Epidural blood patch
| Epidural blood patch | |
|---|---|
 Diagram of an epidural blood patch | |
| ICD-10-PCS | G97.1 |
| MeSH | D017217 |
An epidural blood patch (EBP) is a surgical procedure that uses autologous blood in order to close one or many holes in the dura mater of the spinal cord, usually as a result of a previous lumbar puncture or epidural. The procedure can be used to relieve orthostatic headaches, most commonly post dural puncture headache (PDPH). The procedure carries the typical risks of any epidural procedure. They are usually administered near the site of the cerebrospinal fluid leak (CSF leak), but in some cases the upper part of the spine is targeted. An epidural needle is inserted into the epidural space like a traditional epidural procedure. The blood modulates the pressure of the CSF and forms a clot, sealing the leak. EBPs were first described by American anesthesiologist Turan Ozdil and surgeon James B Gormley around 1960.
EBPs are an invasive procedure but are safe and effective—further intervention is sometimes necessary, and repeat patches can be administered until symptoms resolve. It is the standard treatment for PDPH. Common side effects include back pain and headache. Rebound intracranial hypertension in people with spontaneous intracranial hypotension (SIH) is common, and people with SIH may have less success with EBPs. While the procedure uses blood, it does not carry a significant infectious risk, even in immunocompromised people. The procedure is not entirely benign—seven cases of arachnoiditis have been reported as a result of administration.
Uses
EBPs are administered for treatment-related or spontaneous orthostatic headaches.[1] The procedure is most often used to relieve PDPH following an epidural injection and lumbar puncture. Most PDPHs are self-limiting, so epidural blood patches are only used for people with moderate to severe cases who do not respond to conservative treatment.[2][3] It is also used to treat spontaneous intracranial hypotension (SIH).[4][3] EBP has been used to treat pseudomeningoceles and leaks around intrathecal pumps.[5] For SIH, the same administration technique is used but at a different location with a different amount of blood injected.[6]
Technique
Anatomy
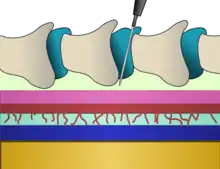
An epidural is injected into the epidural space, inside the bony spinal canal but just outside the dura. In contact with the inner surface of the dura is another membrane called the arachnoid mater, which contains the cerebrospinal fluid. In adults, the spinal cord terminates around the level of the disc between L1 and L2, while in neonates it extends to L3 but can reach as low as L4.[7] Below the spinal cord there is a bundle of nerves known as the cauda equina or "horse's tail". Hence, lumbar epidural injections carry a low risk of injuring the spinal cord. Insertion of an epidural needle involves threading a needle between the bones, through the ligaments and into the epidural space without puncturing the layer immediately below containing CSF under pressure.[7] For administration of an EBP due to PDPH, the level of prior epidural puncture is targeted;[6] blood injected for the most part spreads cranially.[8] For SIH with unidentified leakage spots, L2 and L3 are targeted initially.[6]
Insertion
For EBPs, autologous blood is drawn from a peripheral vein;[2][9] the procedure uses a typical epidural needle.[2] 20 mL of blood is recommended for EBPs, though injection should stop if not tolerated by the patient.[3] This amount of blood is also recommended for people in obstetrics.[10] Targeted EBP is performed under real-time fluoroscopy if the location of the CSF leak is known.[3] This fluoroscopic approach is standard,[6] but with cases of SIH two-site blind injection has similar outcomes. No randomized clinical trials have been conducted for this due to the rarity of SIH.[11] CT scanning can also be used.[3] Blood from EBPs is spread throughout several segments within the epidural space, so it does not need to be injected at the same level as the puncture.[9] For treatment of SIH, medication with acetazolamide before an EBP and administration in the Trendelenburg position is effective.[12]
Mechanism
When an EBP is administered a mass effect occurs which compresses the subarachnoid space, thereby increasing and modulating the pressure of the CSF, which translates intracranially. Blood maintains a pressures surge for a longer time than crystalloid fluids. Simultaneously, an "epidural plug" is formed as a result of clot formation; the clot adheres to the thecal sac, potentially becoming a permanent plug.[3][6][13] After about half a day the mass effect stops, and a mature clot is left.[13]
Contraindications
EBPs are contraindicated in people with bleeding disorders, infection at the puncture site, fever, and bloodstream infections or sepsis.[3] Some recommend blood culture before administration.[13] EBPs should not be administered if there is a systemic infection. It may be contraindicated in people with a spinal deformity, HIV/AIDS, and leukemia. Epidurals are recommended for perioperative COVID-19 people over general anesthesia—EBPs have an extremely low risk of transferring an infection to the central nervous system even with an ongoing infection but are a last resort after conservative treatments and nerve blocks.[3] People who have malignancies as a result of cancer may be contraindicated though it is not an absolute contraindication; though little large-scale clinical studies have been conducted, no adverse effects have been reported.[9]
Effectiveness and complications
EBPs are invasive[13] but are highly effective with a 50-80% success rate, and are relatively low risk, except the risks associated with epidural administration.[2][8] Waiting 24 hours before administration reduces the failure rate of it significantly,[13] though performing it within 48 hours after puncture is associated with a higher need for repeat patches.[8] Successful treatment of PDPH with EBP has been reported months after onset.[5] Success rates may be higher than 96% with repeated EBP, even in the pediatric population.[9] EBPs are more likely to be successful with more than 22.5 mL of blood injected, and in people with less severe spinal CSF leakage. In people with severe leakage, treatment outcome does not depend on the amount of blood injected.[14] An ineffective EBP is more likely to occur in people with SIH where the CSF leak was not identified—they may be repeated for these people. Nerve compression can also occur which can result in transient neurologic damage; less frequently, this may be permanent.[6] Some people may benefit from fibrin glue mixed with the blood.[15] EBP may cause more side effects than a topical nerve block of the sphenopalatine neuron cell group in postpartum people though no large-scale clinical trials have been conducted.[16] Multiple EBPs can be administered as necessary; this is more likely to happen with people with spontaneous headache or multiple leakages.[1] About 20% of people need a second EBP, and up to 20% of women do not have their symptoms resolved.[8]
Additional dural puncture can occur, however, which may increase the chance of inadvertently injecting blood intrathecally.[3] Prophylactic EBPs do not decrease the risk of getting PDPH.[2] The use of EBPs as a treatment for PDPH, although historically considered aggressive, is increasing in adolescents as they are less likely to have their headaches resolved by conservative treatment.[9] Fluoroscopic EBPs are more successful than blindly administered ones. The failure rate is around 15-20%,[3] though this can get as high as 30%.[13] Common side effects are headache, back pain, neck pain, and mild fever. Back pain is reported in approximately 80% of people, which might be a result of increased pressure. Radicular pain may also occur.[3] Rebound intracranial hypotension is very common in people with SIH after an EBP, and can be treated with acetazolamide, topiramate, or in severe cases therapeutic lumbar puncture; most cases are not severe. Rare side effects include subdural or spinal bleeding, infection, and seizure,[3] though EBPs do not carry a significant infectious risk even in immunocompromised people.[5] Neurological symptoms occasionally develop as a result of administration.[8] Seven cases of arachnoiditis have been documented.[17]
History
The treatment of PDPH was historically uncertain—49 recommendations existed for the treatment of it. It was originally thought to be more of a psychogenic disease, which may have delayed the development of EBPs. Turan Ozdil, an anesthesiology instructor at the University of Tennessee, hypothesized how clotted blood could plug a hole in the dura while observing a car tire repair.[5] He worked with his associate W. Forrest Powell, leading to trials on dog models and then on humans around 1960.[5] James B. Gormley, a general surgeon, first observed how bloody lumbar punctures led to reduced rates of PDPH also in 1960;[3] Gormley would use only 2 to 3 mL of blood for experimenting with EBP, and he was not trained in epidural administration. Ozdil was unaware of Gormley's work, and Ozdil designed his technique to be prophylactic. Anesthesiologist Anthony DiGiovanni refined Ozdil and Powell's technique, using 10 mL of blood to treat a person with unknown leakage locations. DiGiovanni's staff member Burdett Dunbar wanted to more widely disseminate their technique, though their study was initially rejected by Anesthesiology until publication in Anesthesia & Analgesia in 1970. Detractors such as Charles Bagley at Johns Hopkins University provided evidence against the treatment since 1928 as according to their studies blood in the CSF had significant side effects up to "severe convulsive seizures"; DiGiovanni disproved this in 1972.[5] J. Selwyn Crawford discovered in 1980 that using a larger volume of blood was more successful.[3] The procedure would be widely accepted at the end of the 1970s.[5]
References
- 1 2 So, Yun; Park, Jung Min; Lee, Pil-Moo; Kim, Cho Long; Lee, Cheolhan; Kim, Jae Hun (2016). "Epidural Blood Patch for the Treatment of Spontaneous and Iatrogenic Orthostatic Headache". Pain Physician. 19 (8): E1115–E1122. ISSN 2150-1149. PMID 27906941.
- 1 2 3 4 5 Tubben, Robert E.; Jain, Sameer; Murphy, Patrick B. (2022), "Epidural Blood Patch", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 29493961, retrieved 2022-01-20
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Shin, Hwa Yong (2022-01-18). "Recent update on epidural blood patch". Anesthesia and Pain Medicine. 17: 12–23. doi:10.17085/apm.21113. ISSN 1975-5171. PMID 35038855. S2CID 246075960.
- ↑ D'Antona, Linda; Jaime Merchan, Melida Andrea; Vassiliou, Anna; Watkins, Laurence Dale; Davagnanam, Indran; Toma, Ahmed Kassem; Matharu, Manjit Singh (2021-03-01). "Clinical Presentation, Investigation Findings, and Treatment Outcomes of Spontaneous Intracranial Hypotension Syndrome: A Systematic Review and Meta-analysis". JAMA Neurology. 78 (3): 329–337. doi:10.1001/jamaneurol.2020.4799. ISSN 2168-6157. PMC 7783594. PMID 33393980.
- 1 2 3 4 5 6 7 Harrington, B (2004). "Postdural Puncture Headache and the Development of the Epidural Blood Patch". Regional Anesthesia and Pain Medicine. 29 (2): 136–163. doi:10.1016/j.rapm.2003.12.023. PMID 15029551. S2CID 31393357.
- 1 2 3 4 5 6 White, Benjamin; Lopez, Victor; Chason, David; Scott, David; Stehel, Edward; Moore, William. The lumbar epidural blood patch: A Primer. Appl Radiol. 2019. 48(2):25-30.
- 1 2 Schneider B, Zheng P, Mattie R, Kennedy DJ (2 August 2016). "Safety of epidural steroid injections". Expert Opinion on Drug Safety. 15 (8): 1031–1039. doi:10.1080/14740338.2016.1184246. PMID 27148630. S2CID 27053083.
- 1 2 3 4 5 "Statement on Post-Dural Puncture Headache Management". American Society of Anesthesiologists. 2021-10-13. Retrieved 2022-01-23.
- 1 2 3 4 5 Morgan, Kyle J.; Mohan, Rahul; Karol, Seth E.; Flerlage, Jamie (2021-06-01). "Epidural blood patch for post-dural puncture headaches in adult and paediatric patients with malignancies: a review". British Journal of Anaesthesia. 126 (6): 1200–1207. doi:10.1016/j.bja.2020.11.041. ISSN 1471-6771. PMID 33612247. S2CID 231990272.
- ↑ Paech, Michael J.; Doherty, Dorota A.; Christmas, Tracey; Wong, Cynthia A. (2011). "The Volume of Blood for Epidural Blood Patch in Obstetrics: A Randomized, Blinded Clinical Trial". Anesthesia & Analgesia. 113 (1): 126–133. doi:10.1213/ANE.0b013e318218204d. ISSN 0003-2999. PMID 21596867. S2CID 24648644.
- ↑ Ahn, Curie; Lee, Eugene; Lee, Joon Woo; Chee, Choong Guen; Kang, Yusuhn; Kang, Heung Sik (2019-04-01). "Two-site blind epidural blood patch versus targeted epidural blood patch in spontaneous intracranial hypotension". Journal of Clinical Neuroscience. 62: 147–154. doi:10.1016/j.jocn.2018.11.039. PMID 30497854. S2CID 53720896.
- ↑ Ferrante, E.; Arpino, I.; Citterio, A.; Wetzl, R.; Savino, A. (2010-05-12). "Epidural blood patch in Trendelenburg position pre-medicated with acetazolamide to treat spontaneous intracranial hypotension: Epidural blood patch to treat spontaneous intracranial hypotension". European Journal of Neurology. 17 (5): 715–719. doi:10.1111/j.1468-1331.2009.02913.x. PMID 20050898. S2CID 41161097.
- 1 2 3 4 5 6 Nath, Gita; Subrahmanyam, Maddirala (2011). "Headache in the parturient: Pathophysiology and management of post-dural puncture headache". Journal of Obstetric Anaesthesia and Critical Care. 1 (2): 57. doi:10.4103/2249-4472.93988. ISSN 2249-4472.
- ↑ Wu, Jr-Wei; Hseu, Shu-Shya; Fuh, Jong-Ling; Lirng, Jiing-Feng; Wang, Yen-Feng; Chen, Wei-Ta; Chen, Shih-Pin; Wang, Shuu-Jiun (2017-01-02). "Factors predicting response to the first epidural blood patch in spontaneous intracranial hypotension". Brain. 140 (2): 344–352. doi:10.1093/brain/aww328. ISSN 0006-8950. PMID 28043956.
- ↑ Elwood, Justin J.; Dewan, Misha; Smith, Jolene M.; Mokri, Bahram; Mauck, William D.; Eldrige, Jason S. (2016-07-04). "Efficacy of epidural blood patch with fibrin glue additive in refractory headache due to intracranial hypotension: preliminary report". SpringerPlus. 5 (1): 317. doi:10.1186/s40064-016-1975-1. ISSN 2193-1801. PMC 4788675. PMID 27066348.
- ↑ Cohen, Shaul; Levin, Danielle; Mellender, Scott; Zhao, Rong; Patel, Preet; Grubb, William; Kiss, Geza (2018). "Topical Sphenopalatine Ganglion Block Compared With Epidural Blood Patch for Postdural Puncture Headache Management in Postpartum Patients: A Retrospective Review". Regional Anesthesia and Pain Medicine. 43 (8): 880–884. doi:10.1097/AAP.0000000000000840. ISSN 1532-8651. PMID 30063655. S2CID 51891715.
- ↑ Villani, Linda A.; Digre, Kathleen B.; Cortez, Melissa M.; Bokat, Christina; Rassner, Ulrich A.; Ozudogru, Seniha N. (2021-02-13). "Arachnoiditis, a complication of epidural blood patch for the treatment of low-pressure headache: A case report and systematic review". Headache. 61 (2): 244–252. doi:10.1111/head.14076. ISSN 1526-4610. PMID 33583044. S2CID 231926107.