Nevus Sebaceous
- Article Author:
- Dana Baigrie
- Article Author:
- Todd Troxell
- Article Editor:
- Christopher Cook
- Updated:
- 10/23/2020 10:12:37 AM
- For CME on this topic:
- Nevus Sebaceous CME
- PubMed Link:
- Nevus Sebaceous
Introduction
Nevus sebaceus of Jadassohn, also referred to as organoid nevus, is a congenital malformation described in 1895 by the dermatologist Josef Jadassohn. These congenital malformations are hamartomas of the pilosebaceous follicular unit. This unit includes follicular, sebaceous, and apocrine components, plus epidermal hyperplasia. These growths most commonly form on the scalp, but may also appear on the forehead, face, or neck. They undergo a growth phase during puberty due to hormonal changes in the patient's body. In adulthood, the growths may develop secondary neoplasms within them, most commonly trichoblastoma. The treatment of these lesions is controversial, with options ranging from observation to early excision in childhood.[1][2]
Etiology
Previously, dermatologists were taught that secondary carcinoma was a relatively common phenomenon, occurring in over 10% of lesions over time. However, studies have since suggested that most secondary neoplasms that develop in adulthood have benign follicular origins, such as with trichoblastoma and syringocystadenoma papilliferum. Many speculate that the malignant growths that arise in nevus sebaceus were previously misdiagnosed as basal cell carcinoma. They were likely trichoblastomas, which can share a very similar histological appearance to basal cell carcinoma. The actual incidence of basal cell carcinoma in nevus sebaceus in less than 1%. Trichoblastoma is the most frequently occurring tumor in nevus sebaceus, followed by syringocystadenoma papilliferum. Other common secondary neoplasms include tricholemmoma, sebaceous adenoma, desmoplastic tricholemmoma, apocrine adenoma, and poroma.[3][4][5][6]
Epidemiology
Approximately 0.3% of newborns are affected by nevus sebaceus, and the incidence is equal between male and female patients. The disorder affects all races and ethnicities. Overall, nevus sebaceus appears as a solitary lesion right after birth, or it may appear before puberty. However, the classic features may not fully develop until after puberty.
Pathophysiology
Nevus sebaceus is not an inherited skin lesion. It carries postzygotic somatic mutations of the Ras protein family, with one study reporting 95% of nevi with HRas mutations and 5% with KRas mutations. These Ras mutations are also present in commonly occurring secondary tumors of nevus sebaceus such as trichoblastomas. Their presence there supports the updated view that the basaloid neoplasms in these lesions are trichoblastomas. They are not the histologically similar basal cell carcinomas which have mutations in the Hedgehog and PTCH pathway.
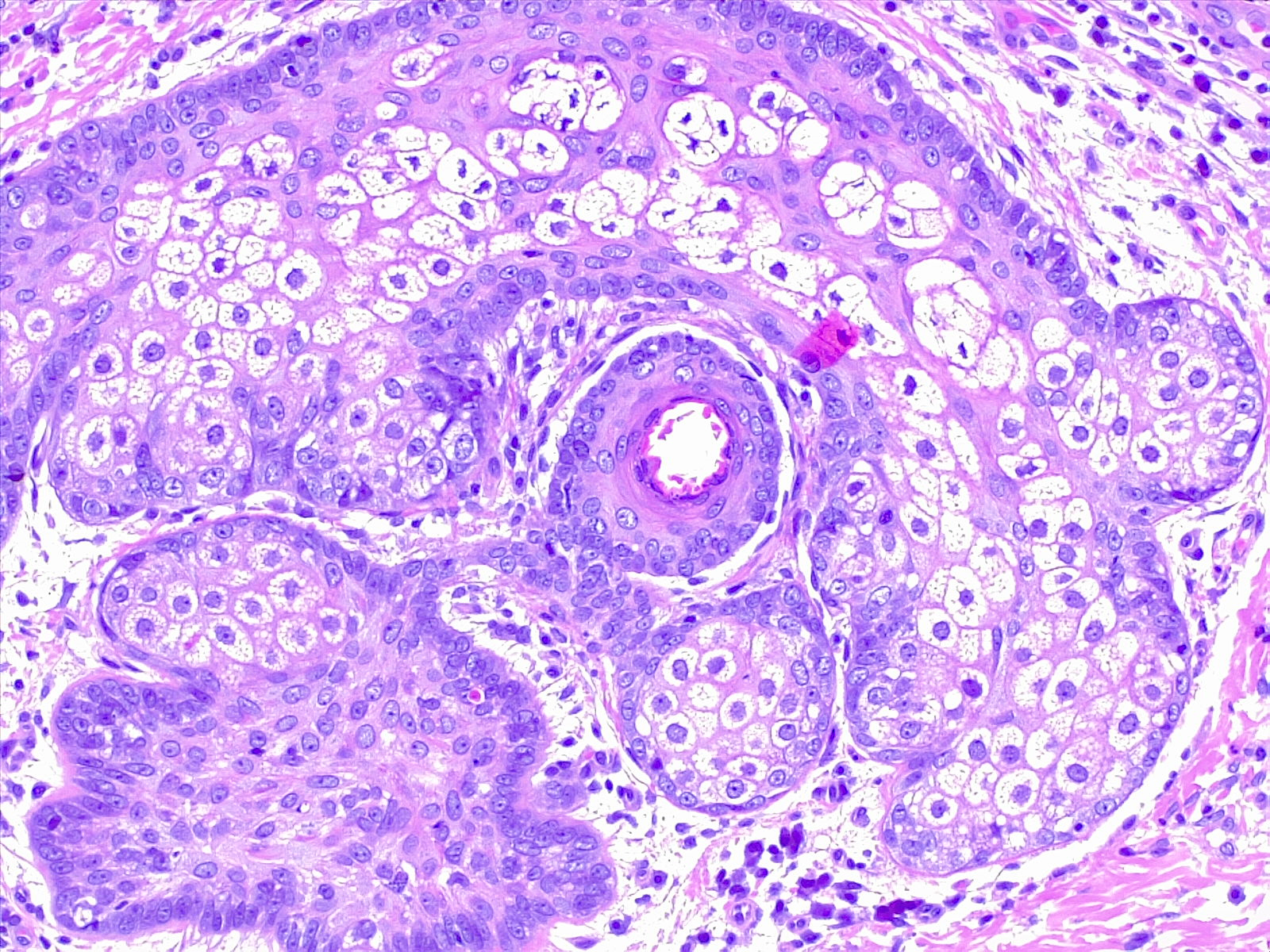
Histopathology
In infancy or early childhood, nevus sebaceus histologically features immature and abnormally formed pilosebaceous units. At this stage of development, epidermal changes may reveal some acanthosis and mild papillomatosis. During puberty, the lesions enlarge clinically as well as microscopically. The sebaceous glands become much more prominent and are located unusually high in the dermis. The number of sebaceous lobules and malformed ducts increases. The hair follicles are typically immature vellus hairs rather than terminal hairs. At this growth phase, the epidermis becomes more papillated and acanthotic.
History and Physical
The lesions either appear at birth or shortly afterward. They have solitary smooth, yellow, well-circumscribed plaques with oval or linear configurations. Linear lesions often spread along the lines of Blaschko. Nevus sebaceus is typically an asymptomatic skin lesion. In the scalp, they are classically associated with overlying partial or total alopecia. At puberty, nevus sebaceus becomes more prominent. It takes on a verrucous or mamillated appearance secondary to the hormonal changes of the child. This evolution mirrors the histologic differentiation of normal sebaceous glands of the skin. The patient or their parents may present to the dermatology clinic for evaluation and potential removal due to its clinical appearance.
Evaluation
Nevus sebaceus is a clinical diagnosis; additional workup is typically unnecessary. The exception would be a child with nevus sebaceus syndrome or a large lesion over 10 cm which may be associated with central nervous system anomalies such as epilepsy or intellectual disability. In this case, appropriate referral to neurology or other specialists may be indicated.
Treatment / Management
The treatment and management of nevus sebaceus remain controversial topics. Because nevus sebaceus was previously thought to indicate a high risk for developing secondary carcinomas later in life, prophylactic excision was an acceptable treatment. However, research suggests the risk for developing secondary carcinomas is low, while the risk of developing secondary benign neoplasms is relatively high. Such benign growths include syringocystadenoma papilliferum and trichoblastoma. Therefore, surgical excision is considered an acceptable treatment for nevus sebaceus in late childhood, once the risk from general anesthesia lessens. Most secondary tumors arising in a nevus sebaceus occur in adults 40 years or older. This statistic is especially relevant as a cosmetic consideration regarding large and verrucous facial lesions during puberty. Shave removal is typically unsuccessful as it may not remove the entire lesion.[4][7][8][9]
Factors to consider before surgery depend on the size and location of the lesion. Most patients require general anesthesia, especially children.
Differential Diagnosis
The differential diagnosis of nevus sebaceus depends on the stage of development. In early infancy, the differential diagnosis may include aplasia cutis congenita or mastocytomas. Other differential diagnoses in later stages of development include congenital nevi, epidermal nevus, seborrheic keratosis, verruca, and early juvenile xanthogranulomas.
Prognosis
The prognosis of nevus sebaceus depends on whether it is benign or malignant at the time of diagnosis. Transformation of the benign lesion to a malignancy is said to occur in about 10% of cases, although some authors suggest that it may be much lower. Previously, the lesion was often misdiagnosed as a basal cell cancer when in fact it was a trichoblastoma. In rare circumstances, malignant changes have been observed in children under the age of five. Sebaceous cysts, once developed, do not regress and remain for most of adult life. The most common skin malignancy to grow in a nevus sebaceus is a basal cell cancer. On the other hand, the most common benign lesion to occur in nevus sebaceus is trichoblastoma.
Complications
The risk of malignancy is minimal and almost nonexistent in children.
Besides transforming into basal cell cancer, other tumors that can appear include keratoacanthoma, leiomyoma and apocrine cystadenoma. In extremely rare cases, a malignant transformation to eccrine proromas may occur. These are usually metastatic by the time diagnosis is made.
Consultations
Once a diagnosis of nevus sebaceus is made, the patient should be referred to a pediatrician and a dermatologist.
Deterrence and Patient Education
Patients should be taught that nevus sebaceus is a benign lesion that may present as a warty patch on the scalp.
The patient should be advised that transformation to malignancy is very rare and usually only seen in adults.
All patients should be asked to see a clinician when there are sudden changes in the color, texture or size of the lesion.
Patients living in rural areas or who appear to be noncompliant with follow up can be given the option of prophylactic surgical removal. This option will remove the risk of malignancy.
Pearls and Other Issues
Nevus sebaceus of Jadassohn is also referred to as organoid nevus. It is a congenital malformation described in 1895 by dermatologist Josef Jadassohn.
These congenital malformations are hamartomas of the pilosebaceous follicular unit which includes follicular, sebaceous, and apocrine components plus epidermal hyperplasia.
These growths most commonly form on the scalp, but may also appear on the forehead, face, or neck.
The prognosis of nevus sebaceus depends on whether it is benign or malignant at the time of diagnosis.
The treatment of these lesions is controversial, with options ranging from observation to early excision in childhood.
Enhancing Healthcare Team Outcomes
Nevus sebaceus of Jadassohn, also referred to as organoid nevus, is a congenital malformation described in 1895 by the dermatologist Josef Jadassohn. These congenital malformations are hamartomas of the pilosebaceous follicular unit. This unit includes follicular, sebaceous, and apocrine components, plus epidermal hyperplasia. These growths most commonly form on the scalp, but may also appear on the forehead, face, or neck. They undergo a growth phase during puberty due to hormonal changes in the patient's body. In adulthood, the growths may develop secondary neoplasms within them, most commonly trichoblastoma. These lesions are best managed by a dermatologist as they are not common. The treatment of these lesions is controversial, with options ranging from observation to early excision in childhood. The prognosis of nevus sebaceus depends on whether it is benign or malignant at the time of diagnosis. The treatment of these lesions is controversial, with options ranging from observation to early excision in childhood.