Wrist Imaging
- Article Author:
- John Copeland
- Article Editor:
- Doug Byerly
- Updated:
- 4/30/2020 7:13:16 PM
- For CME on this topic:
- Wrist Imaging CME
- PubMed Link:
- Wrist Imaging
Introduction
The wrist is one of the most complex joints in the human body, allowing for stability during movement in all three cardinal planes of the human body. Categorically considered a hinge joint like the elbow, the wrist has additional planes of movement and rotation thanks to robust anatomy. Made up of eight carpal bones, the radius, ulna, and five metacarpals, the number of articulations and degrees of motion are quite extensive. As with other joints, numerous ligaments and tendons connect and provide structural stability and movement of the osseous structures of the hand and wrist. The radial and ulnar arteries, as well as their terminal branches, provide the vascularity to the hand and wrist while the median, ulnar, and radial nerves are responsible for motor and sensory innervation.[1][2]
Trauma or other pathology, including degeneration, to any of these structures, can cause a wide range of pain and dysfunction that may not be easily diagnosed due to the inherent anatomic complexity. Perhaps it is no coincidence that the first human radiograph taken in 1895 by William Roentgen was that of the hand and wrist, though far from diagnostic in such primitive form. We are now fortunate to have advanced imaging techniques to assess and diagnose the pathology of this complicated anatomic structure. The purpose of the article is to provide insight into the various imaging modalities as they relate to imaging of the wrist in diagnosing pain and dysfunction from different types of pathology.[3]
Anatomy
The osseous anatomy of the wrist includes the distal radius and ulna, eight carpal bones, and the five metacarpals. See figure 1. The complexity of this three arc system creates multiple synergistic joints that allow the wrist a dynamic range of motion.[4]
The articular surface of osseous structures is covered with articular (hyaline) cartilage, a connective tissue composed of a dense network of collagen fibers resulting in tissue with tensile strength yet more flexible than bone. Together with synovial joint fluid, the hyaline cartilage provides a low friction surface for movement across joints and aids in shock absorption. The various articulations of the osseous structures of the wrist, which include long bones, carpals, and metacarpals, provide a wide range of motion, including various combinations of flexion, extension, ulnar, and radial deviation, supination, and pronation.[5]
An intricate array of intrinsic (carpal to carpal) and extrinsic (radius and ulna to carpal) ligaments binds the osseous structures and allows for compound motions. Each bone has specific connections to adjacent osseous structures that provide the overall balance of stability and movement for the wrist. Typical nomenclature of the ligaments describes the structures connected and the direction of their attachment either proximally to distally, or from the radial to ulnar aspect. For example, the scapholunate ligament attaches the scaphoid and lunate, referencing the specific carpals spanned, from radial to ulnar direction.[6]
The dominant stabilizing structure of the wrist is the triangular fibrocartilage complex (TFCC), located on the ulnar aspect of the wrist. The TFCC is composed of a triangular-shaped articular disc of fibrocartilage, which parallels the articular surface at the ulnocarpal joint with an attachment to the ulnar margin of the distal radius where the disc attaches directly to the articular cartilage of the distal radius. On the ulnar side, the disc has band-like fibrous attachments to the ulnar styloid and the fovea. In addition to the articular disc, the TFCC is composed of the extrinsic ligaments to include the dorsal and volar bands of the radioulnar ligaments, as well as the ulnar collateral, ulnotriquetral and ulnolunate ligaments. The extensor carpi ulnaris tendon and the ulnomeniscal homolog comprise the ulnar margin of the TFCC running along the ulnar margin of the ulnocarpal joint. TFCC extends the articular surface of the radius to include the surface of the ulna and serves to absorb load across the wrist joint. It is a major contributing factor allowing for forearm rotation, offering both flexibility and strength to the connection between the distal radius and ulna.[7][8]
The carpal tunnel or carpal canal is the space along the volar wrist formed between the arch of the carpal bones, which constitutes the floor, and the flexor retinaculum, which forms the roof. The flexor retinaculum is a connective tissue sheath bridging the gap from the scaphoid tubercle and trapezium to the pisiform and hook of the hamate. The median nerve and nine tendons traverse the tightly packed carpal tunnel, including the flexor pollicis longus, four flexor digitorum superficialis, and four flexor digitorum profundus.[9]
The ulnar or Guyon's canal is another tunnel along the volar wrist. It forms from the volar carpal ligament (roof), transverse carpal ligament (floor), the hook of the hamate (radial border), and an ulnar border comprised of the pisiform, pisohamate ligament and abductor digiti minimi muscle. The major structures within the canal include the ulnar nerve, ulnar artery, and ulnar vein.[10]
No fewer than one dozen extensor and flexor tendons traverse the wrist joint from their proximal muscle bellies to aid in wrist and hand movement. The flexor carpi radialis, flexor carpi ulnaris, and palmaris longus tendons pass through the wrist external to, but tightly associated with, the carpal canal. Figure 2.
Blood supply at the wrist is provided by means of branches from the dorsal and palmar carpal arches formed by the anastomosis of ulnar and radial arteries. Additionally, the anterior interosseous arteries supply portions of the wrist, particularly the articular disk of the TFCC. Of note, the retrograde blood supply to the proximal scaphoid from a single dorsal surface entrance point of the radial artery branches increases the risk of avascular necrosis and scaphoid nonunion after a fracture.[8][11][12]
Central nervous system communication derives from the median, radial, and ulnar nerves.[13] The median nerve is responsible for sensation to the volar aspect of palm and first three digits (thumb, index, middle) as well as the radial half of the 4th (ring). It also innervates the dorsal aspect of these digits from the proximal interphalangeal joints (PIP) through the tips. The median nerve and its branches are responsible for motor innervation to pronator teres, flexor carpi radialis, palmaris longus, flexor digitorum superficialis, flexor digitorum profundus, flexor pollicis longus, pronator quadratus, abductor pollicis brevis, flexor pollicis brevis, opponens pollicis, and the first/second lumbricals. The ulnar nerve supplies sensation to the volar and dorsal aspect of the 5th digit (little) and the ulnar portion of the 4th. Motor innervation by the ulnar nerve includes flexor carpi ulnaris, flexor digitorum profundus, palmar brevis, abductor digiti minimi, flexor digiti minimi, opponens digiti minimi, 3rd/4th lumbricals, and palmar/dorsal interosseous muscles. The radial nerve supplies sensation to the dorsal aspect of the thumb and wrist, as well as the 2nd to 3rd digits to the level of the PIP. It also innervates the radial aspect of the 4th to the level of the PIP on the dorsal side.
Plain Films
Plain film radiographs are the backbone of medical imaging and should be the first consideration of any wrist pathology for several reasons. Not only do radiographs offer low cost, non-invasive, and relatively quick results, but their relative familiarity across all medical professions also makes them a great initial choice for diagnosis after a thorough physical exam.[14][15] Additionally, radiographs often offer complementary information to more advanced imaging. For example, soft tissue calcifications such as hydroxyapatite deposition disease (HADD) are often more easily appreciated on radiographs.
Plain radiographs offer less ionizing radiation dose than other forms of imaging, such as computed tomography and fluoroscopy. Another advantage is the portability of x-ray equipment. Portable x-ray machines and imaging cassettes allow technologists to acquire images without transporting a patient to another department within a facility, expediting the opportunity for diagnosis in an emergency room and trauma situations.
Despite the relative simplicity and high yield properties of plain radiographs, there are some disadvantages compared to other imaging modalities. First, exposure to ionizing radiation slightly increases the overall lifetime risk of developing certain cancers, and their usefulness must be judiciously weighed against this risk. Additionally, the risk of damage at the molecular DNA level is magnified in tissues with high rates of growth or replenishment. That makes it slightly more risky for pregnant patients, children, and procedures imaging gonadal tissues. Overall, the benefit must outweigh the risk to proceed. It should be noted that the radiation dose of most radiographic studies, especially in the setting of the appendicular skeletal structures, is relatively low, as is the lifetime risk.[16] Radiographic imaging of the axial skeleton imparts a higher radiation dose and lifetime risk.
Plain radiographs cannot delineate and fully characterize soft tissue structures. Soft tissue damage such as ligamentous and tendon derangement is not always readily apparent on plain radiographs. When these types of injuries are identified, it is by inference of radiographic findings as the ligaments and tendons are not visualized on radiographs. Additionally, the static images produced by routine x-ray equipment do not provide much functional evaluation of joint structures. Weight-bearing or stress imagines provide more information regarding the functional alignment of osseous structures as well as evaluation of the joint space. Joint space narrowing is a radiographic sign of cartilage injury and osteoarthritis. Similarly, vascular flow or real-time motion kinematics are not properly evaluated.[17]
Examples of appropriate uses of plain film radiographs for wrist pathology may include:
- Trauma, fracture identification
- Anatomic alignment (osseous coalitions, advanced scapholunate collapse, dislocations)
- Limited fracture characterization (displacement, the involvement of physis, simple vs. comminuted fractures)
- Fracture follow-up assessment (fracture line, bone remodeling)
- Relative bone density
- Bone lesion identification and classification (internal matrix, cortical destruction)
- Gross soft tissue evaluation (edema/swelling/radiopaque foreign objects, some tendon injuries such as Achilles and patellar)
- Presence of and overall degree of degenerative change/arthritis
Computed Tomography
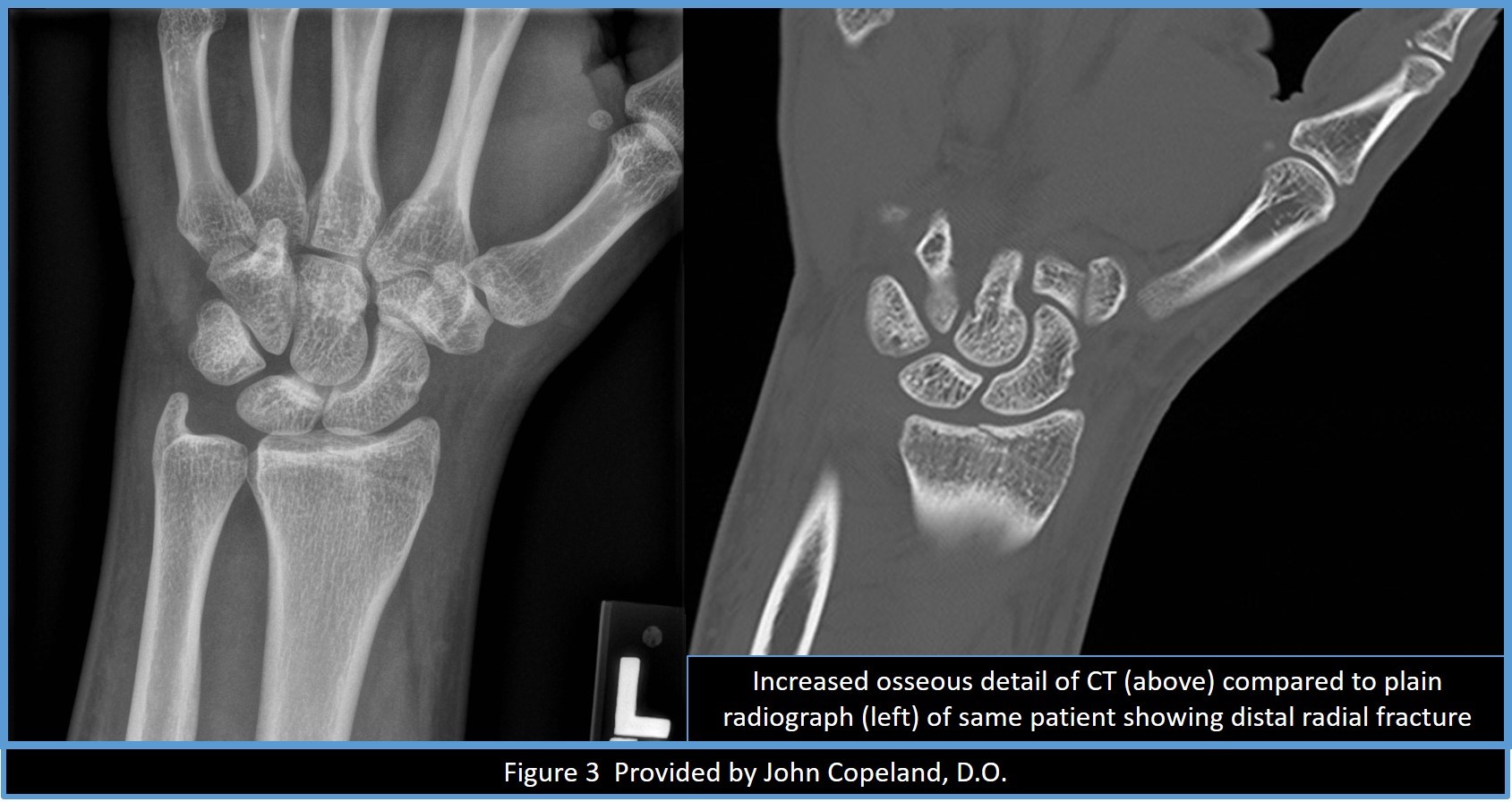
Computed tomography (CT) is the choice for further evaluation of wrist pathology after radiographs when osseous detail is important for diagnosis and treatment. See figure 3. Not only does it offer increased spatial resolution and boney detail, but it also allows users to view structures in multiple cross-sectional axes and even 3-D reconstructions when post-processing software is incorporated.[18][19][20][21]
Another advantage of CT is greater soft tissue delineation, though not to the level of magnetic resonance imaging (MRI). Sensitivity for TFCC injuries with CT is increased when paired with arthrogram injection before CT imaging. Additionally, when used with intravenous contrast, vascular structure and integrity can be evaluated as well as the assessment of fluid collections and infection. Last but not least, patients that are unable to undergo MRI scans due to indwelling ferromagnetic material can safely receive a cross-sectional evaluation with CT.[19][20]
The disadvantages of CT include increased ionizing radiation dose, increased imaging time required and thus the possibility of motion artifact, decreased availability, beam-hardening artifact when imaging through metal hardware and possible difficulty of patient positioning of the wrist within the CT gantry without also exposing the torso or head or forcing the patient into uncomfortable positioning with the arm fully extended over the head while lying down. See figure 4.[8][18][20][22]
Examples of appropriate uses of CT for wrist pathology may include:
- High-quality osseous detail with multiple planes of view
- Enhanced evaluation of anatomic alignment
- Fracture characterization, especially when complex, occult, and as a surgical planning tool
- Degree of fracture nonunion or healing
- Post-surgical changes
- Carpal tunnel syndrome
- Soft tissue delineation (vessels, hematoma, soft tissues masses, tendon entrapment in trauma patients)
- TFCC, ligament and compartmental integrity when paired with pre-scan joint injections (arthrograms)
- Vascular assessment when used with intravenous contrast agents (anatomy and integrity)
- Cross-sectional evaluation when MRI is not an option (indwelling metal, availability, claustrophobia)
Magnetic Resonance
Magnetic resonance imaging (MRI) is a complex use of controlled magnetic field interactions on imaging subjects that is more sensitive than any other imaging modality at delineating soft tissue structures and properties. MRI characterizes normal from abnormal soft tissues based on expected signal intensity of the particular anatomic structure after interactions with the magnetic field. The contrast between ligaments, tendons, fat, and muscle on MRI is much better appreciated than on CT imaging and nearly imperceptible on plain film imaging. Tissues can also be further characterized for their physical properties with the use of diffusion and perfusion sequences. MRI is the test of choice for evaluating vertebral osteomyelitis, soft tissue tumors, and soft tissue injuries such as tendon and ligament injuries.[8][18][19][23][24][25]
Additionally, there is no ionizing radiation used to acquire MRI images, avoiding a potential increase in lifetime risk for cancer. Finally, some angiographic information is available with MRI imaging using intravascular contrast agents or time of flight techniques.[16][26][23]
Despite the obvious superiority of soft tissue characterization over other imaging modalities, there are also disadvantages to MRI, and it should not be used as a primary diagnostic tool. Again, physical exams and plain film evaluation are useful in developing the next best step in the diagnostic pursuit and provide complementary information.
One disadvantage is the expense of the imaging equipment and the associated increased expense to the patient. The cost is often prohibitive for smaller facilities to support dedicated MRI access. Stand-alone imaging centers are often used, and wait times may exceed weeks in high volume communities. One contributing factor to the decreased availability of MRI scheduling is the time required to acquire an MRI study. This time factor also increases the likelihood of motion degraded studies on children, impaired patients, those with pain that increases with remaining recumbent for up to an hour at a time, and anyone with involuntary movement disorders. Typically, musculoskeletal MRI examinations last 20 to 30 minutes, longer if administering IV contrast, while the completion of CT examination can occur in minutes without arthrogram.[25][26]
Another reason MRI may not be best for every situation may be patient induced limitations, such as claustrophobia. MRI imaging takes longer than other modalities, and the small bore of the magnet can be an unpleasant, if not an impossible task for some patients. Another unfortunate limiting factor includes a patient's physical ability, or lack thereof, to properly position and maintains the wrist within the scanning field. Those with limited shoulder movement, obesity, and spinal problems will likely have more difficulty lying down and extending their wrist over their heads into the bore of the magnet.[8] In cases of advanced osteoarthritis, MRI is of limited use as no significant additional beneficial information is obtained from the examination, with no change to current treatment plans.[27]
Since the core of MRI is the use of magnets, retained or surgically implanted ferromagnetic objects are likely an absolute contraindication or may be conditional with strict imaging parameters established by the manufacturer. The magnetic field can also have an adverse effect on certain older cardiac pacemakers and programmable ventriculoperitoneal shunts. These devices may require placement in a disabled or MRI compatible mode by a trained person such as a manufacturer representative. Metallic artifact from retain or implanted metal can interfere with the diagnostic quality of the imaging.[20]
Examples of appropriate uses of MRI for wrist pathology may include:
- Occult fracture
- Stress fracture
- Edema in bone and soft tissues
- Inflammatory arthropathy
- Assessment of cartilage
- Carpal tunnel syndrome
- Bone lesion characterization (osseous and soft tissue neoplasms)
- Tendon pathology (tendinosis, tear, subluxation, tenosynovitis)
- Bursitis/intersection syndrome
- Muscle tear
- TFCC injury (sensitivity increased when paired with arthrogram injection technique)
- Non-osseous coalition
- Avascular necrosis, Kienböck disease
- Osteomyelitis, particularly within the vertebral column
Ultrasonography
Ultrasonography (US) is a relatively inexpensive, readily available, non-ionizing radiation imaging method that uses sound waves to evaluate the human body. Many advantages exist for US wrist imaging, including the fact that there are essentially no contraindications to ultrasound. Metallic hardware severely limits MRI and CT due to artifacts, limitations not incurred with US. Additionally, US allows dynamic imaging of structures in real-time, helpful for evaluation of ligaments and tendons throughout their range of motion. The abilities to individually investigate specific tendons and other distinct wrist structures are possible and especially important given the complexity of the wrist anatomy and compartments. Color and power Doppler imaging allows the differentiation of soft tissue structures by determining the presence of flow in the vasculature or hyperemic tissue.[28][29][30][31]
Ultrasound is unique from other imaging modalities in its reliance on the skill of the technologist or clinician performing the study. An incredible amount of anatomic knowledge is required to evaluate and interpret wrist US images accurately. Also, understanding imaging artifacts, such as anisotropy, normal variations, normal and abnormal appearance of anatomic structures, and familiarity with the equipment (probe selection and machine settings), is essential for both obtaining and interpreting US images. Often a review of US images in a vacuum (interpreter not present for examination) severely limits the interpretation of the images. Ultrasounds diagnostic strength lies in its ability to assess soft tissue structures. It is of limited or no use for assessment of osseous abnormalities and pathology.[28][32][29][30][31]
Examples of appropriate uses of US for wrist pathology may include:
- Soft tissue masses
- Tendon pathology (tendinosis, tear, tenosynovitis)
- Ligamentous injury
- Real-time dynamic evaluation (tendon subluxation)
- Carpal tunnel syndrome
- General vascular flow
Nuclear Medicine
Nuclear medicine (NM) imaging uses intravenously injected radioactive tracers that provide diagnostic data according to the metabolic activity of differing tissues. The radiotracers are attached to specific carrier molecules to target different areas and activity levels in the body. Areas of increased bone remodeling at fracture sites, cancerous overgrowth, and active infection can be targeted in this manner. Bone scintigraphy is the most widely used NM technique for bone imaging. Radiotracers with avidity to osteoblastic activity show increased areas of uptake and thus point to areas of increased turnover such as fractures and neoplasms. Other radiotracers with avidity for leukocytes aid in the detection of infectious and inflammatory processes, including characteristic findings in complex regional pain syndrome or hardware complications. NM is mainly advantageous because of the ability to detect functional changes that appear earlier than anatomic changes detected by other imaging modalities.[18][33][25]
Single-photon emission computed tomography (SPECT/CT) is another NM option for musculoskeletal imaging. It combines the functional assessment of NM with the anatomical assessment of CT. SPECT/CT is often used to increase the diagnostic accuracy of suspected cancerous lesions and stress injuries. Risks and benefits for this type of imaging are the combinations of the collective modalities.[34][35][36]
Perhaps the largest disadvantage of NM is the poor quality anatomic resolution provided by the detection of the radiotracer. NM images do not show sharp osseous details. Another disadvantage of NM includes the radiation dose to the patient and persons within close proximity. Unlike other modalities that pass ionizing radiation through the body to form an image, nuclear medicine detects the amount of radiation that emanates from the radiotracers that are delivered within the body. The patient then becomes the source of radiation and continues to have low levels of radioactivity after the imaging is complete. Radiation dose differs according to the half-life and amount of the specific radiotracer used and the physiologic elimination through urine or stool. In NM techniques such as bone scintigraphy, the entire body receives a radiation dose, not just the imaged area, as is the case in CT and radiographs. The radiotracers are created in laboratories, both on and off-site of most imaging facilities, and the associated costs and availability can be prohibitive. To allow radiotracer uptake in the areas of interest also increases the procedure time. Patients usually end up spending several hours at the facility for a single NM study and, in some cases, may require further imaging several days after radiotracer administration. Another time-based constraint is the delay needed to adequately allow for the physiologic healing process, osteoblastic activity, to initiate. For example, an acute fracture will not be evident on bone scintigraphy until the healing response has initiated.[18][25]
Examples of appropriate uses of NM for wrist pathology may include:
- Assessment of osseous metastasis (osteoblastic neoplasms more than osteolytic)
- Occult fracture (subacute to chronic)
- Stress fracture
- Osteomyelitis
- Bone lesion characterization (aggressive processes tend to be more metabolically active thus higher uptake of radiotracer)
- Avascular necrosis
- Complex regional pain syndrome
Angiography
Conventional angiography is usually performed within an interventional radiology suite closely resembling an operating room. It is performed under sterile conditions and uses intravascular contrast to image basic vascular anatomy and integrity. The use of fluoroscopic imaging systems provides dedicated, small fields of view while allowing for the versatility and computer software required for digital subtraction vascular imaging. Dedicated angiography is useful for evaluating blood supply in cases of avascular necrosis, such as Kienböck disease. In this same manner, physicians can interrogate aneurysms, pseudoaneurysms, anatomic variants, or compromises in blood flow at specific areas of interest.[37][38][39] In addition to provided diagnostic evaluation, angiography based techniques have been developed for the treatment of vascular pathologies such as coiling aneurysms, stenting, angioplasty of stenosis, or embolization of neoplastic processes.
Similar to direct (conventional) angiography, CT, and MRI angiography techniques also use intravenous contrast agents to aide in the assessment of vascular structures and pathology. The timing of contrast administration and imaging by the technologists provide the radiologist a cross-sectional view of various anatomy with the vascular system enhanced by contrast (venous versus arterial). Like dedicated angiography, general anatomic information and vessel integrity are visualized, but with the added benefit of increased clarity of surrounding anatomy compared to conventional angiography.[39]
CT and MRI angiography, however, does not have the benefit of image-guided intravascular treatment. CT guidance of percutaneous procedures such as biopsy and therapeutic injection is common, but endovascular CT image guidance is not commonly performed.
Examples of appropriate uses of angiography for wrist pathology may include:
- Vascular integrity
- Vascular supply (variant anatomy, stenosis, etc.)
- Aneurysm evaluation and treatment
- Pseudoaneurysm evaluation
- Raynaud phenomenon
- Occupational/vibrational induced pathology
- Imaged guided tumor embolization and chemotherapy administration (such as uterine artery embolization for treatment of uterine fibroids)
Patient Positioning
Patient positioning is relatively straight forward for plain films and ultrasound. The patient should sit on a chair or stool next to the imaging table for radiographs and assume a comfortable position on a gurney or chair with the wrist supported on a pillow or tray for ultrasound evaluation. Patient comfort is paramount for maximum patient cooperation in remaining motionless for plain films and ergonomically accessible to the technologist for US imaging. Nuclear medicine positioning for dedicated wrist imaging is similar to plain film or ultrasound. The patient rests their hands on a gamma camera while sitting in a nearby chair.[28][29][30]
Three standard plain film views are the typical protocol in most facilities, the posteroanterior (PA), PA oblique, and lateral. Dedicated scaphoid views should be requested if there is a history of snuffbox tenderness or fall on an outstretched hand.[11][29][30] See figure 5.
Additional supplemental views can be tailored to assess specific structures. Flexion, extension, and radial and ulnar deviation views can assess gross motion and decrease the superimposition of the carpals. The standard PA oblique view provides an additional evaluation of the distal scaphoid and radial styloid process, while an AP oblique view projects the pisiform without a significant overlap of the triquetrum.[40]
Patient positioning for dedicated angiography, typically performed in a surgical suite, likely requires the least precision of the modalities. For these studies, the patient lies supine with the wrist next to, but not on, the torso.[37]
The gantry and bore of CT and MRI equipment present some challenges when positioning a patient for wrist imaging. Ideally, the wrist is placed in the center of the imaging field without having additional anatomic structures nearby. For example, the patient's wrist and arm should not be imaged while resting naturally at the patient's side. This would place the abdomen/pelvis in the field of view, increasing radiation exposure in CT and creating an opportunity for artifacts in both CT and MRI. Getting a patient to comfortably lie on the examination table with their arm extended over the head can be difficult, painful, and sometimes impossible for obese patients, those in poor health, and anyone with incidental shoulder pathology.[8] (See figure 4.)
Clinical Significance
There are several things to consider before choosing an appropriate imaging modality for the wrist. A good simple rule is to start with plain radiographs for a baseline assessment. Remember to request dedicated navicular views to assess for "snuffbox" tenderness, especially with a fall on outstretched hand (FOOSH) mechanism of injury. Further imaging decisions are influenced by the clinical symptoms and findings, both positive and negative, seen on plain film imaging. Consider the limitations of artifacts on cross-sectional imaging if retained ferromagnetic material is imaged. Plain films may give you the best assessment. In the setting of advanced arthrosis (osteoarthritis or inflammatory arthropathy), advanced imaging such as MRI or CT may not change the treatment plan. In these cases, consultation with a specialist before imaging may be indicated to decrease unnecessary imaging.
An additional consideration is that of contrast allergy screening before requesting angiography. It may be appropriate to forego contrast all together or possibly pre-medicate using standard ACR protocols before administering the contrast.[41]
As always, screen for retained metal, cardiac pacemakers, and programmable ventriculoperitoneal shunts before ordering MRI imaging. Patients with implantable devices should be provided documentation describing the specific device (manufacturer), limitations, and imaging conditions for MRI compatibility. Just because a patient was previously scanned without complication does not indicate the device is safe/compatible for MRI imaging. All MRI protocols are not equal; on a previous scan, the device may not have been in the isocenter of the MRI scanner and thereby not exposed to the same magnetic fields and/or electrical currents. Also, while the implanted device or hardware may be MRI compatible, it may interfere with adequate imaging, and a different modality may be more appropriate.
In closing, here are a few specific wrist pathologies with suggested imaging considerations:
- Trauma, including suspected distal radius and ulna fractures - Start with plain films and consider further characterize with CT if the fracture is complex. Follow up, and post-surgical imaging can be accomplished with plain film and limited CT as needed. If the patient remains symptomatic despite conservative treatment, repeat radiographs in 10 to 14 days can help to assess for signs of osseous remodeling. Alternatively, a rapid MRI protocol (limited exam) could be performed to evaluate for occult fractures if patient management will be impacted.
- Scaphoid fracture - Always remember to request a specific scaphoid view with plain radiographs. Additional imaging with CT for boney detail, osseous alignment, and evaluation of healing progression are sometimes required. NM bone scintigraphy or MRI are both options for the assessment of occult fractures in the appropriate clinical setting. NM has the highest sensitivity for detecting occult fractures, but less specificity, leading to overtreatment more often than when CT and MRI are used. MRI has the added benefit of evaluation of surrounding soft tissues and lack of exposure to ionizing radiation.
- Arthritis - Plain films can identify arthritis and degenerative changes and even differentiate inflammatory arthropathy such as rheumatoid from osteoarthritis. Serial radiographs help follow the progression of the disease. Again, CT or MRI can further characterize the processes as needed. Advanced imaging is appropriate in the assessment of early inflammatory arthropathy or osteoarthritis in young patients who may benefit from cartilage replacement procedures. CT or MRI is rarely indicated in advanced osteoarthritis.
- Scapholunate dissociation - This condition is initially identifiable with plain films and further characterized by MRI.
- Carpal dislocations - Again, plain films are used to identify the particular pathology, and CT or MRI are used to characterize the extent of ligamentous involvement and surgical planning further.
- Distal radioulnar joint dislocation or instability – Initial evaluation with radiographs t assess osseous alignment and coexistent fracture followed by MRI to assess ligamentous involvement.
- Osseous and non-osseous carpal coalition - Osseous coalitions are identifiable on plain film. If a non-osseous (fibrous) coalition is suspected, MRI or CT can better identify the presence of such findings while MRI may identify associated soft tissue or bone marrow edema, which would support a clinical diagnosis of a symptomatic fibrous coalition.
- Kienböck disease and avascular necrosis - Serial imaging with plain film can identify and follow the progression. MRI is more sensitive and specific for early detection. NM can exclude but is not specific for the diagnosis even if the scan is positive.
- TFCC tear - As usual, a good place to start is with plain film assessment. Radiographs are helpful for the diagnosis of soft tissue mineralization such as HADD or chondrocalcinosis, which can be difficult to appreciate on MRI. Additionally, unsuspected fracture or arthritis may be identified on radiographs and thereby explain ulnar sided pain without the need for advanced imaging. CT arthrogram or MRI with or without arthrogram can identify the presence and type of TFCC tear or identify other potential causes of ulnar sided wrist pain such as tenosynovitis or intersection syndrome.
- Carpal tunnel syndrome - There is a dedicated plain radiograph to assess the osseous carpal tunnel, but it is limited in identifying the most pathologic causes of this process. Start with plain films, specifically requesting a carpal tunnel view, then proceed to cross-sectional imaging with CT if osseous pathology is expected or US and MRI for soft tissue evaluation. MRI or US can identify imaging findings to support the diagnosis of carpal tunnel syndrome such as median nerve enlargement as well as identify important anatomic variants essential to safe surgical planning such as a persistent median artery. Advanced imaging may also identify soft tissue causes for carpal tunnel, such as accessory muscles or soft tissue masses like ganglion cysts.
- Humpback deformity of the scaphoid - Again, this process will be evident on most plain film imaging studies (lateral view particularly) and further characterized with CT for surgical treatment planning.
- Osteomyelitis – Radiographs are relatively insensitive for early osteomyelitis however are complementary to advanced imaging. Radiographs may show periostitis or cortical destruction. Both MRI and NM imaging are more sensitive for the detection of osteomyelitis than radiographs. MRI has the advantage of being able to identify the extent of the process, coexistent septic arthrosis, and soft tissue involvement (cellulitis, fasciitis, or abscess).
- Metastasis – Osseous lesions can be identified on radiographs when there is advanced destruction; however, the infiltrative marrow-replacing process can be occult on radiographs. Soft tissue masses can soft times be appreciated on radiographs, especially if there are associated osseous remodeling/changes. CT and MRI have a higher sensitivity for the identification of metastasis and better evaluates the extent of disease.
- Bone lesions – Radiographs help determine the presence and type of matrix present in a bone lesion (chondroid versus osteoid). Some bone lesions have a characteristic/pathognomic appearance on radiographs, and further imaging is not indicated, such as non-ossifying fibroma (NOF). As previously described, advanced imaging such as CT and MRI better evaluates the extent of disease (i.e., joint or soft tissue involvement) as well as better characterization of the lesion, thereby narrowing the differential diagnosis and allowing for the determination of indication for tissue sampling. CT and MRI also aides in surgical and biopsy planning.
"The view(s) expressed herein are those of the author(s) and do not reflect the official policy or position of Brooke Army Medical Center, the US Army Medical Department, the US Army Office of the Surgeon General, the Department of the Army, the Department of the Air Force, or the Department of Defense or the US Government."
(Click Image to Enlarge)