: Normal rate, regular rhythm, and normal heart sound with no murmur. 2+ pitting edema bilateral lower extremities and strong pulses in all four extremities.
Pulmonary/Chest: No respiratory status distress at this time, tachypnea present, (+) wheezing noted, bilateral rhonchi, decreased air movement bilaterally. Patient barely able to finish a full sentence due to shortness of breath.
Abdominal: Soft. Obese. Bowel sounds are normal. No distension and no tenderness
Skin: Skin is very dry
Neurologic: Alert, awake, able to protect her airway. Moving all extremities. No sensation losses
Initial Evaluation
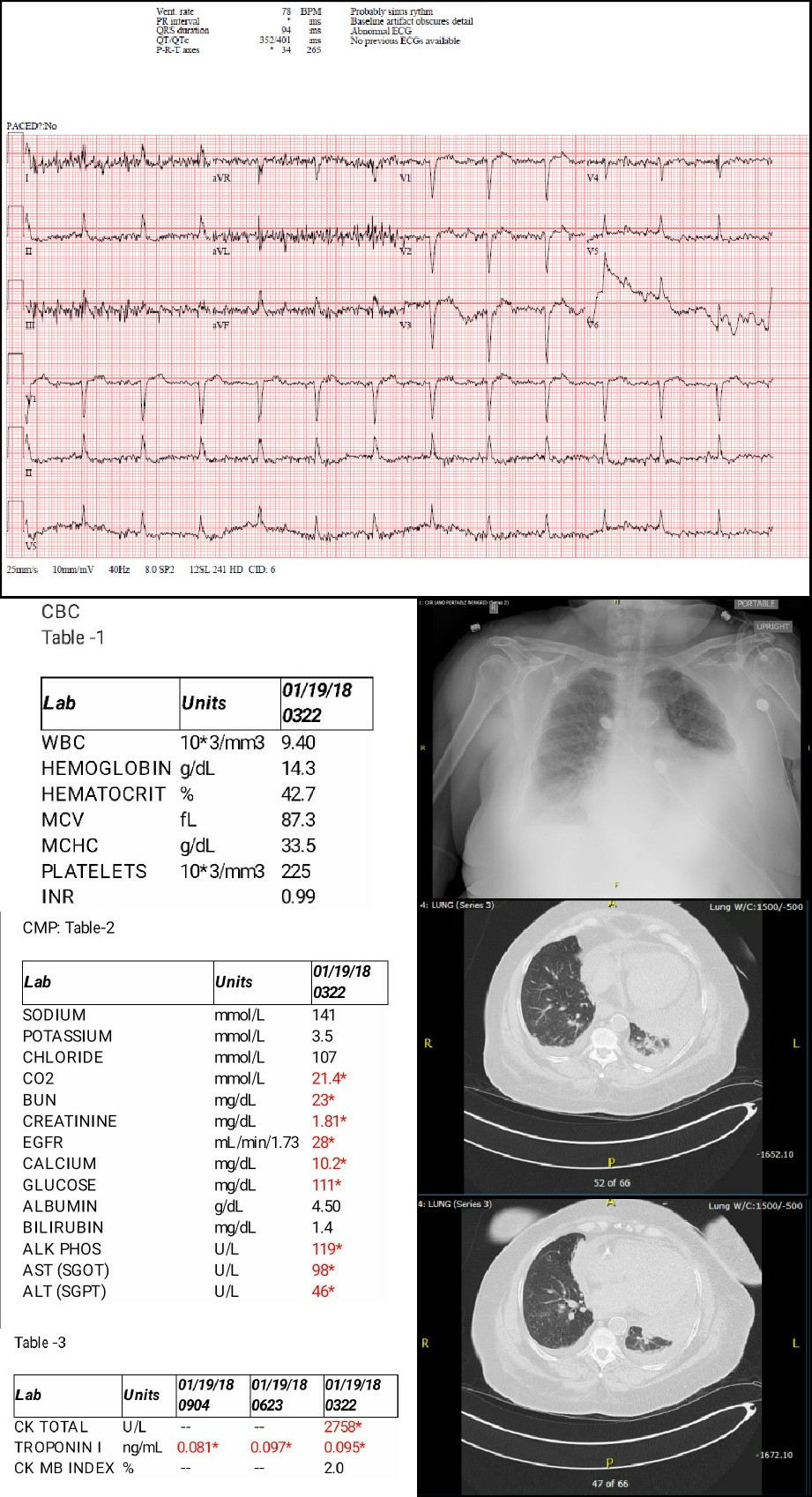
Initial evaluation to elucidate the source of dyspnea was performed and included CBC to establish if an infectious or anemic source was present, CMP to review electrolyte balance and review renal function, and arterial blood gas to determine the PO2 for hypoxia and any major acid-base derangement, creatinine kinase and troponin I to evaluate presence of myocardial infarct or rhabdomyolysis, brain natriuretic peptide, ECG, and chest x-ray. Considering that it is winter and influenza is endemic in the community, a rapid influenza assay was obtained as well.
CBC
Largely unremarkable and non-contributory to establish a diagnosis.
CMP
Showed creatinine elevation above baseline from 1.08 base to 1.81 indicating possible acute injury. EGFR at 28 is consistent with the chronic renal disease. Calcium was elevated to 10.2. However, when corrected for albumin this corrected to 9.8 mg/dL. Mild transaminitis present as seen in Alkaline Phosphatase, AST, and ALT measurements which could be due to liver congestion from volume overload.
Initial arterial blood gas with pH 7.491, PCO2 27.6, PO2 53.6, HCO3 20.6, and oxygen saturation 90% on room air indicating respiratory alkalosis with hypoxic respiratory features.
Creatinine kinase was elevated along with serial elevated troponin I studies. In the setting of her known chronic renal failure, and in the setting of acute injury indicated by the above creatinine value, a differential of rhabdomyolysis is set.
Influenza A and B: Negative
ECG
Normal sinus rhythm with non-specific ST changes in inferior leads. Decreased voltage in leads I, III, aVR, aVL, aVF.
Chest X-ray
Findings: Bibasilar airspace disease that may represent alveolar edema. Cardiomegaly noted. Prominent interstitial markings noted. Small bilateral pleural effusions
Radiologist Impression: Radiographic changes of congestive failure with bilateral pleural effusions greater on the left compared to the right
Differential Diagnosis
- Acute on chronic COPD exacerbation
- Acute on chronic renal failure
- Bacterial pneumonia
- Congestive heart failure
- NSTEMI
- Pericardial effusion
- Hypothyroidism
- Influenza pneumonia
- Pulmonary edema
- Pulmonary embolism
Confirmatory Evaluation
The second day of the admission patient’s shortness of breath was not improved, and she was more confused with difficulty arousing on conversation and examination. To further elucidate the etiology of her shortness of breath and confusion further history was obtained via the patient’s husband. He revealed that she is poorly compliant with taking her medications. He reports that she “doesn’t see the need to take so many pills.”
Testing was performed to include TSH, free T4, BNP, repeated arterial blood gas, CT scan of the chest, and echocardiogram. TSH and free T4 evaluate hypothyroidism. BNP evaluates fluid load status and possible congestive heart failure. CT scan of the chest will look for anatomical abnormalities. An echocardiogram is used to evaluate for left ventricular ejection fraction, right ventricular function, pulmonary artery pressure, valvular function, pericardial effusion and any hypokinetic area.
- TSH: 112.717 (H)
- Free T4: 0.56 (L)
- TSH and Free T4 values indicate severe primary hypothyroidism.
- BNP: 187
BNP can be falsely low in obese patients due to the increased surface area. Additionally, adipose tissue has BNP receptors which augment the true BNP value. Also, African American patients more excretion may have falsely low values secondary to greater excretion of BNP. This test is not that helpful in renal failure due to the chronic nature of fluid overload. This allows for desensitization of the cardiac tissues with a subsequent decrease in BNP release.
Repeat arterial blood gas on BiPAP ventilation shows pH 7.397, PCO2 35.3, PO2 72.4, HCO3 21.2, and oxygen saturation 90% on 2 L supplemental oxygen.
CT chest without contrast was mainly obtained to evaluate left hemithorax especially retrocardiac area.
Radiologist Impression: Tiny bilateral pleural effusions. Pericardial effusion. Coronary artery calcification. Some left lung base atelectasis with minimal airspace disease.
Echocardiogram
The left ventricular systolic function is normal. The left ventricular cavity is borderline dilated.
The pericardial fluid is collected primarily posteriorly, laterally but not apically. There appeared to be a subtle, early hemodynamic effect of the pericardial fluid on the right-sided chambers by way of an early diastolic collapse of the RA/RV and delayed RV expansion until late diastole. Dedicated tamponade study was not performed.
Estimated ejection fraction appears to be in the range of 66% to 70%. The left ventricular cavity is borderline dilated.
The aortic valve is abnormal in structure and exhibits sclerosis.
The mitral valve is abnormal in structure. Mild mitral annular calcification is present. There is bilateral thickening present. Trace mitral valve regurgitation is present.
Diagnosis
- Myxedema coma or severe hypothyroidism
- Pericardial effusion secondary to myxedema coma
- COPD exacerbation
- Acute on chronic hypoxic respiratory failure
- Acute respiratory alkalosis
- Bilateral community-acquired pneumonia
- Small bilateral pleural effusions
- Acute mild rhabdomyolysis
- Acute chronic, stage IV, renal failure
- Elevated troponin I levels, likely secondary to Renal failure
- Diabetes mellitus type 2, non-insulin dependent
- Extreme obesity
- Hepatic dysfunction
Management
The patient was extremely ill and rapidly decompensating with multisystem organ failure including respiratory failure, altered mental status, acute on chronic renal failure, and cardiac dysfunction. The primary concerns for the stability of the patient revolved around the respiratory failure coupled with altered mental status. In the intensive care unit (ICU), she rapidly began to fail BiPAP therapy. Subsequently, the patient was emergently intubated in the ICU. A systemic review of therapies and hospital course is as follows:
Endocrine
Considering the primary diagnosis of myxedema coma, early supplementation with thyroid hormone is essential. Healthcare providers followed the American Thyroid Association recommendations which recommend giving combined T3 and T4 supplementation; however, T4 alone may also be used. T3 therapy is given as a bolus of 5 to 20 micrograms intravenously and continued at 2.5 to 10 micrograms every 8 hours. An intravenous loading dose of 300 to 600 micrograms of T4 is followed by a daily intravenous dose of 50 to 100 micrograms. Repeated monitoring of TSH and T4 should be performed every 1 to 2 days to evaluate the effect and to titrate the dose of medication. The goal is to improve mental function. Until coexistent adrenal insufficiency is ruled out using a random serum cortisol measurement, 50 to 100 mg every 8 hours of hydrocortisone should be administered. In this case, clinicians used hydrocortisone 100 mg IV every 8 hours. Dexamethasone 2 to 4 mg every 12 hours is an alternative therapy.
Neurologic
The patient’s mental status rapidly worsened despite therapy. In the setting of her hypothyroidism history, this may be myxedema coma or due to the involvement of another organ system. The thyroid supplementation medications and hydrocortisone were continued. A CT head without contrast was normal.
Respiratory
For worsening metabolic acidosis and airway protection, the patient was emergently intubated. Her airway was deemed high risk due to having a large tongue, short neck, and extreme obesity. As the patient’s heart was preload dependent secondary to pericardial effusion, a 1-liter normal saline bolus was started. Norepinephrine was started at a low dose for vasopressor support and ketamine with low dose Propofol was used for sedation. Ketamine is a sympathomimetic medication and usually does not cause hypotension as all other sedatives do. The patient was ventilated with AC mode of ventilation, tidal volume of 6 ml/kg ideal body weight, flow 70, initial fio2 100 %, rate 26 per minute (to compensate for metabolic acidosis), PEEP of 8.
Cardiovascular
She was determined to be hemodynamically stable with a pericardial effusion. This patient’s cardiac dysfunction was diastolic in nature as suggested by an ejection fraction of 66% to 70%. The finding of posterior pericardial effusion further supported this conclusion. The posterior nature of this effusion was not amenable to pericardiocentesis. As such, this patient was preload dependent and showed signs of hypotension. The need for crystalloid fluid resuscitation was balanced against the impact increased intravascular volume would have on congestive heart failure and fluid overload status. Thyroid hormone replacement as above should improve hypotension. However, vasopressor agents may be used to maintain vital organ perfusion targeting a mean arterial pressure of greater than 65 mm Hg as needed. BP improved after fluid bolus and eventually the norepinephrine was stopped. Serial echocardiograms were obtained to ensure that the patient did not develop tamponade physiology. Total CK was elevated which was likely due to Hypothyroidism compounded with the chronic renal disease.
Infectious Disease
Blood cultures, urine analysis, and sputum cultures were obtained. The patient's white blood cell count was normal. This is likely secondary to her being immunocompromised due to hypothyroidism and diabetes. In part, the pulmonary findings of diffuse edema and bilateral pleural effusions can be explained by the cardiac dysfunction. Thoracentesis of pleural fluid was attempted and the fluid analyzed for cytology and gram staining to rule out infectious or malignant causes as both a therapeutic and diagnostic measure. Until these results return, broad-spectrum antibiotics are indicated and may be discontinued once the infection is ruled out completely.
Gastrointestinal
Nasogastric tube feedings were started on the patient after intubation. She tolerated feedings well. AST and ALT were mildly elevated which was thought to be due to hypothyroidism and as the TSH and free T4 improved her AST and ALT improved. Eventually, these values became normal once her TSH level was close to 50.
Renal
Her baseline creatinine was found to be close to 1.08 in prior medical records. She presented with a creatinine of 1.8 in the emergency department. As hypothyroidism causes fluid retention in part due to the fact that thyroid hormone encourages excretion of free water and partly due to decreased lymphatic function in returning fluid to vascular circulation. Aggressive diuresis was attempted. As a result, her creatinine increased initially but improved on repeated evaluation and patient had a new baseline creatinine of 1.6. Overall she had a net change in the fluid status of 10 liters negative by her ten days of admission in the ICU.
Hematology
Mildly anemic otherwise WBC and platelet counts were normal. Electrolyte balance should be monitored closely paying attention to sodium, potassium, chloride, and calcium specifically as these are worsened in both renal failure and myxedema.
Daily sedation vacations were done, patients mental status improved and was much better when TSH was around 20. The bilateral pleural effusions improved with aggressive diuresis. Breathing trials were initiated when the patient's fio2 requirements decreased to 60% and a PEEP of 8. She was eventually extubated on to BiPAP and then high flow nasal cannula while off of BiPAP. Pericardial fluid remained stable, and no cardiac tamponade pathology developed. As a result, it was determined that a pericardial window was unnecessary. Furthermore, she was not a candidate for pericardiocentesis as the pericardial effusion was located posterior to the heart. Her renal failure improved with improved cardiac function, diuretics, and thyroid hormone replacement.
After extubation patient had speech and swallow evaluations and was able to resume an oral diet. The patient was eventually transferred out of the ICU to the general medical floor and then eventually to a rehabilitation unit.
Discussion
Despite the name myxedema coma, most patients will not present in a coma status. This illness is at its core a severe hypothyroidism crisis that leads to systemic multiorgan failure. Thyroid hormones T3, and to a lesser extent, T4 act directly on a cellular level to upregulate all metabolic processes in the body. Therefore, deficiency of this hormone is characterized by systemic decreased metabolism and decreased glucose utilization along with increased production and storage of osmotically active mucopolysaccharide protein complexes into peripheral tissues resulting in diffuse edema and swelling of tissue.[1]
Myxedema coma is an illness that occurs primarily in females at a rate of 4:1 compared to men. It typically impacts the elderly at the age of greater than 60 years old and approximately 90% of cases occur during winter months. Myxedema coma is the product of longstanding unidentified or undertreated hypothyroidism of any etiology. Thyroid hormone is necessary throughout the body and acts as a regulatory hormone, that affects many organ systems.[2]In cardiac tissues, myxedema coma manifests as decreased contractility with subsequent reduction in stroke volume and overall cardiac output. Bradycardia and hypotension are typically present also. Pericardial effusions occur due to the accumulation of mucopolysaccharides in the pericardial sac which leads to worsened cardiac function and congestive heart failure from diastolic dysfunction. Capillary permeability is also increased throughout the body leading to worsened edema. Electrocardiogram findings may include bradycardia and low-voltage, non-specific ST waveform changes with possible inverted T waves.
Neurologic tissues are impacted in myxedema coma leading to the pathognomonic altered mental status as a result of hypoxia and decreased cerebral blood flow secondary to cardiac dysfunction as above. Additionally, hypothyroidism leads to decreased glucose uptake and utilization in neurological tissue thus worsening the cognitive function.
The pulmonary system typically manifests this disease process through hypoventilation secondary to central nervous system (CNS) depression of the respiratory drive with blunting of the response to hypoxia and hypercapnia. Additionally; metabolic dysfunction in the muscles of respiration leads to respiratory fatigue and failure, macroglossia from mucopolysaccharide driven edema of the tongue leads to mechanical obstruction of the airway, and obesity hypoventilation syndrome with the decreased respiratory drive as most hypothyroid patients suffer from obesity.
Renal manifestations include decreased glomerular filtration rate from the reduced cardiac output and increased systemic vascular resistance coupled with acute rhabdomyolysis lead to acute kidney injury. In the case of our patient above who has a pre-existing renal disease status post-nephrectomy, this is further worsened. The net effect is worsened fluid overload status compounding the cardiac dysfunction and edema.[3]
The gastrointestinal tract is marked by mucopolysaccharide driven edema as well leading to malabsorption of nutrients, gastric ileus, and decreased peristalsis. Ascites are a common occurrence because of increased capillary permeability in the intestines coupled with coexistent congestive heart failure and congestive hepatic failure. Coagulopathies are common to occur as a result of this hepatic dysfunction.
Evaluation: The diagnosis of myxedema coma, as with all other diseases, is heavily reliant on the history and physical exam. A past medical history including hypothyroidism is highly significant whenever decreased mental status or coma is identified. In the absence of identified hypothyroidism myxedema coma is a diagnosis of exclusion when all other sources of coma have been ruled out. If myxedema coma is suspected, evaluation of thyroid stimulating hormone (TSH), free thyroxine (T4), and serum cortisol is warranted. T4 will be extremely low. TSH is variable depending on the etiology of hypothyroidism with a high TSH indicating primary hypothyroidism and a low or normal TSH indicating secondary etiologies. Cortisol may be low indicating adrenal insufficiency because of the hypothyroidism. [4]
Prognosis: Myxedema coma is a medical emergency. With proper and rapid diagnosis and initiation of therapy the mortality rate is still as high as 25% to 50%. The most common cause of death is due to respiratory failure. The factors which suggest a poorer prognosis include increased age, persistent hypothermia, bradycardia, low score Glasgow Coma Scale, or multi-organ impairment indicated by high APACHE (Acute Physiology and Chronic Health Evaluation) II score. For these reasons, placement in an intensive care unit with a low threshold for intubation and mechanical ventilation can improve mortality outcomes.[3][5]
Pearls of Wisdom
- Not every case of shortness of breath is COPD or congestive heart failure (CHF). While less likely, a history of hypothyroidism should raise suspicion of myxedema coma in a patient with any cognitive changes.
- Myxedema is the great imitator illness that impacts all organ system. It can easily be mistaken for congestive heart failure, COPD exacerbation, pneumonia, renal injury or failure, or neurological insult.
- Initial steps in therapy include aggressive airway management, thyroid hormone replacement, glucocorticoid therapy, and supportive measures.
- These patients should be monitored in an intensive care environment with continuous telemetry.[6]