Heinz Body
- Article Author:
- Timothy Herman
- Article Editor:
- Muhammad Javaid
- Updated:
- 7/27/2020 9:04:56 AM
- For CME on this topic:
- Heinz Body CME
- PubMed Link:
- Heinz Body
Definition/Introduction
Heinz first described these in 1890, and so they were named Heinz bodies. Heinz bodies are indicative of oxidative injury to the erythrocyte. They are clumps of irreversibly denatured hemoglobin attached to the erythrocyte cell membrane. Although the precise mechanism is not entirely understood, the presumption is that amino acid substitutions in the beta-chains of the hemoglobin polypeptides allow them to precipitate within the red blood cell and form Heinz bodies.[1]
Heinz bodies are normally present in healthy cats, but their presence in other species is unhealthy. Heinz body formation can lead to three presentations.
Firstly extensive formation of Heinz bodies and attachment to membranes increases their rigidity and renders them susceptible to fragmentation in the spleen. The macrophages remove the damaged cells in the spleen, which results in the formation of bite cells. This increased destruction may lead to oxidant-induced hemolytic anemia.
Secondly, Heinz bodies result in the production of reactive oxygen species, which can cause intravascular lysis of RBCs leading to hemoglobinemia and hemoglobinuria.
Thirdly methemoglobinemia (brown plasma) can occur in animals from oxidant-induced injury of iron in hemoglobin (Fe+2 becomes oxidized to Fe+3 producing methemoglobin).
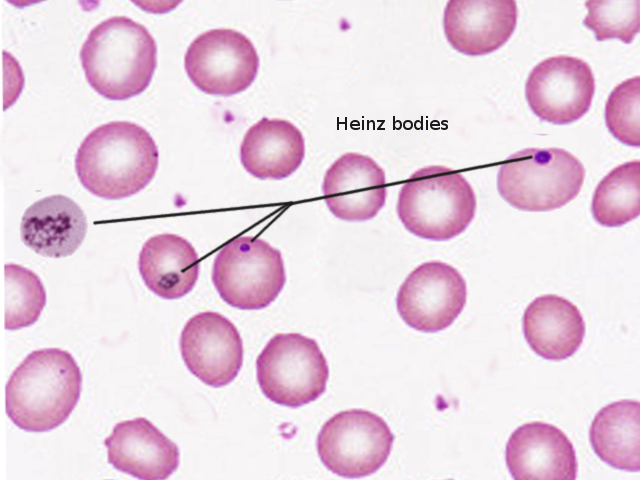
Heinz bodies may be quite small or rather large and prominent. In some instances, a single RBC may have several small Heinz bodies. Heinz bodies stain the same red-pink color of mature RBCs with routine Wright stains and stain pale basophilic with Diff-Quik stain. Otherwise difficult to see, they are easily observable in supravital stains like methylene blue.
On microscopy, Heinz bodies present as small, dark, round, basophilic masses. They are typically located near the inner membrane of the red blood cell.[2]
Issues of Concern
Heinz bodies are likely to cause hemolytic anemia, which can present with various symptoms including jaundice, dyspnea, tachycardia, hematuria, fatigue, and even hypotension. These symptoms must be recognized as early as possible to limit the severity of the anemia and its corresponding complications.[3][4][5]
Clinical Significance
Heinz body formation is an etiology of hemolytic anemia. Heinz body hemolytic anemia is usually associated with toxic exposure like propylene glycol, brassica species.
Cases may result from hereditary defects in the molecular milieu that acts to protect erythrocytes from oxidative damage. Heinz bodies may be present in patients with glucose-6-phosphate dehydrogenase (G6PD), or FAD f(adenine dinucleotide deficiency), i.e. methemoglobinemia.[6] it may also indicate unstable hemoglobin, e.g. HB Koln.
Oxidative damage can occur in red blood cells in various conditions, especially in patients experiencing diabetic ketoacidosis.[7]
In veterinary medicine, it commonly results from the consumption of foods containing thiosulfate consumed by cattle, dogs, and cats. A notable example is the consumption of sodium 2-propenyl thiosulfate, which can be present in boiled garlic.[8]
Drugs acting as oxidants also cause Heinz body formation, important examples being acetaminophen, vitamin K1, propafol, and phenothiazine drenches.
Mineral deficiency, for example, selenium, also increases susceptibility to oxidative damage and Heinz body formation.
The presence of Heinz bodies can ultimately result in hemolytic anemia, and the ability to recognize signs and symptoms of hemolytic anemia is the best way to maximize patient-centered care. Although hemolytic anemia often gets diagnosed by analyzing lab work, it is crucial to be able to recognize classic signs of anemia such as fatigue, dyspnea, paleness, jaundice, and/or hepatosplenomegaly. Being well-versed in identifying these clinical presentations maximizes patient safety and quality of care.[9] [Level 1]
There is no treatment for the oxidation induced anemia; its importance is for diagnostic purposes only.
Nursing, Allied Health, and Interprofessional Team Monitoring
When monitoring patients with Heinz bodies, it is most important to ensure they are not experiencing hemolytic anemia, which may present with jaundice, hepatosplenomegaly, tachycardia, hematuria, and fatigue. Although other symptoms may be present, it is also critical to monitor the lab work of these patients to ensure the hemolytic anemia is under control and undergoing monitoring accordingly.[9][10]