Neuroanatomy, Brain Veins
- Article Author:
- John Hufnagle
- Article Editor:
- Prasanna Tadi
- Updated:
- 7/31/2020 3:17:32 PM
- For CME on this topic:
- Neuroanatomy, Brain Veins CME
- PubMed Link:
- Neuroanatomy, Brain Veins
Introduction
The brain is a tremendously well-perfused organ, receiving up to 20% of the resting cardiac output. This blood flow reaches the brain via the internal carotid arteries and the vertebral arteries and ultimately gets drained by the internal jugular veins. To reach the jugular veins, the brain has an intricate network of venous sinuses that drain not only the brain parenchyma, but the meninges, eyes, and cerebrospinal fluid as well. The drainage pathways can be differentiated teleologically, as either superficial drainage to the dural sinuses, or deep drainage to the medullary veins and ultimately to the cerebral vein of Galen. These vessels are uniformly valveless and as such, freely communicate with each other, which can facilitate the spread of infectious pathogens. The cerebral venous system is also quite delicate and, as the brain is suspended in fluid, mild trauma or even sudden changes in velocity can cause rupture of the cortical bridging vessels, leading to a subdural hematoma.
Structure and Function
The cerebral veins function to drain the capillary network that supplies the brain with blood; this removes carbon dioxide and other metabolic wastes, and allows fresh blood to flow in to take its place. The cerebral veins drain the entire brain as well as the eyes, meninges, and part of the face via the pterygoid plexus. The dural sinuses, especially the superior sagittal sinus, also serve to drain the cerebrospinal fluid via the arachnoid granulations and it is by this process that the CSF ultimately returns to the bloodstream. Structurally, the veins of the brain have no muscular layer, and no valves, which differentiates them from their counterparts in the rest of the body and the lack of a muscular layer allows them to expand substantially. The only exceptions are the larger pial veins, which have a circumferential smooth muscle layer. The superficial dural sinuses have the added benefit of being supported by layers of dura mater, preventing them from being easily compressed if the intracranial pressure rises.
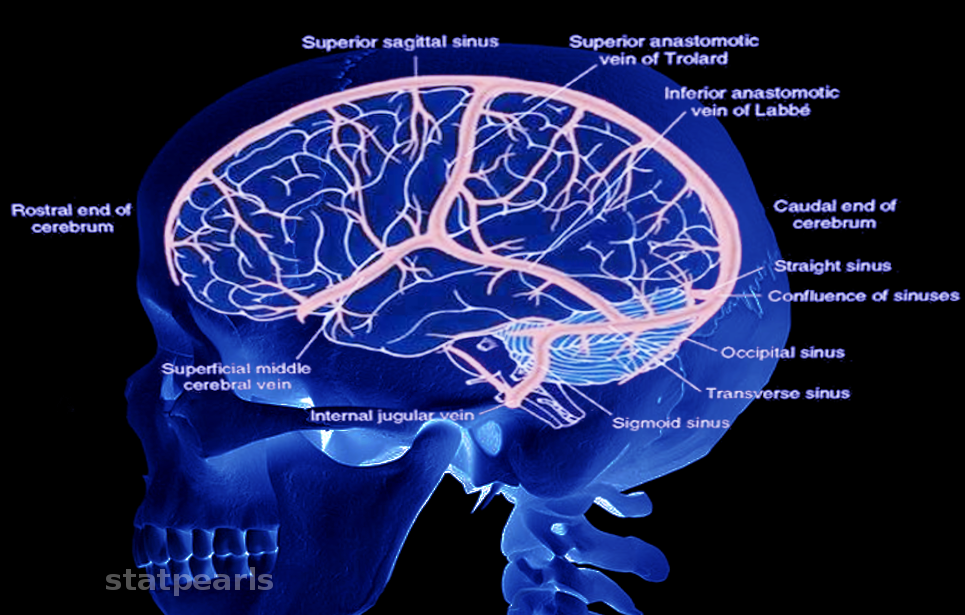
The venous anatomy of the brain is complex, and the first major investigation was only done by Okudera et al. in 1999. It divides into two groups: the superficial medullary or subcortical venous system and the deep medullary venous system based on whether blood from a given venule will drain to the superficial veins or the deep cerebral veins and ultimately the vein of Galen. The superficial medullary veins begin with subcortical veins that drain the outer cortex and flow into the pial veins sitting on the surface of the cortex. The pial veins converge and drain into the cerebral veins. These vessels are numerous and lie on the surface of the brain. The largest three are: the superficial middle cerebral vein lies over the Sylvian fissure, the vein of Trolard courses superiorly to the superior sagittal sinus, and the vein of Labbe drains into the transverse sinus. All cerebral veins typically drain to the nearest dural sinus depending on their location. The superiodorsal veins drain to the superior sagittal sinus, the posterior veins, and veins of the cerebellum drain to the transverse sinus, and the anterior veins can drain to the superior sagittal sinus, cavernous sinus, or the superficial middle cerebral vein. Upon reaching a dural sinus, the veins pierce the arachnoid and dura mater as bridging veins, and their contents drain into the dural sinus. The dural sinuses also collect blood from the minor meningeal veins and from the skull and scalp via emissary veins. The superior sagittal sinus travels caudally until it meets the occipital sinus over the cerebellum, forming the confluence of sinuses, blood then continues to the transverse sinuses.
The deep medullary venous system drains the deep cerebrum. The deep medullary veins are more extensive than the superficial medullary veins and the two only rarely anastomose via ‘transcerebral veins,’ relatively large veins traversing the entire cerebral parenchyma. The deep medullary system consists of venules lying in the white matter, roughly perpendicular to the lateral ventricles. They run parallel to each other and meet at three ‘zones of convergence’ in the parenchyma: the ‘hat-rack,’ ‘candelabra,’ and ‘palmate’ zones. They then converge a fourth and final time, forming the subependymal veins on the inner surface of the lateral ventricles.
Interestingly, it is this arrangement of the medullary veins that causes the characteristic periventricular and subcortical lesions in multiple sclerosis; as the leukocytes that cause demyelination extravasate from these veins. The subependymal veins join two additional groups of veins: the choroidal venous plexus and the thalamostriate veins. The latter systems drain the choroid plexus and much of the deep grey nuclei. When they merge with the subependymal veins, they form the internal cerebral veins. The left and right internal cerebral veins unite beneath the selenium of the corpus callosum to form the great vein of Galen. The vein of Galen, therefore, drains most of the cerebral white matter and deep gray nuclei.
The inferior anterior surface of the brain is drained primarily by the cavernous sinuses. These dural sinuses lie on either side of the sella and directly posterior to the orbits. They receive blood from the brain via the local cerebral veins, the eyes via the superior and inferior ophthalmic veins, and the skull and meninges by the sphenoparietal sinus and middle meningeal vein. Since it drains the middle meningeal vein, the cavernous sinus anastomoses with the maxillary vein. The cavernous sinus also drains the pterygoid plexus, which lies inferior to the cavernous sinus and anterior to the temporomandibular joint. The pterygoid plexus communicates with the facial vein and therefore drains the nose and upper lip. The cavernous sinuses also contain segments of the internal carotid artery, the sympathetic plexus, and cranial nerves III, IV, V1, V2, and VI.
The cavernous sinus drain in three directions. Superiorly it can drain to the superficial middle cerebral vein. Laterally they drain via the superior and inferior petrosal veins to the sigmoid sinus. Medially, both cavernous sinuses drain into the basilar plexus. The basilar plexus courses inferior to the brain, draining the anterior brainstem as it travels, then splits around the foramen magnum and joins the vein of Galen.
The great cerebral vein of Galen lies inferior to the splenium of the corpus callosum. Above the corpus callosum lies the inferior sagittal sinus, traveling on the inferior edge of the falx cerebri. The two meet behind to the splenium and form the straight sinus, which travels posteriorly until it joins the confluence of sinuses.
The confluence of sinuses lies midline, on the border of the cerebellum and occipital lobes. It receives the superior sagittal sinus superiorly, the occipital sinus inferiorly, and the straight sinus anteriorly. It then divides laterally into the transverse sinuses. The transverse sinuses travel downwards and become the sigmoid sinuses. The sigmoid sinuses then descend out of the skull through the jugular foramen as the internal jugular veins.[1][2][3][4][5][6]
Embryology
The mature venous system of the brain originates as a precursor venous system that develops and increases in complexity with the fetal brain. These primitive vessels receive little coverage in medical education texts, and their origin was first described in detail by Dr. George Linus Streeter in 1915. The cerebral veins begin development as undifferentiated mesenchyme known as the primary meninx. The meninx differentiates into a network of capillaries which then develop into a confluence of several vessels comprised of a thin layer of endothelium. They are believed to be of the same heterogeneous origin as the dura mater: both neural crest and mesoderm. The early major vessels are, from rostral to caudal: the anterior cerebral vein, the pro-otic vein, the vena capitis medialis, the vena capitis lateralis, the supra-optic anastomosis, and the posterior rhombencephalic veins. These vessels merge and form the anterior cardinal vein which drains to the primitive atrium. These primitive vessels are fated to develop into their more familiar adult structures. Of note, the anterior cerebral vein develops into the transverse sinuses, the pro-otic vein and vena capitis medialis develop into the cavernous sinus, which will drain the middle meningeal and ophthalmic veins, the vena capitis lateralis regresses, the posterior rhombencephalic vein and the supra-optic anastomosis form the sigmoid sinuses, and the anterior cardinal vein develops into the internal jugular vein. Additionally, the superior sagittal sinus derives as the space between the falx and dural layers along the midline.[7][8][9]
Physiologic Variants
The venous system of the body has considerable variation, and the brain is no exception. This variation is present in the structure and courses of the medullary veins in the parenchyma and the superficial cortical veins. In the deep medullary veins, variation can be noted in the location of subependymal venous connections as the drainage system consolidates and grows in size. The significant variation is also apparent in the superficial veins and dural sinuses. The most common variation of the major dural sinuses is a hypoplastic left transverse sinus, occurring in up to 21% of cases in one study. The same study found that the anterior segment of the superior sagittal sinus was atretic in just under 1% of patients. The superficial anastomotic veins (the superficial middle cerebral vein, the vein of Trolard, and the vein of Labbe) showed significant variation in their dominance, connection, and degree of development. The predominating vein was usually the combination of the superficial middle cerebral vein and the vein of Labbe, although the dominance of any one of the three, or even co-dominance of all three vessels, were observed and did not change between patients with different dominant hemispheres. The primary connection of the superficial middle cerebral vein was to the sphenoparietal sinus in 57% or the cavernous sinus in 19%. The vein of Labbe entered the transverse sinus in 80% of cases. Interestingly, these two veins, despite often being dominant, were each noted to be underdeveloped in 16% of cases.[10][11][12][13]
Surgical Considerations
The intracranial veins are generally less clinically relevant than their arterial counterparts. However, since severe diseases, such as cavernous sinus syndrome, can involve the veins, surgical solutions are necessary. The cavernous sinus itself is challenging to access, and multiple surgical routes are necessary depending on which structure the surgeon is trying to access. Examples are the transsphenoidal-transnasal route, the superior routes (involving a frontotemporal craniotomy), the lateral routes beneath the temporal lobe, and the transorbital route. As for the deep cerebral veins, surgical sacrifice has been shown to cause devastating complications, with one patient suffering extensive venous infarction of the cerebellum after sacrificing the superior petrosal vein. However, a 2013 review showed that careful and selective venous sacrifice is possible and safe in one or more veins.[14][15][16][17]
Clinical Significance
Cavernous Sinus Syndrome
Cavernous sinus syndrome results from obstruction, inflammation, or increase in pressure in the cavernous sinus. Some of the causes include thrombophlebitis, which can be caused by bacteria or fungus spreading from the nasal mucosa, paranasal sinuses, or after a skull fracture. A thrombus can form in any person with a hypercoagulable state, such as protein C or S deficiency, factor V Leiden, or use of combined oral contraceptive pills. Tumors can cause it as well, such as a locally extensive pituitary adenoma. Additionally, an internal carotid artery aneurysm can cause a similar syndrome. Should the aneurysm rupture, a carotid-cavernous fistula can form, causing increased pressure in the sinus. The symptoms of cavernous sinus syndrome reflect the effects on surrounding structures and the cranial and sympathetic nerves passing through the sinus. Involvement of the sympathetic plexus can result in a partial Horner syndrome. Since CN III, IV, and VI are affected, ophthalmoplegia can be expected. Notably, in a carotid artery aneurysm, CN VI is affected first, as it lies in closest proximity to the artery. Proptosis and even pain when pressing on the globe can also occur due to the increased pressure behind the eye. Diagnosis is usually through head imaging showing occlusion, thickening, or swelling of the sinus, often with engorgement of the ophthalmic veins as a result. Treatment involves treating any underlying infection or surgery to decompress the sinus.[18]
Venous Sinus Thrombosis
Thrombi occluding the dural sinuses are rare and typically associated with local trauma or a hypercoagulable state. The occlusion prevents drainage of any tributary veins and results in ischemic damage and increased intracranial pressure. Symptoms depend on the size of the occluded vessel and the area involved but can include focal neurologic deficits, gradually progressive headache, nausea, vomiting, visual disturbances, seizures, and other signs and symptoms of increased intracranial pressure, such as papilledema. Imaging with a CT scan is typically negative, although often an area of absent perfusion is seen in the posterior superior sagittal sinus in the shape of an empty triangle or ‘empty delta sign.’ Magnetic resonance venography is preferred and will show a lack of venous blood flow, confirming the diagnosis. Treatment involves anticoagulation.[19][20]
Subdural Hematoma
A subdural hematoma forms when blood collects beneath the dura mater in the skull; this most commonly occurs due to rupture of the bridging veins that connect the superficial cerebral veins to the major dural sinuses, especially the superior sagittal sinus. The venous blood then leaks out and presses against the brain parenchyma. Since the dural folds do not bind the blood, it is free to extend beyond the suture lines, producing the classic image of a ‘crescent-shaped’ collection of blood between the dural and the brain. This expanding pocket of blood can exert pressure on the brain, causing midline shift or even herniation. This condition can result from head trauma or even by rapid change in velocity (such as a fall that does not result in head trauma), this method of injury is seen most commonly in adults over 80 years of age. Subdural hematomas classically present in the elderly and other patients with cerebral atrophy in whom the bridging veins are already stretched, such as chronic alcoholics. It is also seen in abused infants (the ‘shaken baby syndrome’) as they have especially fragile vessels and is a recognized complication of antiplatelet therapy, anticoagulation, and long-term hemodialysis. The presentation is varied, from absolute loss of consciousness in massive bleeds following severe head trauma, to nearly asymptomatic. An asymptomatic subdural hematoma will delay presentation, and in the case of a sufficiently large bleed, may cause progressive memory loss, weakness, impaired gait, headaches, nausea, and vomiting. In this case, a patient may exhibit a further predisposition to falls and a recurrent acute subdural hematoma on top of the preexisting chronic case. A chronic subdural hematoma is primarily a disease of the elderly. Findings on imaging demonstrate a collection of blood surrounding part of the brain that can stretch around the suture lines, but not into the cisterns or ventricles; a midline shift and ventricular obliteration can accompany this condition. Treatment for subdural hematomas varies from conservative watchful waiting to burr hole surgery or craniotomy with drainage. The determinants of the exact course are patient factors and the size and extent of the hematoma.[21]
Developmental Venous Anomalies
Developmental venous malformations (DVAs), also known as cerebral venous angiomas, medullary venous malformations or cerebral venous malformations are an aberration of a venous structure in the cerebrum. The structure of DVAs is typically a single dilated cerebral vein with surrounding tributary veins draining into it, as opposed to several small separate veins. Simply put, it is a vein draining more than its fair share of parenchyma. DVAs affects approximately 3% of the population and are believed to be caused by aberrant development of a particular segment of a cerebral vein in utero, with compensation to allow the DVA to drain its watershed areas properly. DVAs are typically asymptomatic and pose no problems by themselves. However, they may be associated with a myriad of cerebral vascular pathology, including regional brain atrophy, white matter lesions, nearby bleeding, or calcifications. Additionally, in a study of 11 patients with Sturge-Weber syndrome found cerebral venous abnormalities, including developmental venous abnormalities, in each case. This finding is perhaps unsurprising, as Sturge-Weber is a disease of vascular development and is defined by leptomeningeal angiomatosis, causing an absence of subcortical veins which could lead to dilated deep medullary veins compensating for the additional drainage. Treatment of developmental venous abnormalities is conservative, due to their generally benign course and the risk of infarction in the vessels should surgery be attempted.[22][23][24][25]
Facial Venous Plexus Anastomosis
The facial venous plexus primarily drains the skin over the nose and of the upper lip. This venous network is valveless and drains to the facial vein. However, it also anastomoses with the pterygoid plexus, along with the veins draining the nasal mucosa. As these vessels are valveless, this allows for free communication between the nasal mucosa and epidermis of the face and the cavernous sinus and from there, the surface of the cerebral cortex. This arrangement is the rationale behind the term ‘danger triangle of the face’ comprising the nose and upper lip, where a pimple or blemish that is ruptured or irritated may cause pathogens to reach the cavernous sinus or cortex, potentially causing infection or cavernous sinus syndrome.