Carbimazole
 | |
| Names | |
|---|---|
| Trade names | Neo-mercazole, others |
IUPAC name
| |
| Clinical data | |
| Drug class | Thioamide[1] |
| Main uses | Overactive thyroid[2] |
| Side effects | Fever, rash, joint pain, low white blood cells, pancreatitis[2][1] |
| Routes of use | By mouth[3] |
| Typical dose | 5 to 40 mg per day[2] |
| External links | |
| AHFS/Drugs.com | International Drug Names |
| Legal | |
| Legal status |
|
| Pharmacokinetics | |
| Protein binding | 85% |
| Elimination half-life | 5.3h |
| Excretion | >90%Kidney |
| Chemical and physical data | |
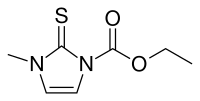
| Formula | C7H10N2O2S |
| Molar mass | 186.23 g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 122 to 125 °C (252 to 257 °F) |
SMILES
| |
InChI
| |
Carbimazole (CMZ) is a medication used to treat overactive thyroid, including Grave's disease.[2] In the United Kingdom, it is the first choice antithyroid medicine.[2] It can take a month or two before full effects.[2] It is taken by mouth.[2]
Side effects may include fever, rash, and joint pain.[1] Rare side effects may include bone marrow problems resulting in low white blood cells.[2] Other side effects may include pancreatitis.[2] Use during pregnancy may harm the baby; though, it has been used in pregnancy due to there also being harms of high thyroid.[2][1]
It is a type of thioamide, along with propylthiouracil (PTU).[4][1] After absorption it is converted to the active form, methimazole.[1] Methimazole prevents the thyroid peroxidase enzyme from adding iodine and coupling the tyrosine residues on thyroglobulin, hence reducing the production of T3 and T4.[4]
Carbimazole came into medical use in 1952.[5] It is on the World Health Organization's List of Essential Medicines as an alternative to methimazole.[6] It is available as a generic medication.[2] In the United Kingdom three month at a dose of 20 mg per day costs the NHS about £6 as of 2023.[2]
Medical uses
Medical therapy for hyperthyroidism typically involves either titrating the dose of carbimazole until the person becomes euthyroid or maintaining a high dose of carbimazole to suppress endogenous thyroid production, and then replacing thyroid hormone with levothyroxine ("block and replace").[7] Treatment is usually given for 1-2 years followed by a trial withdraw.[7]
The onset of anti-thyroid effect is rapid but the onset of clinical effects on thyroid hormone levels in the blood is much slower. This is because the large store of pre-formed T3 and T4 in the thyroid gland and bound to thyroid binding globulin (99% bound) has to be depleted before any beneficial clinical effect occurs.
Dosage
The starting dose is often 15 to 40 mg per day, which is decreased to 5 to 15 mg per day once thyroid levels have improved.[2] Doses of 40 to 60 mg per day together with levothyroxine may also be used.[2]
Side effects
Whilst rashes and pruritus are common, these can often be treated with antihistamines without stopping the carbimazole. For those patients where sensitivity reactions cannot be controlled, propylthiouracil may be used as an alternative; cross-sensitivity between these drugs is rare.
Its most serious rare side effect is bone marrow suppression causing neutropenia and agranulocytosis. This may occur at any stage during treatment and without warning; monitoring of white cell count is not useful. Patients are advised to immediately report symptoms of infection, such as sore throat or fever, so that a full blood count test may be arranged. If this confirms a low neutrophil count, discontinuation of the drug leads to recovery. However failure to report suggestive symptoms or delays in considering the possibility of immunosuppression and its testing, can lead to fatalities.
Precautions
Some people are allergic to azole(s). Some azole drugs have adverse side-effects. Some azole drugs may disrupt estrogen production in pregnancy, affecting pregnancy outcome.[8]
Carbimazole should be used judiciously in pregnancy as it crosses the placenta. It has (rarely) been associated with congenital defects, including aplasia cutis of the neonate but is not contra-indicated. However, it more predictably may cause fetal hypothyroidism so (in minimal doses) it can be used in order to control maternal hyperthyroidism. There are reported cases of goiter and choanal atresia in fetus.[9] Furthermore, breast feeding is possible but only if lowest effective dose is used and neonatal development is closely monitored.
For the above reasons, it is preferable to use PTU in pregnancy, especially in the first trimester, with the possibility of changing to Carbimazole for the second and third trimesters.[10]
Society and culture
Brand names
- Neo-mercazole[11]
- Vidalta
- Thyrocab
- Neomerdin
References
- 1 2 3 4 5 6 Francis, Thanuya; Francis, Niroshan; Lazarus, John H.; Okosieme, Onyebuchi E. (3 May 2020). "Safety of antithyroid drugs in pregnancy: update and therapy implications". Expert Opinion on Drug Safety. 19 (5): 565–576. doi:10.1080/14740338.2020.1748007. ISSN 1474-0338.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 BNF 83 (British National Formulary) March 2022 (83 ed.). Pharmaceutical Press. 13 Aug 2022. p. 829. ISBN 9780857114341.
- ↑ Ritter, James M.; Flower, Rod; Henderson, Graeme; Loke, Yoon Kong; Rang, Humphrey P. (2020). "35. Drugs affecting major organ systems". Rang & Dale's Pharmacology. Elsevier. pp. 452–453. ISBN 978-0-7020-7448-6. Archived from the original on 2021-08-28. Retrieved 2021-10-08.
- 1 2 Dong, Betty J. (2020). "38. Thyroid and antithyroid drugs". In Katzung, Bertram G.; Trevor, Anthony J. (eds.). Basic and Clinical Pharmacology 15e. New York: McGraw-Hill. pp. 718–719. ISBN 978-1-260-45231-0. Archived from the original on 2021-10-10. Retrieved 2021-10-10.
- ↑ Rifai, Nader (3 February 2022). Tietz Textbook of Laboratory Medicine - E-Book: Tietz Textbook of Laboratory Medicine - E-Book. Elsevier Health Sciences. p. 807. ISBN 978-0-323-83467-4. Archived from the original on 10 September 2023. Retrieved 9 September 2023.
- ↑ World Health Organization (2023). The selection and use of essential medicines 2023: web annex A: World Health Organization model list of essential medicines: 23rd list (2023). Geneva: World Health Organization. hdl:10665/371090. WHO/MHP/HPS/EML/2023.02.
- 1 2 Wiffen, Philip; Stoner, Nicola (2017). "20. Therapy-related issues: endocrine". Oxford Handbook of Clinical Pharmacy. Oxford: Oxford University Press. pp. 499–500. ISBN 978-0-19-873582-3. LCCN 2016945512. Archived from the original on 2021-10-09. Retrieved 2021-10-08.
- ↑ Kragie L, Turner SD, Patten CJ, Crespi CL, Stresser DM (August 2002). "Assessing pregnancy risks of azole antifungals using a high throughput aromatase inhibition assay". Endocrine Research. 28 (3): 129–40. doi:10.1081/ERC-120015045. PMID 12489563. S2CID 8282678.
- ↑ Brunton L, Chabner BA, Knollman B (2011). Goodman & Gilman's pharmacological basis of therapeutics (12th ed.). McGraw-Hill. ISBN 978-0-07-162442-8.
- ↑ Bahn RS, Burch HS, Cooper DS, Garber JR, Greenlee CM, Klein IL, Laurberg P, McDougall IR, Rivkees SA, Ross D, Sosa JA, Stan MN (July 2009). "The Role of Propylthiouracil in the Management of Graves' Disease in Adults: report of a meeting jointly sponsored by the American Thyroid Association and the Food and Drug Administration". Thyroid. 19 (7): 673–4. doi:10.1089/thy.2009.0169. PMID 19583480.
- ↑ "Neo-Mercazole Carbimazole". Nicholas Laboratories Indonesia. Archived from the original on 2016-03-04. Retrieved 2021-06-22.
External links
| Identifiers: |
|---|