Esophageal balloon tamponade
| Esophageal balloon tamponade | |
|---|---|
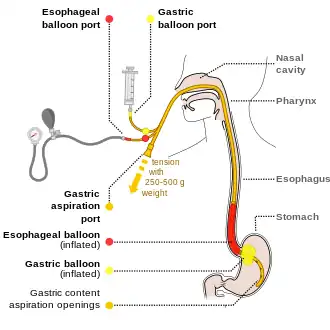 | |
| Drawing of using the Blakemore tube. There is a manometer connected to the esophageal port, to enable inflating the balloon with correct pressure. | |
| Contraindications | Recent esophageal surgery, esophageal stricture[1] |
| Types | Sengstaken-Blakemore, Minnesota, Linton[2] |
| Steps | 1) Intubate 2) Verify balloons intact 3) Place tube via the mouth 4) Verify placement by X-ray 5) Inflate stomach balloon 6) Apply traction 7) Inflate the esophageal balloon if needed[1] |
| Complications | Airway obstruction, esophageal rupture[1] |
Esophageal balloon tamponade refers to the use of balloon tamponade in the esophagus and stomach.[1] This is generally carried out to treat bleeding from esophageal or gastric varices when other measures are not available or not successful.[1]
The most common cause of bleeding from varices is cirrhosis.[1] These devices are generally only used in people who are hemodynamically unstable.[1] Contraindications for placement include recent esophageal surgery or esophageal stricture.[1]
Preparation involves intubation followed by placing the person on their back at 45 degrees.[1] The device is than checked to make sure no leaks are present.[1] It is than placed via the mouth and 50 ml of air are added to the stomach balloon.[1] An X-ray is than done to verify placement and once confirmed more air is added.[1] Traction can than be applied.[1] Bleeding is than checked for, and if present the esophageal balloon may be inflated using a manometer.[1]
After placement, further treatment is required.[1] Complications can include airway obstruction, esophageal rupture, and aspiration pneumonia.[1] The procedure is rarely done.[1] The first device developed was the Sengstaken-Blakemore tube in the 1950s.[1] Other versions of the device include the Minnesota tube and the Linton tube.[1][2]
Medical use
When inserted balloon catheters are intended to stop bleeding from vascular structures—including esophageal varices and gastric varices—in the upper gastrointestinal tract. Balloon tamponade is considered a bridge to more definitive treatment.
It is estimated to be about 90% effective.[3]
Contraindications
Contraindications include recent esophageal surgery and esophageal stricture.[1] A hiatus hernia may make use more complicated.[1][4]
Technique
While there is slight variation between the types of tubes the general technique is:
- Intubate to protect the airway
- Verify that all balloons inflate and are intact
- Place the tube all the way in either via the mouth or nose and put in a bit of air
- Verify that the end of the tube is in the stomach by X-ray
- Inflate the stomach balloon and apply traction. This may be done by attaching a liter bag of normal saline over an intravenous pole.
- Often this is sufficient. If the esophageal balloon is inflated a manometer is required to verify that excessive pressures are not used
The esophageal balloon can have 40 cmH2O (30 mmHg) place in it.[1] If this is not enough 60 cmH2O (45 mmHg) may be used.[1]
Traction can then be applied, with a number of techniques described to maintain this.[5]
Equipment
There are three types of balloons manufactured for the purpose of tamponading upper gastrointestinal bleeds, each with different volume capacities and aspiration ports.
They include:
- Sengstaken-Blakemore tube, with three lumens (two balloons and a gastric aspiration port). Pressure can be applied to gastric and esophageal varices by balloon inflation and traction.[6]
- Linton tube, with a large gastric balloon, and gastric and esophageal aspirates
- Minnesota four-lumen tube, with esophageal and gastric balloons, and esophageal and gastric aspirates.
 A Blakemore tube
A Blakemore tube Manometer used to inflate the esophageal balloon and verify that excessive pressures are not used
Manometer used to inflate the esophageal balloon and verify that excessive pressures are not used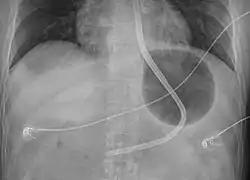 A Blakemore tube inflated in the stomach
A Blakemore tube inflated in the stomach
Society and culture
Instructions are available on how to make a training mannequin to practice placement.[7]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 Powell, M; Journey, JD (January 2021). "Sengstaken-Blakemore Tube". PMID 32644350.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 "Esophageal Balloon Tamponade". fpnotebook.com. Archived from the original on 22 January 2021. Retrieved 15 March 2021.
- ↑ "Sengstaken–Blakemore and Minnesota Tubes • LITFL • CCC Equipment". Life in the Fast Lane • LITFL. 30 January 2019. Archived from the original on 24 January 2021. Retrieved 15 March 2021.
- ↑ Morgenstern, Justin (23 May 2016). "Balloon tamponade of GI bleeding". First10EM. Archived from the original on 7 March 2021. Retrieved 15 March 2021.
- ↑ Murphy, Evelyn Patricia; O'Brien, Sean Michael; Regan, Mark (20 March 2017). "Alternative method of tractioning the Sengstaken-Blakemore tube". BMJ Case Reports: bcr2016218401. doi:10.1136/bcr-2016-218401.
- ↑ "Sengstaken-Blakemore Tube Placement: Background, Indications, Contraindications". 2018-07-05. Archived from the original on 2019-06-05. Retrieved 2018-11-07.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Young, TP; Kuntz, HM; Alice, B; Roper, J; Kiemeney, M (November 2017). "An Inexpensive Esophageal Balloon Tamponade Trainer" (PDF). The Journal of emergency medicine. 53 (5): 726–729. doi:10.1016/j.jemermed.2017.08.018. PMID 29128036. Archived (PDF) from the original on 2021-01-27. Retrieved 2021-03-15.
External links
- EMRAP Blakemore tube Archived 2021-08-29 at the Wayback Machine
- EMRAP Minnesota tube Archived 2021-08-28 at the Wayback Machine
- Life in the Fastlane Blakemore and Minnesota instructions Archived 2021-01-24 at the Wayback Machine
| Classification |
|---|