Optic Nerve Sheath Ultrasound
- Article Author:
- Evan Richards
- Article Editor:
- Dana Mathew
- Updated:
- 7/31/2020 2:27:23 PM
- For CME on this topic:
- Optic Nerve Sheath Ultrasound CME
- PubMed Link:
- Optic Nerve Sheath Ultrasound
Introduction
The use of point-of-care ultrasound (POCUS) has expanded considerably over the past two decades allowing for enhanced and swift evaluations, rapid triage, improved diagnostic capabilities in austere situations, and real-time assessment of focused clinical questions in critically ill patients in the intensive care unit (ICU).[1] Emergency medicine physicians have led the way in the establishment and education of bedside use of ultrasound. In 2001, the American College of Emergency Physicians (ACEP) published the first Emergency Ultrasound Guidelines to clarify the primary indications, the scope of practice, training, and continuing education regarding the use of emergency ultrasound.[2] These guidelines have continued to expand alongside the ever-growing use of ultrasound. They have been adopted by several other specialties, especially in the application of “procedural ultrasound” to assist in real-time guidance of vascular access, peripheral nerve blockade, and pre-surgical evaluations.[3][4] The main difference between POCUS and dedicated ultrasound exams is the ability to answer a focused clinical question rapidly, to facilitate serial examinations in the setting of clinical deterioration, or to guide a bedside procedure rather than provide a detailed report with the grading of pathology.[2][5] With small, portable models of ultrasound becoming available, advanced diagnostics are becoming more accessible in remote environments and on the battlefield. Physicians and advanced paramedical providers in these settings are becoming trained to perform extended focused assessment with sonography in trauma (eFAST), optic nerve sheath ultrasound (ONSUS) for the evaluation of intracranial hypertension, inferior vena cava collapsibility assessments for the evaluation of volume status, and countless other examples of image-guided procedures.[6][7] The focus of this article will be on optic nerve sheath ultrasound for the diagnosis, monitoring, and management of elevated intracranial pressure (ICP).
Anatomy and Physiology
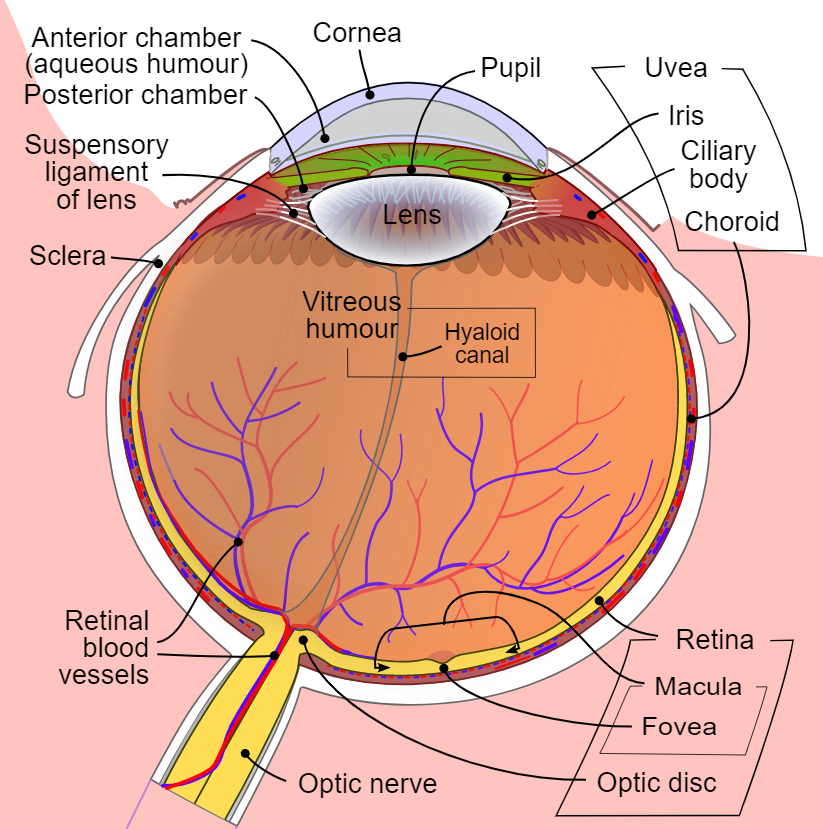
The eye is an ideal configuration for ultrasound imaging as it is superficial with well-demarcated fluid-filled structures that serve as an excellent medium for ultrasound beam transduction. At least a basic understanding of ocular anatomy is required to perform an ONSUS, and identification of anterior structures will increase success in measuring the optic nerve sheath in the correct plane.
The eyeball rests in a membranous sac called the Tenon capsule, surrounded by periocular fat, soft tissue, and the orbital walls. It attaches via the corneoscleral junction and the optic nerve, with extraocular muscle tendons piercing the Tenon sac, inserting into the sclera, and allowing for eyeball mobility on multiple axes. Two fluid-filled structures that require identification in the study include the anterior chamber (AC) and posterior chamber (PC), which are separated by the lens and both harbor anechoic fluid. Posterior to the PC is the retina with a hyperechoic nervous membrane.[8] Posterior to the retina and optic disc, one can identify the optic nerve by its anechoic core, flanked by a hyperechoic sheath on the medial and lateral borders in the transverse plane. The optic nerve can be thought of as an outpouching of intact brain tissue with the intraorbital component being fully encapsulated by dura, arachnoid, and pia matter, allowing the optic nerve sheath to transmit cerebral spinal fluid and fluctuate in size based on changes in intracranial pressure.[9][10] The bulbous portion of the optic nerve, approximately 3 mm posterior to the globe, appears to be the most distensible and sensitive to changes in ICP based on in-vivo models of elevated ICP and artificial creations of elevated ICP in cadaveric models.[9][11]
Indications
Ocular ultrasound can be performed for various reasons, including vision loss, headache, and trauma. It can be very beneficial in identifying or excluding retinal detachment, foreign bodies, lens dislocation, vitreous hemorrhage, and other superficial abnormalities that can cause loss of eyesight. ONSUS is usually performed in the setting of suspected or confirmed traumatic brain injury (TBI), intracranial hypertension, or optic neuritis.[12] ONSUS has the advantage of being non-invasive and avoids the risk of infection, hemorrhage, or ionizing radiation that are inevitable with intracranial monitors and computed tomography (CT).[13] ONSUS can also be used as a tool to help “rule out” elevated ICP in non-acute trauma settings such as troubleshooting of a malfunctioning intraventricular device, before or following lumbar punctures, or while evaluating the safety of neuraxial anesthesia in patients with a previous history of elevated ICP. It should be emphasized that these readings should be evaluated in the overall clinical context, as such applications are not well studied or validated.[14][15][16][17][18]
Contraindications
Equipment
The advantage of ONSUS is that it can be performed with most ultrasound equipment that is abundantly available in emergency departments and ICUs throughout the United States. There are commercially available high-frequency ocular ultrasound units designed for dedicated studies of the eye, but most conventional ultrasound units with a high frequency (7-10 MHz or higher) linear array probes are sufficient to visualize the optic nerve with the closed eye technique.[21][22] Additional equipment required may include a clear sterile intravenous catheter adhesive to create a barrier and ultrasound gel as a conduction medium.
Personnel
Typically, ONSUS can be performed by an individual and requires no additional assistance in patient positioning. Depending on space constraints, it can be useful to have an assistant familiar with ultrasound to capture images, adjust depth, gain, and other functions to optimize imaging.
Preparation
Awake and alert patients should be briefed on the procedure. Obtunded, intubated, or heavily sedated patients should have a gross eye evaluation for signs and symptoms of globe rupture or hyphema. If there is evidence of globe rupture, including visible conjunctival or scleral defect, severe chemosis, 360-degree conjunctival hemorrhage, hypotony, or total hyphema, the procedure should be aborted to avoid further herniation of intraocular contents, and an ophthalmologist should be consulted.[23][19][24] It can be beneficial to instruct awake patients to “look ahead” with a closed eye or to examine the eye orientation in obtunded patients before the start of the procedure to orient the ultrasound beam in the transverse plane and avoid oblique slices of the optic nerve. Some practitioners will apply petroleum jelly or ophthalmic ointment to the eyes to avoid air trapping before the application of a clear plastic adhesive dressing. Ultrasound gel should be applied liberally to the adhesive before scanning.[25] The patient position should be dictated by comfort and ease of examination, but will typically be done in the supine to 30 degrees “head up” position. Although theoretical concerns may exist for changes in ICP and ocular nerve sheath diameter (ONSD) relative to patient position and ventilator settings, these changes do not appear to manifest in in-vivo models. Several small studies have shown there to be no significant change in ONSD with changes to patient position, the elevation of positive end-expiratory pressure, or even the artificial creation of pneumoperitoneum in laparoscopic surgeries.[26][27][28][29][30]
Technique
After the application of a sterile dressing over a closed eye and copious ultrasound gel, the high-frequency ultrasound transducer should be placed over the eye with little to no contact with the sterile dressing in the transverse plane. The sonographer’s hand should be placed on a non-compressible surface (the patient’s nose, midface, or forehead) to avoid direct globe pressure, discomfort, and distortion of anatomy. Small movements nasally and temporally followed by caudad and cephalad should be executed trying to capture the optic nerve sheath in the same plane as the AC, PC, and lens to avoid obliquing of the image. Once the anechoic streak posterior to the optic disc is visualized, the image should be captured, and measurements can be taken from the saved image. The optic nerve is relatively cylindrical and symmetric, theoretically making a single view acceptable for measurement.[12] However, the dogma of “one view is no views” should be applied in all ultrasonographic studies, and another image should be captured in the sagittal plane. After measuring 3mm posterior to the globe, use electronic calipers to measure the distance of decreased echogenicity between the hyperechoic demarcations of the sheath. A large discrepancy between images captured in separate planes should alert the sonographer to possible artefactual or off-axis errors, and he/she should rescan in both planes. Once optimal images are captured in two planes, the mean should be determined to estimate the true ONSD. Both eyes should be scanned, and bilateral measurements should be considered.
If difficulty in acquiring an image during the ultrasound study is encountered, one should try to center the focal ultrasound beam transversely through the plane of the lens. The contralateral eye can be assessed to estimate the location and orientation of the pupil on the studied eye. Increasing the volume of an ultrasound gel buffer can improve the quality of the image. Increasing the gain can be helpful to enhance discernment between the actual nerve sheath and nerve. If available, color doppler can help visualize the retinal artery near the posterior globe as a reference point.Once the optic nerve sheath diameter is determined, it requires evaluation in the overall clinical context. Earlier studies have most commonly used a cutoff of 5.0 mm with excellent sensitivity as well as positive and negative predictive values, but cutoffs correlating to elevations of ICP greater than 20 mm Hg have varied from less than 5 mm to greater than 6 mm in different papers. One meta-analysis of 12 studies that compared optic nerve sheath values to CT evidence of elevated ICP yielded a specificity of 92.3% and a sensitivity of 95.6% utilizing a 5 mm cutoff in adult patients.[31]
Complications
ONSUS is safe and benign in the absence of an open globe. If an open globe injury is suspected, however, there is potential for further ocular injury, and the study should not proceed without consultation or assistance from an ophthalmologist.[19][20] It is worth noting that despite the reasonably good sensitivity and specificity shown in several studies, imagining the optic nerve sheath in the traditional visual axis, and even the mean measurements of the ONSD captured in the transverse and sagittal plane, have been questioned by several authors. Copetti et al. challenge that conventional views of the optic nerve sheath in several studies are more likely to be an artifact (potentially acoustic shadow cast from the lamina cribrosa) rather than the optic nerve itself. False positives, created by artifact or excessive pressure on the globe itself, could result in unmerited treatment, invasive monitoring, or additional unindicated studies. Copetti suggests utilizing color doppler to identify the retinal artery and measuring the optic nerve from the lateral position.[32]
Clinical Significance
There are broad applications of ONSUS in both advanced medical centers and battlefield environments. It is often difficult and potentially life-threating to transport critically ill intensive care unit patients to radiology suites. The mortality rate of inter-hospital transfer of critically ill patients has been reported as high as 2%, with adverse event rates as high as 68%.[33] Given that several studies have shown that CT scans usually result in therapeutic changes in only about half of all cases (39% to 68%), only judicious use of out of ICU radiographic studies should be considered.[34][35] Head CT accounts for more than 25% of ICU inter-hospital transports, and depending on the indication, ONSUS may be a modality in improving the decision making process for obtaining such imaging.[36] If a multisystem trauma patient with a known, stable intracranial hemorrhage and known baseline ONSD experiences neurological decline in the ICU, it could potentially be worthwhile to perform serial ONSUS on the patient to rule out intracranial hypertension or herniation if the risks of transport are significant and an evolution of the hemorrhage without intracranial hypertension would not change management. This is why it is so paramount to perform early and frequent ONSUS in patients at risk for developing increased ICP as a significant change in ONSD is far more suggestive of changes in ICP than a single absolute number.
Medics and physicians have used ultrasound in a myriad of environments, including high altitude, polar, battlefield, and in-flight expeditions, when other imaging is not readily available.[7] Traumatic brain injury (TBI) remains a common battlefield injury with over 200000 DoD reported cases between 2010 to 2018. Over 80% of these TBIs are classified as mild and do not require neurosurgical intervention, but evaluation in austere locations can be difficult.[37] Not only does ONSUS provide the ability for rapid triage and the minimally invasive evaluation of intracranial hypertension in an equivocal clinical setting, but it also provides useful data for the early medical treatment of intracranial hypertension while arranging evacuation to definitive neurosurgical care. Though ONSUS is not specifically mentioned by the most recent Joint Trauma System Clinical Practice Guideline on Traumatic Brain/Severe Head Injury (2 March 2017), the authors note that “treatment of known or suspected intracranial hypertension remains a cornerstone of therapy in patients with severe brain injury.” Further recommendations are that after conservative management (head of bed elevation 30 to 45 degrees, SBP goals greater than 100 to 110 mm Hg, normoventilation with PaCo2 35 to 40 mm Hg, blood glucose less than 180 mg/dl, PaO2 greater than 60 mmHg, seizure prophylaxis, etc.) treatment with 3% saline with a target serum sodium goal of 150 to 160 should be instituted if there is no contraindication. When utilizing invasive ICP monitoring, a treatment goal of less than 22 mmHg is often cited.[38][39] Since invasive ICP monitors require some neurosurgical expertise, and traditional cutoffs of ONSD of 5 mm typically correlate to an ICP greater than 20 mmHg, ONSUS could be utilized as an aid in the decision-making process to start hypertonic therapy and as a real-time monitor of clinical effects.
Enhancing Healthcare Team Outcomes
ONSUS remains a relatively new modality for the assessment of ICP. Initial studies have shown that it is an extremely easy skill to acquire and can be performed bilaterally in less than 5 minutes by experienced operators.[12][31] Interestingly, research regarding the training of ONSUS in non-physician Special Operations Combat Medic (SOCM) trainees with minimal to no ultrasound experience has shown that after a 5-minute tutorial, trainees were able to obtain statistically non-significant measurement differences in ONSD when compared to expert physicians.[13] Additional research has suggested that novice ultrasound users can obtain proficiency with this scan in as little as 25 exams, while an experienced sonologist might become proficient with as few as ten scans.[12] Given the safety profile of surface ultrasound and its expansion of utility in physician and non-physician training, the skill of ONSUS can be acquired and utilized by the entire health care team.[13] [Level 1]
Nursing, Allied Health, and Interprofessional Team Interventions
In the right clinical setting or environment, ONSUS could provide enough information to institute neuroprotective measures or medical management in anticipation of further imaging, evacuation, or neurosurgical intervention. All members of the healthcare team should understand the ramifications of an elevated or increasing ONSD and should familiarize themselves with ICP lowering techniques.
Nursing, Allied Health, and Interprofessional Team Monitoring
ONSUS can be taught to virtually any medical professional even with limited ultrasound experience.[13] This may include paramedical, nursing, physician assistant, and physician providers. In many medical centers that offer neurosurgical services, there is not a neurosurgeon “in-house“ 24/7. Therefore, initial evaluation and interim monitoring will often be the responsibility of emergency medicine, intensive care, and nursing providers. There is a considerable utility in teaching this modality to any team that will commonly care for neurosurgical or critically ill patients.
(Click Image to Enlarge)