Chronic bacterial prostatitis
| Chronic bacterial prostatitis | |
|---|---|
 | |
| Specialty | Urology |
| Symptoms | Pain with urination, trouble with the stream, frequent urination[1] |
| Complications | Sexual dysfunction[1] |
| Duration | >3 months[1] |
| Causes | Often Escherichia coli[1] |
| Risk factors | Urinary catheterization, diabetes, prostate biopsy, uncircumcised, transurethral resection of the prostate (TURP)[1][2] |
| Diagnostic method | Based on symptoms, examination, and urine testing[1] |
| Differential diagnosis | Benign prostatic hyperplasia (BPH), chronic pelvic pain syndrome (CPPS), interstitial cystitis, prostate cancer, pelvic floor dysfunction, prostatic abscess, bladder cancer[1][2] |
| Treatment | Antibiotics, alpha blockers[1] |
| Frequency | <1% of males at some point[2] |
Chronic bacterial prostatitis (CBP) is a bacterial infection of the prostate gland that results in symptoms for greater than 3 months.[1] Typical symptoms include pain with urination, trouble with the stream, and frequent urination.[1] Other symptoms may include pain in the lower abdomen or perineum, sexual dysfunction, or fever.[1] Symptoms are generally milder than acute bacterial prostatitis.[3]
Chronic bacterial prostatitis develops in about 10% of people after acute bacterial prostatitis.[1] Risk factors include urinary catheterization, diabetes, prostate biopsy, being uncircumcised, and transurethral resection of the prostate (TURP).[1][2] Most cases are due to the bacteria Escherichia coli.[1] Diagnosis is based on symptoms, examination, and urine testing.[1] Positive cultures are required for the diagnosis.[4] Other forms of prostatitis include acute bacterial prostatitis and chronic pelvic pain syndrome (CPPS).[5]
Treatment is generally with antibiotics by mouth for 4 to 12 weeks.[1] The antibiotics used should be based on the urine culture results with commonly used agents including levofloxacin] or azithromycin.[3][2] Alpha blockers, such as tamsulosin, and pain medications may also be used.[2] Re-occurrence of disease is common.[1] Chronic bacterial prostatitis occurs in less than 1% of males at some point in time.[2] It most commonly occurs in those under the age of 50.[1]
Signs and symptoms
Chronic bacterial prostatitis is a relatively rare condition that usually presents with an intermittent UTI-type picture. It is defined as recurrent urinary tract infections in men originating from a chronic infection in the prostate. Symptoms may be completely absent until there is also bladder infection, and the most troublesome problem is usually recurrent cystitis.[6] It is said that recurrent and relapsing UTIs (i.e., UTIs due to the same pathogen) are a hallmark of chronic bacterial prostatitis.[7][8][9]
Chronic bacterial prostatitis is the cause of less than 5% of prostate-related non-BPH lower urinary tract symptoms (LUTS).
Diagnosis
In chronic bacterial prostatitis, there are bacteria in the prostate, but there may be no symptoms or milder symptoms than occur with acute prostatitis.[10] The prostate infection is diagnosed by culturing urine as well as prostate fluid (expressed prostatic secretions or EPS) which are obtained by the doctor performing a rectal exam and putting pressure on the prostate. If no fluid is recovered after this prostatic massage, a post massage urine should also contain any prostatic bacteria.
Prostate specific antigen levels may be elevated, although there is no malignancy. Semen analysis is a useful diagnostic tool.[11] Semen cultures are also performed. Antibiotic sensitivity testing is also done to select the appropriate antibiotic. Other useful markers of infection are seminal elastase and seminal cytokines.
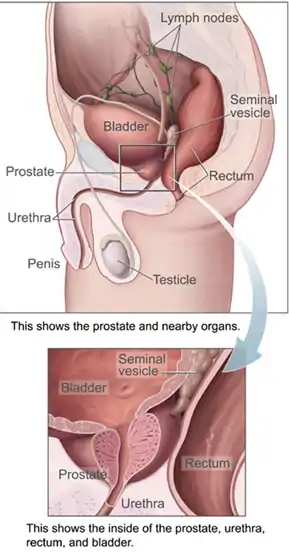
 Prostate, urethra, and seminal vesicles.
Prostate, urethra, and seminal vesicles. The arteries of the pelvis.
The arteries of the pelvis. Male pelvic organs seen from right side.
Male pelvic organs seen from right side.
Treatment
Antibiotic therapy has to overcome the blood/prostate barrier that prevents many antibiotics from reaching levels that are higher than minimum inhibitory concentration.[12] A blood-prostate barrier restricts cell and molecular movement across the prostate epithelium.[13] Treatment requires prolonged courses (4–8 weeks) of antibiotics that penetrate the prostate well.[14] The fluoroquinolones, tetracyclines and macrolides have the best penetration. There have been contradictory findings regarding the penetrability of nitrofurantoin, quinolones (ciprofloxacin, levofloxacin), sulfas (trimethoprim-sulfamethoxazole), doxycycline and macrolides (erythromycin, clarithromycin). This is particularly true for gram-positive infections. Other antibiotics with the potential for improved activity, including linezolid, moxifloxacin, tigecycline, daptomycin, clindamycin, and vancomycin, have been used limitedly off-label with reported success.[15]
In a review, levofloxacin was found to reach prostatic fluid concentrations 5.5 times higher than ciprofloxacin, indicating a greater ability to penetrate the prostate.[16] Moxifloxacin shows even greater prostatic penetration than levofloxacin and may be the only fluoroquinolone able to obtain prostatic concentrations 10-fold above the minimum inhibitory concentration against Enterococcus faecalis.[17] However, limited experience with moxifloxacin for chronic prostatitis exists.[17][15]
Success rates with antibiotics by mouth can reach 70% to 90% at 6 months, although trials comparing them with placebo or no treatment do not exist.[18]
Persistent infections may be helped in 80% by the use of alpha blockers (tamsulosin, alfuzosin), or long term low dose antibiotic therapy.[19] Recurrent infections may be caused by inefficient urination (benign prostatic hypertrophy, neurogenic bladder), prostatic stones or a structural abnormality that acts as a reservoir for infection.
In theory, the ability of some strains of bacteria to form biofilms might be one of the factors that facilitate development of chronic bacterial prostatitis.[20]
There is tentative evidence to support pelvic floor physiotherapy.[2]
Prostatectomy has been used to treat chronic bacterial prostatitis but inadequate data —including no randomized controlled trials— exists to allow clinical decisions.[21] Moreover, prostatectomy can result in erectile dysfunction and urinary incontinence as complications.[21]
Prognosis
Over time, the relapse rate is high, exceeding 50%. However, combination therapies offer a better prognosis than antibiotics alone.
A 2014 found that recurrence occurred within 2 months in 28% of the group using antibiotics alone (prulifloxacin 600 mg), but in only 8% of the group taking prulifloxacin in combination with Serenoa repens extract, Lactobacillus Sporogens and Arbutin.[22]
Large prostatic stones was shown to be related with the presence of bacteria,[23] a higher urinary symptoms and pain score, a higher IL-1β and IL-8 concentration in seminal plasma, a greater prostatic inflammation and a lower response to antibiotic treatment.[24]
Epidemiology
Chronic bacterial prostatitis is rare.[25]
Research
Bacteriophages hold promise as another potential treatment for chronic bacterial prostatatis.[26]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 Su, ZT; Zenilman, JM; Sfanos, KS; Herati, AS (3 June 2020). "Management of Chronic Bacterial Prostatitis". Current urology reports. 21 (7): 29. doi:10.1007/s11934-020-00978-z. PMID 32488742.
- 1 2 3 4 5 6 7 8 Holt, JD; Garrett, WA; McCurry, TK; Teichman, JM (15 February 2016). "Common Questions About Chronic Prostatitis". American family physician. 93 (4): 290–6. PMID 26926816.
- 1 2 Davis, NG; Silberman, M (January 2023). "Bacterial Acute Prostatitis". PMID 29083799.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Bowen, DK; Dielubanza, E; Schaeffer, AJ (27 August 2015). "Chronic bacterial prostatitis and chronic pelvic pain syndrome". BMJ clinical evidence. 2015. PMID 26313612.
- ↑ Holt JD, Garrett WA, McCurry TK, Teichman JM (February 2016). "Common Questions About Chronic Prostatitis". American Family Physician. 93 (4): 290–6. PMID 26926816.
- ↑ Habermacher GM, Chason JT, Schaeffer AJ (2006). "Prostatitis/chronic pelvic pain syndrome". Annual Review of Medicine. 57 (1): 195–206. doi:10.1146/annurev.med.57.011205.135654. PMID 16409145.
- ↑ Najar MS, Saldanha CL, Banday KA (October 2009). "Approach to urinary tract infections". Indian J Nephrol. 19 (4): 129–39. doi:10.4103/0971-4065.59333. PMC 2875701. PMID 20535247.
- ↑ Lipsky BA, Byren I, Hoey CT (June 2010). "Treatment of bacterial prostatitis". Clin Infect Dis. 50 (12): 1641–52. doi:10.1086/652861. PMID 20459324.
- ↑ Wright ET, Chmiel JS, Grayhack JT, Schaeffer AJ (December 1994). "Prostatic fluid inflammation in prostatitis". J Urol. 152 (6 Pt 2): 2300–3. doi:10.1016/s0022-5347(17)31662-2. PMID 7966728.
- ↑ "Prostatitis - Symptoms". NHS Choices. 2017-10-19. Archived from the original on 2017-10-17. Retrieved 2022-08-19.
- ↑ Magri V, Wagenlehner FM, Montanari E, Marras E, Orlandi V, Restelli A, et al. (July 2009). "Semen analysis in chronic bacterial prostatitis: diagnostic and therapeutic implications". Asian Journal of Andrology. 11 (4): 461–77. doi:10.1038/aja.2009.5. PMC 3735310. PMID 19377490.
- ↑ Fulmer BR, Turner TT (May 2000). "A blood-prostate barrier restricts cell and molecular movement across the rat ventral prostate epithelium". The Journal of Urology. 163 (5): 1591–4. doi:10.1016/S0022-5347(05)67685-9. PMID 10751894. Archived from the original on 2019-12-10. Retrieved 2022-08-19.
- ↑ Barza M (January 1993). "Anatomical barriers for antimicrobial agents". European Journal of Clinical Microbiology & Infectious Diseases. 12 Suppl 1 (Suppl 1): S31-5. doi:10.1007/BF02389875. PMID 8477760. S2CID 23753756.
- ↑ Charalabopoulos K, Karachalios G, Baltogiannis D, Charalabopoulos A, Giannakopoulos X, Sofikitis N (December 2003). "Penetration of antimicrobial agents into the prostate" (PDF). Chemotherapy. 49 (6): 269–79. doi:10.1159/000074526. PMID 14671426. S2CID 14731590. Archived (PDF) from the original on 2021-05-06. Retrieved 2022-08-19.
- 1 2 Perletti G, Trinchieri A, Stamatiou K, Magri V (February 2022). "Safety considerations with new antibacterial approaches for chronic bacterial prostatitis". Expert Opin Drug Saf. 21 (2): 171–182. doi:10.1080/14740338.2021.1956459. PMID 34260337.
- ↑ "Levofloxacin and Its Effective Use in the Review Management of Bacterial Prostatitis" (PDF). Archived from the original (PDF) on 2017-08-09. Retrieved 2016-02-08.
- 1 2 Xiong S, Liu X, Deng W, Zhou Z, Li Y, Tu Y, Chen L, Wang G, Fu B (2020). "Pharmacological Interventions for Bacterial Prostatitis". Front Pharmacol. 11: 504. doi:10.3389/fphar.2020.00504. PMC 7203426. PMID 32425775.
- ↑ Bowen DK, Dielubanza E, Schaeffer AJ (August 2015). "Chronic bacterial prostatitis and chronic pelvic pain syndrome". BMJ Clinical Evidence. 2015: 1802–1831. PMC 4551133. PMID 26313612.
- ↑ Shoskes DA, Hakim L, Ghoniem G, Jackson CL (April 2003). "Long-term results of multimodal therapy for chronic prostatitis/chronic pelvic pain syndrome". The Journal of Urology. 169 (4): 1406–10. doi:10.1097/01.ju.0000055549.95490.3c. PMID 12629373.
- ↑ Wagenlehner FM, Pilatz A, Bschleipfer T, Diemer T, Linn T, Meinhardt A, et al. (August 2013). "Bacterial prostatitis". World Journal of Urology. 31 (4): 711–6. doi:10.1007/s00345-013-1055-x. PMID 23519458. S2CID 1925596.
- 1 2 Schoeb DS, Schlager D, Boeker M, Wetterauer U, Schoenthaler M, Herrmann TR, Miernik A (November 2017). "Surgical therapy of prostatitis: a systematic review". World J Urol. 35 (11): 1659–1668. doi:10.1007/s00345-017-2054-0. PMID 28612108.
- ↑ Busetto GM, Giovannone R, Ferro M, Tricarico S, Del Giudice F, Matei DV, et al. (July 2014). "Chronic bacterial prostatitis: efficacy of short-lasting antibiotic therapy with prulifloxacin (Unidrox®) in association with saw palmetto extract, lactobacillus sporogens and arbutin (Lactorepens®)". BMC Urology. 14 (1): 53. doi:10.1186/1471-2490-14-53. PMC 4108969. PMID 25038794.
- ↑ Mazzoli, Sandra (August 2010). "Biofilms in chronic bacterial prostatitis (NIH-II) and in prostatic calcifications". FEMS Immunology and Medical Microbiology. 59 (3): 337–344. doi:10.1111/j.1574-695X.2010.00659.x. ISSN 1574-695X. PMID 20298500.
- ↑ Soric, Tomislav; Selimovic, Mirnes; Bakovic, Lada; Šimurina, Tatjana; Selthofer, Robert; Dumic, Jerka (2017). "Clinical and Biochemical Influence of Prostatic Stones". Urologia Internationalis. 98 (4): 449–455. doi:10.1159/000455161. ISSN 1423-0399. PMID 28052296. S2CID 4927272.
- ↑ Schneider H, Ludwig M, Hossain HM, Diemer T, Weidner W (October 2003). "The 2001 Giessen Cohort Study on patients with prostatitis syndrome--an evaluation of inflammatory status and search for microorganisms 10 years after a first analysis". Andrologia. 35 (5): 258–62. doi:10.1046/j.1439-0272.2003.00586.x. PMID 14535851. S2CID 21022117.
- ↑ Letkiewicz S, Międzybrodzki R, Kłak M, Jończyk E, Weber-Dąbrowska B, Górski A (November 2010). "The perspectives of the application of phage therapy in chronic bacterial prostatitis". FEMS Immunology and Medical Microbiology. 60 (2): 99–112. doi:10.1111/j.1574-695X.2010.00723.x. PMID 20698884.
External links
| Classification | |
|---|---|
| External resources |
- Prostatitis at Curlie