Neuroanatomy, Autonomic Nervous System Visceral Afferent Fibers and Pain
- Article Author:
- Terrence Sanvictores
- Article Editor:
- Prasanna Tadi
- Updated:
- 10/15/2020 8:42:27 AM
- For CME on this topic:
- Neuroanatomy, Autonomic Nervous System Visceral Afferent Fibers and Pain CME
- PubMed Link:
- Neuroanatomy, Autonomic Nervous System Visceral Afferent Fibers and Pain
Introduction
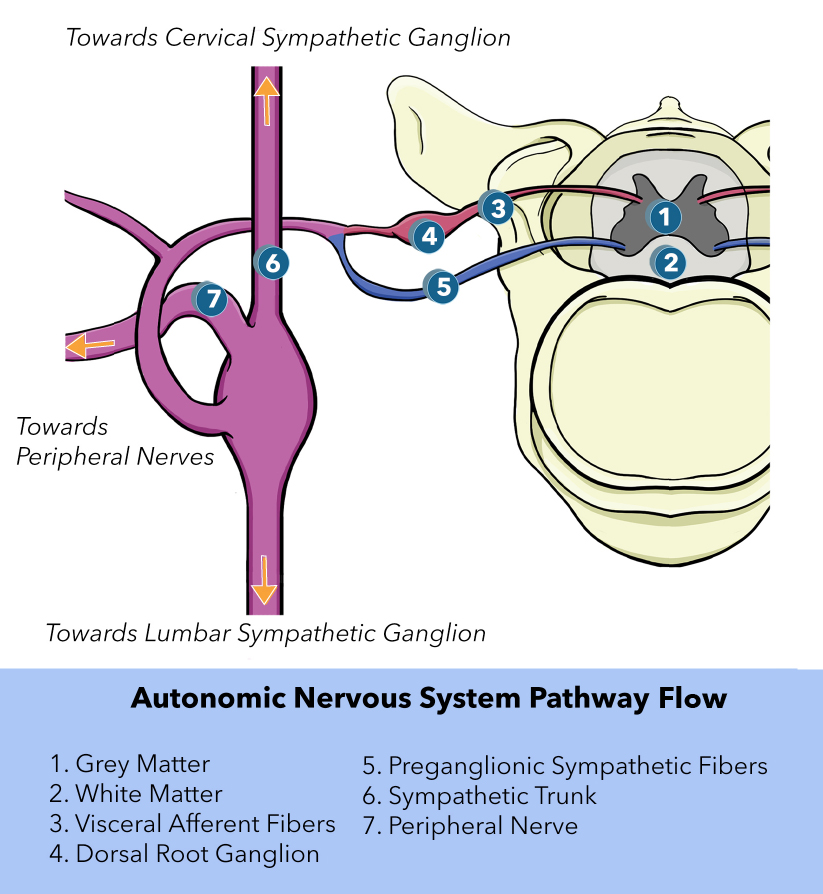
The autonomic nervous system (ANS) consists of general visceral efferent (GVE) fibers that create a motor response due to general visceral afferent (GVA) fiber stimulation. Although general visceral afferent fibers are part of the ANS, they are not classified as part of the sympathetic or parasympathetic system. However, these visceral sensory nerves often colocalize within sympathetic and parasympathetic nerves.[1] GVA fibers carry sensory impulses from internal organs to the central nervous system (CNS). Stimuli that activate GVA fibers include hunger, blood pressure, organ distention, and visceral inflammation. These afferent fibers allow the body to monitor the internal environment and adjust effector organs as necessary to maintain homeostasis.
Structure and Function
GVA fibers are primarily made of unipolar neurons. Each of these neurons is comprised of a cell body, an axon, and dendrites. The unipolar cell body of a GVA fiber can be found somewhere along a cranial nerve or in the dorsal root of the spinal cord. The cell body controls all the functions of the neuron and allows information to pass between the dendrites and axons. The axon is a long, tubular structure that conducts electrical impulses away from the cell body. Dendrites are tree-like projections that receive input from other cells and transmit this information to the neuronal cell body. Furthermore, these dendrites make up the receptive field that allows the neuron to detect specific changes in its surrounding environment.
Visceral afferent fibers are supported by Schwann cells. This support cell is a type of glial cell that supplies nutrients to peripheral nerves and has a role in nerve regeneration.[2] Schwann cells also insulate (myelinate) the axons of neurons from the peripheral nervous system by forming the myelin sheath.[3] This sheath is not continuous, which leaves unmyelinated gaps along the axon called nodes of Ranvier. Together, the myelin sheath and nodes of Ranvier improve the axonal conduction velocity resulting in a faster response time.
Three types of sensory receptors can activate GVA fibers: mechanoreceptors, nociceptors, and chemoreceptors. Each of these receptors detects a specific stimulus and additionally has a differing set of nerve fibers associated with them. Mechanoreceptors respond to mechanical pressure or physical deformation.[4] They receive their innervation through type II or III A-delta sensory fibers. Nociceptors detect pain and are innervated by type III and IV C fibers.[5] Chemoreceptors detect chemical changes (i.e., pH, carbon dioxide, and oxygen levels).[6][7] Cranial nerves innervate this latter receptor type.
Embryology
The nervous system initially arises from neural plate development.[8] An indentation, called the neural groove, eventually appears along the neural plate midline. As neurulation progresses, the neural groove deepens while the neural folds (the borders of the neural plate) converge on the dorsal midline to create the neural tube. This neural tube becomes the future site of the CNS, while neural crest develops on the roof plate of the neural tube. Cells from the neural crest undergo a transition from epithelial to mesenchymal cells, where they divide from the neuroepithelium and migrate through the periphery. From this point, those neural crest cells differentiate into varied cell types, which include cells of the PNS.[9] Further differentiation of PNS cells gradually leads to the development of GVA fibers.
Blood Supply and Lymphatics
Vasa nervorum vessels are the main blood supply for GVA fibers. These small arteries branch off from adjacent blood vessels and generally supply nutrients for each peripheral nerve.
Nerves
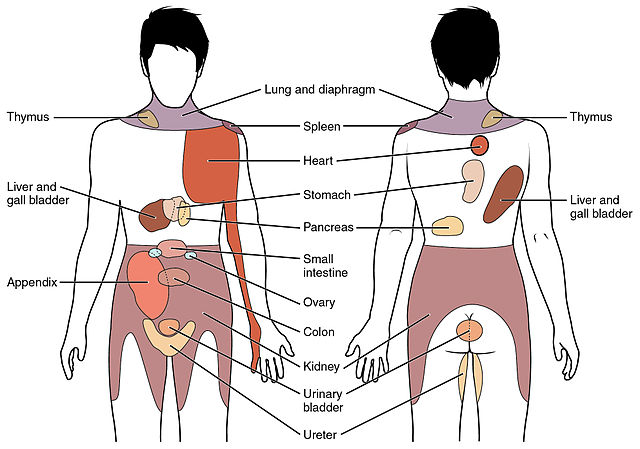
Once the sensory receptor is activated, the GVA impulse travels through unipolar neurons to reach the CNS. When the GVA fiber reaches the dorsal horn of the spinal cord, it terminates on a second-order neuron. These neurons then ascend upwards into the brain for further processing. Normally, visceral afferent activity does not reach the level of consciousness. However, if the visceral afferent activity is pain related, it can reach the level of consciousness. Visceral pain is frequently felt in a remote area from the location of the organ; this is known as referred pain. The chart at the end of this article provides more information about where referred pain appears for specific organs.
The cranial nerves with GVA fibers are the facial nerve (CN VII), the glossopharyngeal nerve (CN IX), and the vagus nerve (CN X). The facial nerve has a small amount of GVA fibers and primarily uses sensory neurons in the geniculate ganglion.[10] The glossopharyngeal nerve provides GVA fibers to the carotid sinus, carotid body, and other structures.[11]
The carotid sinus is found proximal to the internal carotid artery and possesses baroreceptors sensitive to blood pressure, while the carotid body is located at the bifurcation of the carotid artery with chemoreceptors that mean O2 levels. Fibers from both the carotid sinus and carotid body terminate on the solitary nucleus. Other areas that are innervated by GVA fibers of the glossopharyngeal nerve include mucosal membranes that line the inner surface of the middle ear, the Eustachian tube, the tonsils, posterior third of the tongue, and the posterior/upper surfaces of the pharynx. Fibers from these areas contain cell bodies in the inferior ganglion of CN IX and terminate in the nucleus of the solitary tract.
The vagus nerve has GVA fibers in the tongue, larynx, pharynx, trachea, esophagus, lungs, bronchi, stomach, heart, and intestines.[12] With regards to the lungs, GVA fibers help regulate the depth of breathing. In the heart, the vagal fibers innervate the aortic arch baroreceptors. Finally, chemoreceptors of the abdomen, heart, bronchi, and carotid body are innervated by vagus nerve GVA fibers as well.[13] All these vagal fiber cell bodies can be found within the inferior ganglia. The central processes of these neurons enter the medulla and terminate on the nucleus of the solitary tract.
Muscles
Stimulation of GVA fibers influences the motor response of their respective GVE fibers. These visceromotor fibers either innervate smooth muscle, cardiac muscle, or glands.
Physiologic Variants
The sensitivity of receptors associated with GVA fibers can affect the body's ability to maintain homeostasis. Upregulation or downregulation of these receptors can also change the intensity of the signal propagated through the afferent fiber. This intensity becomes especially important when it affects the perception of referred pain.
Understanding variations in nerve anatomy is vital, especially for accurate nerve conduction studies.[14] This knowledge becomes increasingly important for patients that need to undergo surgery. In general, correctly mapping a patient's nerve variants can reduce surgical risk.
Surgical Considerations
Denervation of GVA fibers can be the product of surgical treatment or as an accident from an invasive intervention. A disorder with a denervation treatment is carotid sinus syndrome, which is caused by overactive carotid sinus baroreceptor stimulation.[15] This syndrome can cause temporary loss of consciousness and recurrent dizziness. Surgical denervation of the carotid sinus leads to a decrease in sympathetic and vagal baroreflex sensitivity. However, it creates an increase in the variability of blood pressure without leading to chronic hypertension.[16]
Clinical Significance
Diabetic neuropathy is a form of nerve pathology that may occur for those with diabetes. High blood sugar not only interferes with a nerve's ability to send signals but can also weaken the walls of the vasa nervorum blood vessels that supply nerves with oxygen and nutrients. Diabetic neuropathy can affect the nerves of the autonomic system, especially GVA fibers, which can result in decreased blood pressure regulation and gastroparesis.[17] GVA fibers affected by diabetic neuropathy reduce their corresponding GVE fiber response.
General knowledge says that referred pain occurs because multiple primary sensory neurons converge on a single ascending tract in the spinal cord. When painful stimuli appear from visceral receptors, the brain is not able to distinguish between the visceral signals and signals that come from somatic receptors, which causes the brain to interpret that the pain is coming from somatic regions (i.e., skin, skeletal musculature, and bones) of the body rather than the visceral regions (i.e., spleen, kidney, and heart). For example, patients with angina pectoris, a type of cardiac pain, experience referred pain to the chest and upper left arm.[18] Another example is patients with temporomandibular disorder (TMD) can have referred pain to the teeth or other sections in the orofacial area.[19] Areas of referred pain can be cross-referenced against dermatome charts to help identify the visceral organ sending pain signals.
(Click Image to Enlarge)