Anterior Cord Syndrome
- Article Author:
- Nathaniel Pearl
- Article Editor:
- Laurence Dubensky
- Updated:
- 8/10/2020 10:54:42 PM
- For CME on this topic:
- Anterior Cord Syndrome CME
- PubMed Link:
- Anterior Cord Syndrome
Introduction
Anterior cord syndrome is an incomplete cord syndrome that predominantly affects the anterior 2/3 of the spinal cord, characteristically resulting in motor paralysis below the level of the lesion as well as the loss of pain and temperature at and below the level of the lesion. The patient presentation typically includes these two findings; however, there is variability depending on the portion of the spinal cord affected. Other findings include back pain, or autonomic dysfunction such as hypotension, neurogenic bowel or bladder, and sexual dysfunction.[1] The severity of motor dysfunction can vary, typically resulting in paraplegia or quadriplegia.
Anterior cord syndrome is caused by ischemia within the anterior spinal artery (ASA), which supplies blood to the anterior 2/3of the spinal cord. The ASA forms from the bilateral vertebral arteries at the foramen magnum. It runs as an uninterrupted artery within the anterior median sulcus of the spinal cord to the conus medullaris. Radicular arteries enter the spinal canal through the intervertebral foramen and primarily supply the nerve roots; however, some also anastomose and contribute to the ASA. The largest of these radicular arteries is the artery of Adamkiewicz, which most commonly arises off of a left intercostal artery between T9-T12 but can vary anatomically. The ASA gives off small sulcal and penetrating arteries that enter the body of the spinal cord to supply blood.[2]
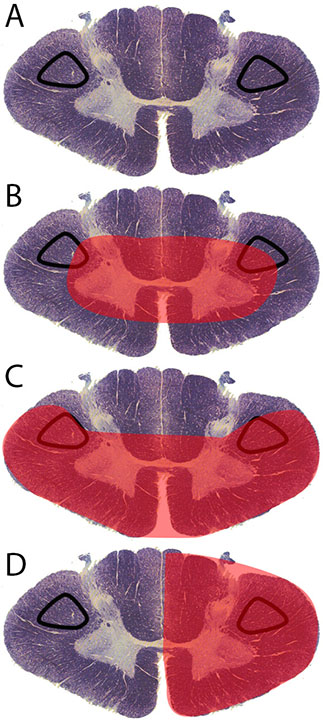
The anterior spinal artery supplies blood to the bilateral anterior and lateral horns of the spinal cord, as well as the bilateral spinothalamic tracts and corticospinal tracts. The anterior horns and corticospinal tracts control the somatic motor system from the neck to the feet. The lateral horns span T1-L2 of the spinal cord and house the neuronal cell bodies of the sympathetic nervous system. The spinothalamic tracts relay pain and temperature sensory information. The anterior spinal artery, with a few radicular artery contributions, is the sole source of blood supply to these areas of the spinal cord via its sulcal and penetrating arteries.
Ischemia of the ASA causes symptoms consistent with the dysfunction of these tracts. Since the ASA is formed from the more cephalad vertebral arteries and runs caudally, the higher the location at which ischemia occurs, the more widespread or severe the symptoms will be. Since the lateral horns are located only between T1-L2 of the spinal cord, autonomic symptoms are not always present if ischemia does not involve this region.[1] Proprioception, vibratory sense, two-point discrimination, and fine touch are not affected in anterior cord syndrome. These sensations are under the control of the dorsal column of the spinal cord, which is supplied by two posterior spinal arteries running in the posterior lateral sulci.[3]
Etiology
The root cause of anterior cord syndrome is ischemia of the anterior spinal artery. Thus, the etiology of anterior cord syndrome is very wide, in that it includes any procedure or disease process that can limit blood flow to this region of the vasculature. The most common cause of anterior cord syndrome is iatrogenic, namely thoracic and thoracoabdominal aortic aneurysm repair. Several factors during surgery can contribute to ischemia of the cord, including hypotension, cross-clamping of the aorta, increased spinal canal pressure, and occlusion of arteries feeding the cord.[4][5][6] Aortic dissection is a rare cause of spinal cord ischemia due to occlusion of branch vessels of the aorta, which include radicular arteries that help to feed the ASA.[7]
Other causes include hypotension secondary to other disease processes such as cardiac arrest, atherothrombotic disease, emboli, vasculitis, and other disorders affecting blood vessels, sickle cell and other hypercoagulable diseases, AV malformation, intervertebral disc herniation, and cocaine use.[8]
Epidemiology
Epidemiologic data on the subject of anterior cord syndrome is sparse. There are a limited number of studies on cord infarction as a whole; estimates are that cord infarction accounts for approximately 1.2 percent of all strokes.[9] The incidence of spinal cord infarction has been estimated to be 3.1 per 100,000 persons or 7600 people per year in the United States.[10] It is also of note that anterior cord syndrome is the most common pattern of spinal cord infarction.[8]
History and Physical
Due to the ischemic etiology of anterior cord syndrome, symptoms are typically acute in onset. Patients present with acute motor dysfunction as well as the loss of pain and temperature sensation below the level of infarction. These symptoms are almost always bilateral because both halves of the anterior spinal cord receive vascular supply from one midline anterior spinal artery. Depending on the location of infarction, the severity of motor dysfunction varies typically from paraplegia to quadriplegia.
Often the location of infarction includes the lateral horns within levels T1-L2 of the spinal cord, causing autonomic dysfunction, the most common manifestations being neurogenic bowel/bladder requiring bladder catheterization, hypotension, and sexual dysfunction. Acute onset of back pain is also a common symptom of cord infarctions in general and usually localizes at the level of the infarction.[11][12][13] It is important to note that there have been rare reported cases of anterior cord syndrome with unilateral symptomatology; this may be due to occlusion of unilateral sulcal arteries or collateralization from one posterior spinal artery.[13]
Evaluation
MRI is the primary imaging modality in the diagnosis of anterior cord syndrome. T2 hyperintensities within the region of the anterior horns are the hallmark finding. These hyperintensities on the sagittal view appear as thin “pencil-like” lesions extending vertically across several spinal levels. On the axial view, these hyperintensities appear as two bright dots, one within each anterior horn, resembling “owl’s eyes” in appearance. If imaging is obtained in the early stages of development, edema will be present and can cause the spinal cord to appear expanded in the region of infarction. Sometimes, signs of vertebral body infarction can be identified near the area of question, increasing the specificity of imaging for cord infarction.[13][14][15] MRI also serves the purpose of ruling out other causes of myelopathy, namely any compressive pathologies.
Patients with history and clinical findings consistent with anterior cord syndrome with positive MRI findings likely do not need further testing. However, other testing can rule out alternative diagnoses, as well as determine the underlying etiology that has caused their cord infarction. Additional imaging tests can rule out aortic or vertebral artery dissection, multiple sclerosis, or look for sources of embolism. Lumbar puncture and CSF testing can help to look for infection or inflammatory disease. Blood and urine tests can rule out infectious, hypercoagulable, atherosclerotic, inflammatory/rheumatic, or drug-related etiologies.
Treatment / Management
The most common etiology of anterior cord syndrome is aortic surgery. A protocol exists to reduce ischemia affecting the spinal cord after aortic surgery. It involves creating incremental increases in the patient’s mean arterial pressure by using IV fluids to increase intravascular volume and vasopressor medications to increase systemic vascular resistance. A lumbar drain is also placed to remove the cerebrospinal fluid. These interventions should increase blood flow to the affected region of the spine by optimizing vasculature as well as reducing overall pressure within the spinal canal.[16][17]
For atherothrombotic or embolic etiologies of anterior cord syndrome, thrombolysis is not yet considered standard of care. However, throughout the literature, there have been several acute cord ischemia patients treated with intravenous thrombolysis within 4.5 hours of symptom onset with rapid improvement in neurologic symptoms and no hemorrhagic complications. There is a theory that thrombolysis for this condition can be an effective treatment within a time-frame similar to stroke patients, but further studies on safety and efficacy are needed.[18]
Ultimately, the underlying cause of anterior cord syndrome should be the focus of treatment; this may be surgery to correct an aortic dissection, or immunosuppression therapy to treat vasculitis. Once cord infarction has occurred, symptomatic management is also paramount. This management could include fluid or pressor support for neurogenic hypotension, intubation, and mechanical ventilation for high cervical infarctions that affect the diaphragm or bladder catheterization for neurogenic dysfunction.
Long term sequelae of hospitalization must be addressed as well, including the risk of deep vein thrombosis and pressure sores in an immobilized patient, as well as gastrointestinal stress ulcers sometimes found in cervical infarctions. Physical and occupational therapy are also crucial in the process of regaining motor function in these patients.
Differential Diagnosis
- Central cord syndrome
- Dorsal cord syndrome
- Brown-Séquard syndrome
- Conus medullaris syndrome
- Cauda equina syndrome
- Transverse myelitis
- Guillain-Barré syndrome
- Multiple sclerosis
- Spinal epidural abscess
- Epidural hematoma
- Disk herniation
- Spinal cord neoplasm
- Meningitis/encephalitis
Prognosis
The overall mortality rate for spinal cord infarction has reportedly been between 9 and 23%, and the majority of deaths occur shortly after the initial injury.[5] Etiology is also important, in that patients with aortic dissection/rupture or with high cervical lesions are at greater risk of death. Survivors will have a varying degree of functional motor and sensory dysfunction. Two crucial prognostic factors are the severity of symptoms at initial presentation, and the amount of improvement in the first 24 hours.
More severe presenting symptoms and lack of significant improvement in the first 24 hours leads to a much poorer prognosis. Female sex and old age are two additional poor prognostic factors identified. Studies have shown that in less severe cases, favorable outcomes with improvement in neurologic function are possible and that a small number of patients regain their full walking ability. Functional improvements can slowly develop over several years post-injury.[5][19]
Complications
The majority of life-threatening complications occur shortly after the initial infarct or during the hospitalization period. Hypotension can occur due to the involvement of the lateral horns containing sympathetic neuronal cell bodies. Respiratory failure is a possibility in high cervical infarctions due to involvement at the level of the phrenic nerve, which innervates the diaphragm.
High cervical infarctions can also cause bradycardia requiring treatment with atropine or electrical pacing. Since patients typically have a significant motor impairment, prolonged immobilization can easily lead to deep vein thrombosis or pulmonary embolism.
Other complications during the hospitalization period include neurogenic bowel and bladder, pressure sores, and gastrointestinal stress ulcers. Survivors must handle a myriad of long-term complications, including functional motor and sensory dysfunction, chronic pain, spasticity, and bowel/bladder/sexual dysfunction.
Deterrence and Patient Education
Many of the etiologies causing anterior cord syndrome result from preventable disease processes. Educating patients about primary disease prevention is important in the avoidance of this syndrome. Aortic surgery is the most common cause of anterior cord syndrome, which can be a result of many pathologies, including aortic aneurysm or dissection. Atherosclerosis leading to thrombosis, as well as an embolus, are also common causes. Preventable risk factors for these diseases include hypertension, dyslipidemia, diabetes, and smoking.[20][21][22]
Patient education should focus on smoking cessation and the development of a healthy lifestyle through exercise and proper nutrition habits. If primary prevention fails and patients do develop these risk factors, secondary prevention is needed through further lifestyle guidance as well as medical management to maintain these conditions in a well-controlled state. If patients do develop cord infarction, continued strict management of these conditions can help prevent reoccurrence or continued functional decline. Ultimately, physical and occupational therapy, as well as psychiatry, play a significant role in the patient’s return to functional independence in regards to motor function, social health, and quality of life.[23]
Enhancing Healthcare Team Outcomes
Anterior cord syndrome is often a severe, life-changing disease. It affects multiple organ systems throughout the body and thus requires a team approach to optimally care for the patient. Emergency department providers must be able to quickly recognize the clinical signs and move to confirmatory imaging as well as treatment.
Neurologists play a vital role in the evaluation and treatment of spinal cord injury, as do vascular surgeons if an aortic etiology is suspected. Nurses will be able to identify and prevent developing complications such as pressure sores, urinary retention, or deep vein thrombosis. Pharmacists manage the multiple medications that patients with cord infarction may often require, helping to avoid developing complications of the spinal cord injury.
Physical and occupational therapy play an important prognostic role, helping the patient with rehabilitation and improvement of their functional motor status. Overall lifespan and functional independence of patients with spinal cord injury have made significant improvements over the years, and this is a result of improvements across a wide variety of fields coming together to enhance patient care.[24] [Level 5]