Metformin
 | |
 | |
| Names | |
|---|---|
| Pronunciation | /mɛtˈfɔːrmɪn/, met-FOR-min |
| Trade names | Fortamet, Glucophage, Glumetza, others |
| Other names | N,N-dimethylbiguanide[1] |
IUPAC name
| |
| Clinical data | |
| Drug class | Biguanide[2] |
| Main uses | Type 2 diabetes[3] |
| Side effects | Diarrhea, nausea, abdominal pain, low blood sugar[2] |
| Pregnancy category | |
| Routes of use | By mouth |
| Defined daily dose | 2 grams[5] |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a696005 |
| Legal | |
| License data | |
| Legal status | |
| Pharmacokinetics | |
| Bioavailability | 50–60%[6][7] |
| Protein binding | Minimal[6] |
| Metabolism | Not by liver[6] |
| Elimination half-life | 4–8.7 hours[6] |
| Excretion | Urine (90%)[6] |
| Chemical and physical data | |
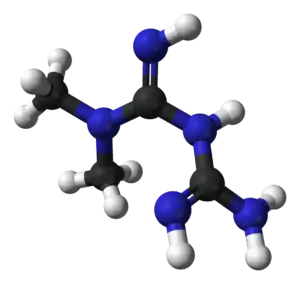
| Formula | C4H11N5 |
| Molar mass | 129.167 g·mol−1 |
| 3D model (JSmol) | |
| Density | 1.3±0.1[8] g/cm3 |
SMILES
| |
InChI
| |
Metformin, marketed under the trade name Glucophage among others, is the first-line medication for the treatment of type 2 diabetes,[2][9] particularly in people who are overweight.[10] It is also used in the treatment of polycystic ovary syndrome.[2] It is not associated with weight gain.[11] It is taken by mouth.[2]
Metformin is generally well tolerated.[12] Common side effects include diarrhea, nausea, and abdominal pain.[2] It has a low risk of causing low blood sugar.[2] High blood lactic acid level is a concern if the medication is used in overly large doses or prescribed in persons with severe kidney problems.[13][14] It is not recommended in those with significant liver disease.[2] While no clear harm comes from use during pregnancy, insulin is generally preferred for gestational diabetes.[2][15] Metformin is a biguanide antihyperglycemic agent.[2] It works by decreasing glucose production by the liver and increasing the insulin sensitivity of body tissues.[2]
Metformin was discovered in 1922.[16] French physician Jean Sterne began study in humans in the 1950s.[16] It was introduced as a medication in France in 1957 and the United States in 1995.[2][17] It is on the World Health Organization's List of Essential Medicines.[18] Metformin is the most widely used medication for diabetes taken by mouth.[16] It is available as a generic medication.[2] The wholesale price in the developed world was between US$0.20 and $6 per month as of 2014.[19] In the United States, it costs 5 to 25 USD per month.[2] In the UK, a standard 500 mg tablet costs around £0.03, with other forms being more expensive.[20] In 2017, it was the fourth-most commonly prescribed medication in the United States, with more than 78 million prescriptions.[21][22]
Medical uses
Metformin is used to lower the blood sugar in those with type 2 diabetes.[2] It is also used as a second line agent for infertility in those with polycystic ovary syndrome.[2][23]
Type 2 diabetes
The American Diabetes Association and the American College of Physicians each recommend metformin as a first-line agent to treat type 2 diabetes.[24][25][26] It is as effective as repaglinide and more effective than all other oral diabetes mellitus type 2 drugs.[27]
Efficacy
The UK Prospective Diabetes Study, a large clinical trial performed in 1980–90s, provided evidence that metformin reduced the rate of adverse cardiovascular outcomes in overweight patients with type 2 diabetes relative to other antihyperglycemic agents.[28] However, accumulated evidence from other and more recent trials reduced confidence in the efficacy of metformin for cardiovascular disease prevention.[29][30] Outcomes are improved even in those with some degree of kidney disease, heart failure, or chronic liver disease.[31]
Treatment guidelines for major professional associations including the European Association for the Study of Diabetes, the European Society for Cardiology, and the American Diabetes Association, now describe evidence for the cardiovascular benefits of metformin as equivocal.[25][32]
In 2017, the American College of Physicians's guidelines were updated to recognize metformin as the first-line treatment for type 2 diabetes. These guidelines supersede earlier reviews. For example, a 2014 review found tentative evidence that people treated with sulfonylureas had a higher risk of severe low blood sugar events (RR 5.64), though their risk of nonfatal cardiovascular events was lower than the risk of those treated with metformin (RR 0.67). Not enough data were available at that time to determine the relative risk of death or of death from heart disease.[33]
Metformin has little to no effect on body weight in type 2 diabetes compared with placebo,[34] in contrast to sulfonylureas which are associated with weight gain.[34] There is some evidence that metformin is associated with weight loss in obesity in the absence of diabetes.[35][36] Metformin has a lower risk of hypoglycemia than the sulfonylureas,[37][38] although hypoglycemia has uncommonly occurred during intense exercise, calorie deficit, or when used with other agents to lower blood glucose.[39][40] Metformin modestly reduces LDL and triglyceride levels.[37][38]
Polycystic ovarian syndrome
In those with polycystic ovarian syndrome (PCOS), tentative evidence shows that metformin use increases the rate of live births.[41] This includes in those who have not been able to get pregnant with clomiphene.[42] Metformin does not appear to change the risk of miscarriage.[41] A number of other benefits have also been found both during pregnancy and in nonpregnant people with PCOS.[43][44] In women with PCOS undergoing in vitro fertilization, evidence does not support a benefit with respect to live births.[45] The evidence does not support general use during pregnancy for improving maternal and infant outcomes in obese women.[46]
The United Kingdom's National Institute for Health and Clinical Excellence recommended in 2004 that women with PCOS and a body mass index above 25 be given metformin for anovulation and infertility when other therapies fail to produce results.[47] UK and international clinical practice guidelines do not recommend metformin as a first-line treatment[48] or do not recommend it at all, except for women with glucose intolerance.[49] The guidelines suggest clomiphene as the first medication option and emphasize lifestyle modification independently from medical treatment. Metformin treatment decreases the risk of developing type 2 diabetes mellitus in women with PCOS who exhibited impaired glucose tolerance (IGT) at baseline.[50][51]
Diabetes mellitus and pregnancy
A review of metformin use during pregnancy compared to insulin alone found good short-term safety for both the mother and baby, but unclear long-term safety.[52] Several observational studies and randomized, controlled trials found metformin to be as effective and safe as insulin for the management of gestational diabetes.[53][54] Nonetheless, several concerns have been raised and evidence on the long-term safety of metformin for both mother and child is lacking.[55] Compared with insulin, women with gestational diabetes treated with metformin gain less weight and are less likely to develop pre‐eclampsia during pregnancy.[55][56] Babies born to women treated with metformin have less visceral fat, and this may make them less prone to insulin resistance in later life.[57] The use of metformin for gestational diabetes resulted in smaller babies compared to treatment with insulin. However, despite initially lower birth weight, children exposed to metformin during pregnancy had accelerated growth after birth, and were heavier by mid-childhood than those exposed to insulin during pregnancy. This pattern of initial low birth weight followed by catch-up growth that surpasses comparative children has been associated with long-term cardio-metabolic disease.[58]
Weight change
Metformin is typically associated with weight loss.[59] Metformin appears to be safe and effective in counteracting the weight gain caused by the antipsychotic medications olanzapine and clozapine.[60][61] Although modest reversal of clozapine-associated weight gain is found with metformin, primary prevention of weight gain is more valuable.[62]
Use with insulin
Metformin may reduce the insulin requirement in type 1 diabetes, albeit with an increased risk of hypoglycemia.[63]

Skin
In terms of skin conditions metformin may also be effective in the case of:[64]
Dosage
The defined daily dose is 2 grams by mouth.[5] The typical initial dose is 500 mg once per day for the first week increased to 500 mg twice per day the second week.[3] Doses up to 2 grams per day may be used.[3] In those with moderate kidney problems a maximum dose of 1 gram is recommended.[3]
Contraindications
Metformin is contraindicated in people with:
- severe renal impairment (estimated glomerular filtration rate (eGFR) below 30 ml/min/1.73 m2)
- known hypersensitivity to metformin
- acute or chronic metabolic acidosis, including diabetic ketoacidosis, with or without coma
Warnings are also given regarding the use of metformin in less severe renal impairment, people aged 65 years old or greater, hypoxic states (e.g., acute congestive heart failure), excessive alcohol intake, hepatic impairment, concomitant use of certain drugs (e.g. carbonic anhydrase inhibitors such as topiramate), surgery, and other procedures, or in people having a radiological study with administration of an iodinated contrast agent.
Metformin is recommended to be temporarily discontinued before any procedure involving use of iodinated contrast agents, (such as a contrast-enhanced CT scan or angiogram) due to the increased risk of lactic acidosis resulting from impaired kidney function;[65][66] metformin can be resumed after two days after contrast administration, if renal function is adequate and stable.
Side effects
The most common side effects of metformin is gastrointestinal irritation, including diarrhea, cramps, nausea, vomiting, and increased flatulence; metformin is more commonly associated with gastrointestinal adverse effects than most other antidiabetic medications.[38] The most serious potential adverse effect of metformin is lactic acidosis; this complication is rare, and the vast majority of these cases seem to be related to conditions, such as impaired liver or kidney function, rather than to the metformin itself.[67] Metformin is not approved for use in those with severe kidney disease, but may still be used at lower doses in those with kidney problems.[68]
Gastrointestinal
Gastrointestinal upset can cause severe discomfort; it is most common when metformin is first administered, or when the dose is increased. The discomfort can often be avoided by beginning at a low dose (1.0 to 1.7 grams per day) and increasing the dose gradually, but even with low doses, 5% of people may be unable to tolerate metformin.[69] Use of slow- or extended-release preparations may improve tolerability.[69]
Long-term use of metformin has been associated with increased homocysteine levels[70] and malabsorption of vitamin B12.[71][72] Higher doses and prolonged use are associated with increased incidence of vitamin B12 deficiency,[73] and some researchers recommend screening or prevention strategies.[74]
Lactic acidosis
Lactic acidosis almost never occurs with metformin exposure during routine medical care.[75] Rates of metformin-associated lactic acidosis is about nine per 100,000 person-years, which is similar to the background rate of lactic acidosis in the general population.[76] A systematic review concluded no data exists to definitively link metformin to lactic acidosis.[77]
Metformin is generally safe in people with mild to moderate chronic kidney disease, with proportional reduction of metformin dose according to severity of estimated glomerular filtration rate and with periodic assessment of kidney function, (e.g., periodic plasma creatinine measurement).[78] The FDA recommends avoiding the use of metformin in more severe chronic kidney disease, below the estimated glomerular filtration rate (eGFR) cutoff of 30 mL/minute/1.73 m2.[79] Lactate uptake by the liver is diminished with metformin use because lactate is a substrate for hepatic gluconeogenesis, a process that metformin inhibits. In healthy individuals, this slight excess is cleared by other mechanisms (including uptake by unimpaired kidneys), and no significant elevation in blood levels of lactate occurs.[37] Given severely-impaired kidney function, clearance of metformin and lactate is reduced, increasing levels of both, and possibly causing lactic acid buildup. Because metformin decreases liver uptake of lactate, any condition that may precipitate lactic acidosis is a contraindication. Common causes include alcoholism (due to depletion of NAD+ stores), heart failure and respiratory disease (due to inadequate tissue oxygenation); the most common cause is kidney disease.[80]
Metformin has been suggested as increasing production of lactate in the large intestine, which could potentially contribute to lactic acidosis in those with risk factors.[81] However, the clinical significance of this is unknown, and the risk of metformin-associated lactic acidosis is most commonly attributed to decreased hepatic uptake rather than increased intestinal production.[37][80][82]
The risk of metformin-associated lactic acidosis is also increased by massive overdose of metformin, although even quite large doses are often not fatal.[83]
Overdose
The most common symptoms following overdose include vomiting, diarrhea, abdominal pain, tachycardia, drowsiness, and, rarely, hypoglycemia or hyperglycemia.[84][85] Treatment of metformin overdose is generally supportive, as no specific antidote is known. Extracorporeal treatments are recommended in severe overdoses.[86] Due to metformin's low molecular weight and lack of plasma protein binding, these techniques have the benefit of removing metformin from blood plasma, preventing further lactate overproduction.[86]
Metformin may be quantified in blood, plasma, or serum to monitor therapy, confirm a diagnosis of poisoning, or assist in a forensic death investigation. Blood or plasma metformin concentrations are usually in a range of 1–4 mg/l in persons receiving therapeutic doses, 40–120 mg/l in victims of acute overdosage, and 80–200 mg/l in fatalities. Chromatographic techniques are commonly employed.[87][88]
Interactions
The H2-receptor antagonist cimetidine causes an increase in the plasma concentration of metformin by reducing clearance of metformin by the kidneys;[89] both metformin and cimetidine are cleared from the body by tubular secretion, and both, particularly the cationic (positively charged) form of cimetidine, may compete for the same transport mechanism.[90] A small double-blind, randomized study found the antibiotic cephalexin to also increase metformin concentrations by a similar mechanism;[91] theoretically, other cationic medications may produce the same effect.[90]
Metformin also interacts with anticholinergic medications, due to their effect on gastric motility. Anticholinergic drugs reduce gastric motility, prolonging the time drugs spend in the gastrointestinal tract. This impairment may lead to more metformin being absorbed than without the presence of an anticholinergic drug, thereby increasing the concentration of metformin in the plasma and increasing the risk for adverse effects.[92]
Pharmacology
Mechanism of action
The molecular mechanism of metformin is not completely understood. Multiple potential mechanisms of action have been proposed: inhibition of the mitochondrial respiratory chain (complex I), activation of AMP-activated protein kinase (AMPK), inhibition of glucagon-induced elevation of cyclic adenosine monophosphate (cAMP) with reduced activation of protein kinase A (PKA), inhibition of mitochondrial glycerophosphate dehydrogenase, and an effect on gut microbiota.[93][94][95] Metformin also exerts an anorexiant effect in most people, decreasing caloric intake.[96] Ultimately, it decreases gluconeogenesis (glucose production) in the liver.[81][97] It also has an insulin-sensitizing effect with multiple actions on tissues including the liver, skeletal muscle, endothelium, adipose tissue, and the ovary.[50][98] The average patient with type 2 diabetes has three times the normal rate of gluconeogenesis; metformin treatment reduces this by over one-third.[99]
Activation of AMPK was required for metformin's inhibitory effect on liver glucose production.[100] AMPK is an enzyme that plays an important role in insulin signalling, whole body energy balance and the metabolism of glucose and fats.[101] AMPK Activation was required for an increase in the expression of small heterodimer partner, which in turn inhibited the expression of the hepatic gluconeogenic genes phosphoenolpyruvate carboxykinase and glucose 6-phosphatase.[102] Metformin is frequently used in research along with AICA ribonucleotide as an AMPK agonist. The mechanism by which biguanides increase the activity of AMPK remains uncertain; however, metformin increases the concentration of cytosolic adenosine monophosphate (AMP) (as opposed to a change in total AMP or total AMP/adenosine triphosphate).[103] Increased cellular AMP has been proposed to explain the inhibition of glucagon-induced increase in cAMP and activation of PKA.[93] Metformin and other biguanides may antagonize the action of glucagon, thus reducing fasting glucose levels.[104] Metformin also induces a profound shift in the faecal microbial community profile in diabetic mice and this may contribute to its mode of action possibly through an effect on glucagon-like peptide-1 secretion.[94]
In addition to suppressing hepatic glucose production, metformin increases insulin sensitivity, enhances peripheral glucose uptake (by inducing the phosphorylation of GLUT4 enhancer factor), decreases insulin-induced suppression of fatty acid oxidation,[105] and decreases absorption of glucose from the gastrointestinal tract. Increased peripheral use of glucose may be due to improved insulin binding to insulin receptors.[106] The increase in insulin binding after metformin treatment has also been demonstrated in patients with NIDDM.[107]
AMPK probably also plays a role in increased peripheral insulin sensitivity, as metformin administration increases AMPK activity in skeletal muscle.[108] AMPK is known to cause GLUT4 deployment to the plasma membrane, resulting in insulin-independent glucose uptake. Some metabolic actions of metformin do appear to occur by AMPK-independent mechanisms.
Metformin has indirect antiandrogenic effects in women with insulin resistance, such as those with polycystic ovary syndrome, due to its beneficial effects on insulin sensitivity.[109] It may reduce testosterone levels in such women by as much as 50%.[109] However, a Cochrane review found that metformin was only slightly effective for decreasing androgen levels in women with polycystic ovary syndrome.[110]
Metformin also has significant effects on the gut microbiome, such as its effect on increasing agmatine production by gut bacteria; however, the relative importance of this mechanism compared to other mechanisms is uncertain.[111][112][113]
Pharmacokinetics
Metformin has an oral bioavailability of 50–60% under fasting conditions, and is absorbed slowly.[90][114] Peak plasma concentrations (Cmax) are reached within one to three hours of taking immediate-release metformin and four to eight hours with extended-release formulations.[90][114] The plasma protein binding of metformin is negligible, as reflected by its very high apparent volume of distribution (300–1000 l after a single dose). Steady state is usually reached in one or two days.[90]
Metformin has acid dissociation constant values (pKa) of 2.8 and 11.5, so exists very largely as the hydrophilic cationic species at physiological pH values. The metformin pKa values make it a stronger base than most other basic medications with less than 0.01% nonionized in blood. Furthermore, the lipid solubility of the nonionized species is slight as shown by its low logP value (log(10) of the distribution coefficient of the nonionized form between octanol and water) of −1.43. These chemical parameters indicate low lipophilicity and, consequently, rapid passive diffusion of metformin through cell membranes is unlikely. As a result of its low lipid solubility it requires the transporter SLC22A1 in order for it to enter cells.[115][116] The logP of metformin is less than that of phenformin (−0.84) because two methyl substituents on metformin impart lesser lipophilicity than the larger phenylethyl side chain in phenformin. More lipophilic derivatives of metformin are presently under investigation with the aim of producing prodrugs with superior oral absorption than metformin.[117]
Metformin is not metabolized. It is cleared from the body by tubular secretion and excreted unchanged in the urine; metformin is undetectable in blood plasma within 24 hours of a single oral dose.[90][118] The average elimination half-life in plasma is 6.2 hours.[90] Metformin is distributed to (and appears to accumulate in) red blood cells, with a much longer elimination half-life: 17.6 hours[90] (reported as ranging from 18.5 to 31.5 hours in a single-dose study of nondiabetics).[118]
Chemistry
Metformin hydrochloride (1,1-dimethylbiguanide hydrochloride) is freely-soluble in water, slightly soluble in ethanol, but almost insoluble in acetone, ether, or chloroform. The pKa of metformin is 12.4.[119] The usual synthesis of metformin, originally described in 1922, involves the one-pot reaction of dimethylamine hydrochloride and 2-cyanoguanidine over heat.[120][121]

According to the procedure described in the 1975 Aron patent,[122] and the Pharmaceutical Manufacturing Encyclopedia,[123] equimolar amounts of dimethylamine and 2-cyanoguanidine are dissolved in toluene with cooling to make a concentrated solution, and an equimolar amount of hydrogen chloride is slowly added. The mixture begins to boil on its own, and after cooling, metformin hydrochloride precipitates with a 96% yield.
History

The biguanide class of antidiabetic medications, which also includes the withdrawn agents phenformin and buformin, originates from the French lilac or goat's rue (Galega officinalis), a plant used in folk medicine for several centuries.[124] Galega officinalis itself does not contain any of these medications, but isoamylene guanidine; phenformin, buformin, and metformin are chemically synthesized compounds composed of two guanidine molecules, and are more lipophilic than the plant-derived parent compound.[124]
Metformin was first described in the scientific literature in 1922, by Emil Werner and James Bell, as a product in the synthesis of N,N-dimethylguanidine.[120] In 1929, Slotta and Tschesche discovered its sugar-lowering action in rabbits, finding it the most potent biguanide analog they studied.[125] This result was completely forgotten, as other guanidine analogs, such as the synthalins, took over and were themselves soon overshadowed by insulin.[126]
Interest in metformin resumed at the end of the 1940s. In 1950, metformin, unlike some other similar compounds, was found not to decrease blood pressure and heart rate in animals.[127] That year, Filipino physician Eusebio Y. Garcia[128] used metformin (he named it Fluamine) to treat influenza; he noted the medication "lowered the blood sugar to minimum physiological limit" and was not toxic. Garcia believed metformin to have bacteriostatic, antiviral, antimalarial, antipyretic and analgesic actions.[129] In a series of articles in 1954, Polish pharmacologist Janusz Supniewski[130] was unable to confirm most of these effects, including lowered blood sugar. Instead he observed antiviral effects in humans.[131][132]
French diabetologist Jean Sterne studied the antihyperglycemic properties of galegine, an alkaloid isolated from Galega officinalis, which is related in structure to metformin and had seen brief use as an antidiabetic before the synthalins were developed.[133] Later, working at Laboratoires Aron in Paris, he was prompted by Garcia's report to reinvestigate the blood sugar-lowering activity of metformin and several biguanide analogs. Sterne was the first to try metformin on humans for the treatment of diabetes; he coined the name "Glucophage" (glucose eater) for the medication and published his results in 1957.[126][133]
Metformin became available in the British National Formulary in 1958. It was sold in the UK by a small Aron subsidiary called Rona.[134]
Broad interest in metformin was not rekindled until the withdrawal of the other biguanides in the 1970s. Metformin was approved in Canada in 1972,[135] but did not receive approval by the U.S. Food and Drug Administration (FDA) for type 2 diabetes until 1994.[136] Produced under license by Bristol-Myers Squibb, Glucophage was the first branded formulation of metformin to be marketed in the U.S., beginning on 3 March 1995.[137] Generic formulations are now available in several countries, and metformin is believed to have become the world's most widely prescribed antidiabetic medication.[133]
Society and culture
Cost
The wholesale price in the developed world was between US$0.21 and $5.55 per month as of 2014.[19] In the United States, it costs US$5 to US$25 per month.[2] In 2017, it was the fourth-most commonly prescribed medication in the United States, with more than 78 million prescriptions.[21][22]
.svg.png.webp) Metformin costs (US)
Metformin costs (US).svg.png.webp) Metformin prescriptions (US)
Metformin prescriptions (US)
Environmental
Metformin and its major transformation product guanylurea are present in wastewater treatment plant effluents and regularly detected in surface waters. Guanylurea concentrations above 200 μg L−1 have been measured in a German river which are amongst the highest reported for pharmaceutical transformation products in aquatic environments.[138]
Formulations

The name "metformin" is the BAN, USAN and INN for this medication, and is sold under several trade names. Common brand names include Glucophage, Riomet, Fortamet, and Glumetza in the US.[139] In other areas of the world, there is also Obimet, Gluformin, Dianben, Diabex, Diaformin, Metsol, Siofor, Metfogamma and Glifor.[140][141] There are several formulations of Metformin available to the market, and all but the liquid form have generic equivalents.[139] Metformin IR (immediate release) is available in 500, 850, and 1000-mg tablets, while Metformin XR (extended release) is available in 500, 750, and 1000-mg strengths (also sold as Fortamet, Glumetza, and Glucophage XR in the US). The use of an extended release formulation is to counteract common gastrointestinal adverse effects, as well as to increase compliance by reducing pill burden and therefore can improve adherence, at the expense of the pill's larger size. Also available is liquid metformin (sold only as Riomet in the US), where 5 mL of solution contains the same amount of drug as a 500 mg tablet. The use of a liquid form can be beneficial in helping those with physical or psychological swallowing problems take the medication, or to potentially reduce the number of steps needed to take the medication.
Combination with other medications
When used for type 2 diabetes, metformin is often prescribed in combination with other medications.
Several are available as fixed-dose combinations, with the potential to reduce pill burden, decrease cost, and simplify administration.[142][143]
Thiazolidinediones (glitazones)
Rosiglitazone
A combination of metformin and rosiglitazone was released in 2002, and sold as Avandamet by GlaxoSmithKline,[144] or as a generic medication.[145] Formulations are in 500 mg/1 mg, 500 mg/2 mg, 500 mg/4 mg, 1 g/2 mg, and 1 g/4 mg of metformin/rosiglitazone.
By 2009 it had become the most popular metformin combination.[146]
In 2005, the stock of Avandamet was removed from the market, after inspections showed the factory where it was produced was violating good manufacturing practices.[147] The medication pair continued to be prescribed separately and Avandamet was again available by the end of that year. A generic formulation of metformin/rosiglitazone from Teva received tentative approval from the FDA and reached the market in early 2012.[148]
However, following a meta-analysis in 2007 that linked the medication's use to an increased risk of heart attack,[149] concerns were raised over the safety of medicines containing rosiglitazone. In September 2010 the European Medicines Agency (EMA) recommended that the medication be suspended from the European market because the benefits of rosiglitazone no longer outweighed the risks.[150][151]
It was withdrawn from the market in the UK and India in 2010,[152] and in New Zealand and South Africa in 2011.[153] From November 2011 until November 2013 the FDA[154] did not allow rosiglitazone or metformin/rosiglitazone to be sold without a prescription; moreover, makers were required to notify patients of the risks associated with its use, and the drug had to be purchased by mail order through specified pharmacies.[155]
In November 2013, the FDA lifted its earlier restrictions on rosiglitazone after reviewing the results of the 2009 RECORD clinical trial (a six-year, open label randomized control trial), which failed to show elevated risk of heart attack or death associated with the medication.[156][157][158]
Pioglitazone
The combination of metformin and pioglitazone (Actoplus Met, Piomet, Politor, Glubrava) is available in the US and in the European Union.[159][160][161][162][163]
DPP-4 inhibitors
Dipeptidyl peptidase-4 inhibitors inhibit dipeptidyl peptidase-4 and thus reduce glucagon and blood glucose levels.
DPP-4 inhibitors combined with metformin include a sitagliptin/metformin combination (Janumet),[164][165] a saxagliptin/metformin combination (Kombiglyze XR, Komboglyze),[166][167] and an alogliptin/metformin combination (Kazano, Vipdomet).[168][169]
Metformin combined with linagliptin is marketed under the trade name Jentadueto.[170][171]
Sulfonylureas
Sulfonylureas act by increasing insulin release from the beta cells in the pancreas.[172] They often can be used as secondary therapy if metformin alone is not sufficiently effective at reaching normal blood glucose levels.
Metformin is available combined with the sulfonylureas glipizide (Metaglip) and glibenclamide (US: glyburide) (Glucovance). Generic formulations of metformin/glipizide and metformin/glibenclamide are available (the latter is more popular).[173]
Meglitinide
Meglitinides are similar to sulfonylureas, as they bind to beta cells in the pancreas, but differ by the site of binding to the intended receptor and the drug's affinity to the receptor.[172] As a result, they have a shorter duration of action compared to sulfonylureas, and require higher blood glucose levels to begin to secrete insulin. Both meglitinides, known as nateglinide and repanglinide, is sold in formulations combined with metformin. A repaglinide/metformin combination is sold as Prandimet, or as its generic equivalent.[174][175]
Triple combination
The combination of metformin wiih dapagliflozen and saxagliptin, is available in the United States as Qternmet XR.[176]
The combination of metformin with pioglitazone and glibenclamide[177] is available in India as Accuglim-MP, Adglim MP, and Alnamet-GP, along with the Philippines as Tri-Senza.[141]
The combination of metformin with pioglitazone and lipoic acid is available in Turkey as Pional.[141]
Impurities
In December 2019, the U.S. Food and Drug Administration (FDA) announced that it learned that some metformin medicines manufactured outside the United States might contain a nitrosamine impurity called N-nitrosodimethylamine (NDMA), classified as a probable human carcinogen, at low levels.[178] Health Canada announced that it was assessing NDMA levels in metformin.[179]
In February 2020, the FDA found NDMA levels in some tested metformin samples that did not exceed the acceptable daily intake.[180][181]
In February 2020, Health Canada announced a recall of Apotex immediate-release metformin,[182] followed in March by recalls of Ranbaxy metformin[183] and in March by Jamp metformin.[184]
On 29 May 2020, the FDA asked five companies to voluntarily recall their sustained-release metformin products.[185][186][187][188][189][190] The five companies were not named, but they were revealed to be Amneal Pharmaceuticals, Actavis Pharma, Apotex Corp, Lupin Pharma, and Marksans Pharma Limited in a letter sent to Valisure, the pharmacy that had first alerted the FDA to this contaminant in metformin via a Citizen Petition.[191]
In June 2020, the FDA posted its laboratory results showing NDMA amounts in metformin products it tested.[192] It found NDMA in certain lots of extended release (ER) metformin and is recommending companies recall lots with levels of NDMA above the acceptable intake limit of 96 nanograms per day.[192] The FDA is also collaborating with international regulators to share testing results for metformin.[192]
In July 2020, Lupin Pharmaceuticals pulled all lots (batches) of metformin after discovering unacceptably high levels of NDMA in tested samples.[193]
Research
Metformin has been studied for its effects on multiple other conditions, including:
- Non-alcoholic fatty liver disease[194][195][196]
- Premature puberty[196][197]
- Cancer[140][198][199]
- Cardiovascular disease in people with diabetes[200]
While metformin may reduce body weight in persons with fragile X syndrome, it is uncertain whether it improves neurological or psychiatric symptoms.[201] Metformin has been studied in vivo (C. elegans and crickets) for effects on aging.[116][202] A 2017 review found that people with diabetes who were taking metformin had lower all-cause mortality. They also had reduced cancer and cardiovascular disease compared with those on other therapies.[200]
References
- ↑ Sirtori CR, Franceschini G, Galli-Kienle M, Cighetti G, Galli G, Bondioli A, Conti F (December 1978). "Disposition of metformin (N,N-dimethylbiguanide) in man". Clinical Pharmacology and Therapeutics. 24 (6): 683–93. doi:10.1002/cpt1978246683. PMID 710026.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 "Metformin Hydrochloride". The American Society of Health-System Pharmacists. Archived from the original on 24 December 2016. Retrieved 2 January 2017.
- 1 2 3 4 "METFORMIN oral - Essential drugs". medicalguidelines.msf.org. Archived from the original on 29 August 2021. Retrieved 31 August 2020.
- 1 2 "Metformin Use During Pregnancy". Drugs.com. 10 September 2019. Archived from the original on 16 April 2020. Retrieved 4 February 2020.
- 1 2 "WHOCC - ATC/DDD Index". www.whocc.no. Archived from the original on 17 September 2020. Retrieved 31 August 2020.
- 1 2 3 4 5 Dunn CJ, Peters DH (May 1995). "Metformin. A review of its pharmacological properties and therapeutic use in non-insulin-dependent diabetes mellitus". Drugs. 49 (5): 721–49. doi:10.2165/00003495-199549050-00007. PMID 7601013.
- ↑ Hundal RS, Inzucchi SE (2003). "Metformin: new understandings, new uses". Drugs. 63 (18): 1879–94. doi:10.2165/00003495-200363180-00001. PMID 12930161.
- ↑ "metformin_msds". Archived from the original on 12 June 2017. Retrieved 2 August 2020.
- ↑ Maruthur NM, Tseng E, Hutfless S, Wilson LM, Suarez-Cuervo C, Berger Z, Chu Y, Iyoha E, Segal JB, Bolen S (June 2016). "Diabetes Medications as Monotherapy or Metformin-Based Combination Therapy for Type 2 Diabetes: A Systematic Review and Meta-analysis". Annals of Internal Medicine. 164 (11): 740–51. doi:10.7326/M15-2650. PMID 27088241.
- ↑ Clinical Obesity (2nd ed.). Oxford: John Wiley & Sons. 2008. p. 262. ISBN 978-0-470-98708-7. Archived from the original on 8 September 2017.
- ↑ "Type 2 diabetes and metformin. First choice for monotherapy: weak evidence of efficacy but well-known and acceptable adverse effects". Prescrire International. 23 (154): 269–72. November 2014. PMID 25954799.
- ↑ Triggle CR, Ding H (January 2017). "Metformin is not just an antihyperglycaemic drug but also has protective effects on the vascular endothelium". Acta Physiologica. 219 (1): 138–151. doi:10.1111/apha.12644. PMID 26680745.
- ↑ Blumenberg A, Benabbas R, Sinert R, Jeng A, Wiener SW (April 2020). "Do Patients Die with or from Metformin-Associated Lactic Acidosis (MALA)? Systematic Review and Meta-analysis of pH and Lactate as Predictors of Mortality in MALA". J Med Toxicol. 16 (2): 222–229. doi:10.1007/s13181-019-00755-6. PMID 31907741.
- ↑ Lipska KJ, Bailey CJ, Inzucchi SE (June 2011). "Use of metformin in the setting of mild-to-moderate renal insufficiency". Diabetes Care. 34 (6): 1431–7. doi:10.2337/dc10-2361. PMC 3114336. PMID 21617112.
- ↑ Lautatzis ME, Goulis DG, Vrontakis M (November 2013). "Efficacy and safety of metformin during pregnancy in women with gestational diabetes mellitus or polycystic ovary syndrome: a systematic review". Metabolism. 62 (11): 1522–34. doi:10.1016/j.metabol.2013.06.006. PMID 23886298.
- 1 2 3 Fischer, Janos (2010). Analogue-based Drug Discovery II. John Wiley & Sons. p. 49. ISBN 978-3-527-63212-1. Archived from the original on 8 September 2017.
- ↑ McKee, Mitchell Bebel Stargrove, Jonathan Treasure, Dwight L. (2008). Herb, nutrient, and drug interactions : clinical implications and therapeutic strategies. St. Louis, Mo.: Mosby/Elsevier. p. 217. ISBN 978-0-323-02964-3. Archived from the original on 8 September 2017.
- ↑ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- 1 2 "Metformin". Archived from the original on 3 August 2017. Retrieved 11 January 2016.
- ↑ Hitchings, Andrew; Lonsdale, Dagan; Burrage, Daniel; Baker, Emma (2019). The Top 100 Drugs: Clinical Pharmacology and Practical Prescribing (2nd ed.). Elsevier. pp. 154–155. ISBN 978-0-7020-7442-4. Archived from the original on 22 May 2021. Retrieved 9 November 2021.
- 1 2 "The Top 300 of 2020". ClinCalc. Archived from the original on 12 February 2021. Retrieved 7 April 2020.
- 1 2 "Metformin Hydrochloride - Drug Usage Statistics". ClinCalc. 23 December 2019. Archived from the original on 19 May 2021. Retrieved 7 April 2020.
- ↑ Lord JM, Flight IH, Norman RJ (October 2003). "Metformin in polycystic ovary syndrome: systematic review and meta-analysis". BMJ. 327 (7421): 951–3. doi:10.1136/bmj.327.7421.951. PMC 259161. PMID 14576245.
- ↑ Bennett WL, Maruthur NM, Singh S, Segal JB, Wilson LM, Chatterjee R, Marinopoulos SS, Puhan MA, Ranasinghe P, Block L, Nicholson WK, Hutfless S, Bass EB, Bolen S (May 2011). "Comparative effectiveness and safety of medications for type 2 diabetes: an update including new drugs and 2-drug combinations". Annals of Internal Medicine. 154 (9): 602–13. doi:10.7326/0003-4819-154-9-201105030-00336. PMC 3733115. PMID 21403054.
- 1 2 Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, Peters AL, Tsapas A, Wender R, Matthews DR (June 2012). "Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD)". Diabetes Care. 35 (6): 1364–79. doi:10.2337/dc12-0413. PMC 3357214. PMID 22517736.
- ↑ Qaseem A, Humphrey LL, Sweet DE, Starkey M, Shekelle P (February 2012). "Oral pharmacologic treatment of type 2 diabetes mellitus: a clinical practice guideline from the American College of Physicians". Annals of Internal Medicine. 156 (3): 218–31. doi:10.7326/0003-4819-156-3-201202070-00011. PMID 22312141.
- ↑ Jia Y, Lao Y, Zhu H, et al. (January 2019). "Is metformin still the most efficacious first-line oral hypoglycaemic drug in treating type 2 diabetes? A network meta-analysis of randomized controlled trials". Obes Rev. 20 (1): 1–12. doi:10.1111/obr.12753. PMID 30230172.
- ↑ "Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group". Lancet. 352 (9131): 854–65. September 1998. doi:10.1016/S0140-6736(98)07037-8. PMID 9742977.
- ↑ Selvin E, Bolen S, Yeh HC, Wiley C, Wilson LM, Marinopoulos SS, Feldman L, Vassy J, Wilson R, Bass EB, Brancati FL (October 2008). "Cardiovascular outcomes in trials of oral diabetes medications: a systematic review". Archives of Internal Medicine. 168 (19): 2070–80. doi:10.1001/archinte.168.19.2070. PMC 2765722. PMID 18955635.
- ↑ Boussageon R, Supper I, Bejan-Angoulvant T, Kellou N, Cucherat M, Boissel JP, Kassai B, Moreau A, Gueyffier F, Cornu C (2012). "Reappraisal of metformin efficacy in the treatment of type 2 diabetes: a meta-analysis of randomised controlled trials". PLOS Medicine. 9 (4): e1001204. doi:10.1371/journal.pmed.1001204. PMC 3323508. PMID 22509138.
- ↑ Crowley MJ, Diamantidis CJ, McDuffie JR, Cameron CB, Stanifer JW, Mock CK, Wang X, Tang S, Nagi A, Kosinski AS, Williams JW (February 2017). "Clinical Outcomes of Metformin Use in Populations With Chronic Kidney Disease, Congestive Heart Failure, or Chronic Liver Disease: A Systematic Review". Annals of Internal Medicine. 166 (3): 191–200. doi:10.7326/M16-1901. PMC 5293600. PMID 28055049.
- ↑ Rydén L, Grant PJ, Anker SD, Berne C, Cosentino F, Danchin N, Deaton C, Escaned J, Hammes HP, Huikuri H, Marre M, Marx N, Mellbin L, Ostergren J, Patrono C, Seferovic P, Uva MS, Taskinen MR, Tendera M, Tuomilehto J, Valensi P, Zamorano JL (May 2014). "ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD—summary". Diabetes & Vascular Disease Research. 11 (3): 133–73. doi:10.1177/1479164114525548. PMID 24800783.
- ↑ Hemmingsen B, Schroll JB, Wetterslev J, Gluud C, Vaag A, Sonne DP, Lundstrøm LH, Almdal T (July 2014). "Sulfonylurea versus metformin monotherapy in patients with type 2 diabetes: a Cochrane systematic review and meta-analysis of randomized clinical trials and trial sequential analysis". CMAJ Open. 2 (3): E162–75. doi:10.9778/cmajo.20130073. PMC 4185978. PMID 25295236.
- 1 2 Johansen K (January 1999). "Efficacy of metformin in the treatment of NIDDM. Meta-analysis". Diabetes Care. 22 (1): 33–7. doi:10.2337/diacare.22.1.33. ISSN 0149-5992. PMID 10333900.
- ↑ Golay A (January 2008). "Metformin and body weight". International Journal of Obesity. 32 (1): 61–72. doi:10.1038/sj.ijo.0803695. PMID 17653063.
- ↑ Mead E, Atkinson G, Richter B, Metzendorf MI, Baur L, Finer N, Corpeleijn E, O'Malley C, Ells LJ (November 2016). "Drug interventions for the treatment of obesity in children and adolescents". The Cochrane Database of Systematic Reviews. 11: CD012436. doi:10.1002/14651858.CD012436. hdl:10149/620651. PMC 6472619. PMID 27899001.
- 1 2 3 4 Maharani U (2009). "Chapter 27: Diabetes Mellitus & Hypoglycemia". In Papadakis MA, McPhee SJ (eds.). Current Medical Diagnosis and Treatment 2010 (49th ed.). McGraw-Hill Medical. pp. 1092–93. ISBN 978-0-07-162444-2.
- 1 2 3 Bolen S, Feldman L, Vassy J, Wilson L, Yeh HC, Marinopoulos S, Wiley C, Selvin E, Wilson R, Bass EB, Brancati FL (September 2007). "Systematic review: comparative effectiveness and safety of oral medications for type 2 diabetes mellitus". Annals of Internal Medicine. 147 (6): 386–99. doi:10.7326/0003-4819-147-6-200709180-00178. PMID 17638715.
- ↑ DiPiro, Joseph T.; Talbert, Robert L.; Yee, Gary C.; Matzke, Gary R.; Wells, Barbara G.; Posey, L. Michael (2005). Pharmacotherapy: a pathophysiologic approach. New York: McGraw-Hill. ISBN 978-0-07-141613-9.
- ↑ "Glucophage package insert" Archived 29 August 2021 at the Wayback Machine. Princeton, NJ: Bristol-Myers Squibb Company; 2009.
- 1 2 Morley LC, Tang T, Yasmin E, et al. (November 2017). "Insulin-sensitising drugs (metformin, rosiglitazone, pioglitazone, D-chiro-inositol) for women with polycystic ovary syndrome, oligo amenorrhoea and subfertility". Cochrane Database Syst Rev. 11: CD003053. doi:10.1002/14651858.CD003053.pub6. PMC 6486196. PMID 29183107.
Our updated review suggests that metformin alone may be beneficial over placebo for live birth, although the evidence quality was low.
- ↑ Ghazeeri GS, Nassar AH, Younes Z, Awwad JT (June 2012). "Pregnancy outcomes and the effect of metformin treatment in women with polycystic ovary syndrome: an overview". Acta Obstetricia et Gynecologica Scandinavica. 91 (6): 658–78. doi:10.1111/j.1600-0412.2012.01385.x. PMID 22375613.
- ↑ Kumar P, Khan K (May 2012). "Effects of metformin use in pregnant patients with polycystic ovary syndrome". Journal of Human Reproductive Sciences. 5 (2): 166–9. doi:10.4103/0974-1208.101012. PMC 3493830. PMID 23162354.
- ↑ Tay CT, Joham AE, Hiam DS, et al. (November 2018). "Pharmacological and surgical treatment of nonreproductive outcomes in polycystic ovary syndrome: An overview of systematic reviews". Clinical Endocrinology. 89 (5): 535–53. doi:10.1111/cen.13753. PMID 29846959.
- ↑ Tso LO, Costello MF, Albuquerque LE, et al. (November 2014). "Metformin treatment before and during IVF or ICSI in women with polycystic ovary syndrome". Cochrane Database Syst Rev (11): CD006105. doi:10.1002/14651858.CD006105.pub3. PMC 6953331. PMID 25406011.
- ↑ Dodd JM, Grivell RM, Deussen AR, et al. (July 2018). "Metformin for women who are overweight or obese during pregnancy for improving maternal and infant outcomes". Cochrane Database Syst Rev. 7: CD010564. doi:10.1002/14651858.CD010564.pub2. PMC 6513233. PMID 30039871.
- ↑ National Collaborating Centre for Women's and Children's Health (2004). Fertility: assessment and treatment for people with fertility problems (PDF). London: Royal College of Obstetricians and Gynaecologists. pp. 58–59. ISBN 978-1-900364-97-3. Archived (PDF) from the original on 11 July 2009.
- ↑ Balen A (December 2008). "Metformin therapy for the management of infertility in women with polycystic ovary syndrome" (PDF). Scientific Advisory Committee Opinion Paper 13. Royal College of Obstetricians and Gynaecologists. Archived from the original (PDF) on 18 December 2009. Retrieved 13 December 2009.
- ↑ The Thessaloniki ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group (March 2008). "Consensus on infertility treatment related to polycystic ovary syndrome". Human Reproduction. 23 (3): 462–77. doi:10.1093/humrep/dem426. PMID 18308833.
- 1 2 Diamanti-Kandarakis E, Economou F, Palimeri S, Christakou C (September 2010). "Metformin in polycystic ovary syndrome". Annals of the New York Academy of Sciences. 1205 (1): 192–8. Bibcode:2010NYASA1205..192D. doi:10.1111/j.1749-6632.2010.05679.x. PMID 20840272.
- ↑ Diamanti-Kandarakis E, Christakou CD, Kandaraki E, Economou FN (February 2010). "Metformin: an old medication of new fashion: evolving new molecular mechanisms and clinical implications in polycystic ovary syndrome". European Journal of Endocrinology. 162 (2): 193–212. doi:10.1530/EJE-09-0733. PMID 19841045.
- ↑ Butalia S, Gutierrez L, Lodha A, Aitken E, Zakariasen A, Donovan L (January 2017). "Short- and long-term outcomes of metformin compared with insulin alone in pregnancy: a systematic review and meta-analysis". Diabetic Medicine. 34 (1): 27–36. doi:10.1111/dme.13150. PMID 27150509.
- ↑ Nicholson W, Bolen S, Witkop CT, Neale D, Wilson L, Bass E (January 2009). "Benefits and risks of oral diabetes agents compared with insulin in women with gestational diabetes: a systematic review". Obstetrics and Gynecology. 113 (1): 193–205. doi:10.1097/AOG.0b013e318190a459. PMID 19104375.
- ↑ Kitwitee P, Limwattananon S, Limwattananon C, Waleekachonlert O, Ratanachotpanich T, Phimphilai M, Nguyen TV, Pongchaiyakul C (September 2015). "Metformin for the treatment of gestational diabetes: An updated meta-analysis". Diabetes Research and Clinical Practice. 109 (3): 521–32. doi:10.1016/j.diabres.2015.05.017. PMID 26117686.
- 1 2 Balsells M, García-Patterson A, Solà I, Roqué M, Gich I, Corcoy R (January 2015). "Glibenclamide, metformin, and insulin for the treatment of gestational diabetes: a systematic review and meta-analysis". BMJ (Systematic Review & Meta-Analysis). 350: h102. doi:10.1136/bmj.h102. PMC 4301599. PMID 25609400.
- ↑ Alqudah A, McKinley MC, McNally R, et al. (February 2018). "Risk of pre-eclampsia in women taking metformin: a systematic review and meta-analysis". Diabet. Med. 35 (2): 160–172. doi:10.1111/dme.13523. PMID 29044702. Archived from the original on 3 November 2017. Retrieved 2 August 2020.
- ↑ Sivalingam VN, Myers J, Nicholas S, Balen AH, Crosbie EJ (2014). "Metformin in reproductive health, pregnancy and gynaecological cancer: established and emerging indications". Human Reproduction Update. 20 (6): 853–68. doi:10.1093/humupd/dmu037. PMID 25013215.
- ↑ Tarry-Adkins JL, Aiken CE, Ozanne SE (August 2019). "Neonatal, infant, and childhood growth following metformin versus insulin treatment for gestational diabetes: A systematic review and meta-analysis". PLOS Med. 16 (8): e1002848. doi:10.1371/journal.pmed.1002848. PMC 6684046. PMID 31386659.
- ↑ Yerevanian A, Soukas AA (June 2019). "Metformin: Mechanisms in Human Obesity and Weight Loss". Current Obesity Reports. 8 (2): 156–64. doi:10.1007/s13679-019-00335-3. PMC 6520185. PMID 30874963.
- ↑ Choi YJ (2015). "Efficacy of adjunctive treatments added to olanzapine or clozapine for weight control in patients with schizophrenia: a systematic review and meta-analysis". TheScientificWorldJournal. 2015: 1–10. doi:10.1155/2015/970730. PMC 4310265. PMID 25664341.
- ↑ Praharaj SK, Jana AK, Goyal N, Sinha VK (March 2011). "Metformin for olanzapine-induced weight gain: a systematic review and meta-analysis". British Journal of Clinical Pharmacology. 71 (3): 377–82. doi:10.1111/j.1365-2125.2010.03783.x. PMC 3045546. PMID 21284696.
- ↑ Siskind DJ, Leung J, Russell AW, Wysoczanski D, Kisely S (2016). "Metformin for Clozapine Associated Obesity: A Systematic Review and Meta-Analysis". PLOS ONE. 11 (6): e0156208. Bibcode:2016PLoSO..1156208S. doi:10.1371/journal.pone.0156208. PMC 4909277. PMID 27304831.
- ↑ Vella S, Buetow L, Royle P, Livingstone S, Colhoun HM, Petrie JR (May 2010). "The use of metformin in type 1 diabetes: a systematic review of efficacy". Diabetologia. 53 (5): 809–20. doi:10.1007/s00125-009-1636-9. PMID 20057994.
- ↑ Badr, D.; Kurban, M.; Abbas, O. (2013). "Metformin in dermatology: an overview". Journal of the European Academy of Dermatology and Venereology. 27 (11): 1329–1335. doi:10.1111/jdv.12116. ISSN 1468-3083. Archived from the original on 22 September 2021. Retrieved 19 September 2021.
- ↑ Weir J (19 March 1999). Guidelines with Regard to Metformin-Induced Lactic Acidosis and X-ray Contrast Medium Agents. Royal College of Radiologists. Retrieved 26 October 2007 through the Internet Archive.
- ↑ Thomsen HS, Morcos SK (August 2003). "Contrast media and the kidney: European Society of Urogenital Radiology (ESUR) guidelines". The British Journal of Radiology. 76 (908): 513–8. doi:10.1259/bjr/26964464. PMID 12893691.
- ↑ Khurana R, Malik IS (January 2010). "Metformin: safety in cardiac patients". Heart. 96 (2): 99–102. doi:10.1136/hrt.2009.173773. PMID 19564648.
- ↑ Heaf, J (June 2014). "Metformin in chronic kidney disease: time for a rethink". Peritoneal Dialysis International. 34 (4): 353–7. doi:10.3747/pdi.2013.00344. PMC 4079480. PMID 24711640.
- 1 2 Fujita Y, Inagaki N (January 2017). "Metformin: New Preparations and Nonglycemic Benefits". Current Diabetes Reports. 17 (1): 5. doi:10.1007/s11892-017-0829-8. PMID 28116648.
- ↑ Wulffelé MG, Kooy A, Lehert P, Bets D, Ogterop JC, Borger van der Burg B, Donker AJ, Stehouwer CD (November 2003). "Effects of short-term treatment with metformin on serum concentrations of homocysteine, folate and vitamin B12 in type 2 diabetes mellitus: a randomized, placebo-controlled trial". Journal of Internal Medicine. 254 (5): 455–63. doi:10.1046/j.1365-2796.2003.01213.x. PMID 14535967. S2CID 12507226.
- ↑ Andrès E, Noel E, Goichot B (October 2002). "Metformin-associated vitamin B12 deficiency". Archives of Internal Medicine. 162 (19): 2251–2. doi:10.1001/archinte.162.19.2251-a. PMID 12390080.
- ↑ Gilligan MA (February 2002). "Metformin and vitamin B12 deficiency". Archives of Internal Medicine. 162 (4): 484–5. doi:10.1001/archinte.162.4.484. PMID 11863489.
- ↑ de Jager J, Kooy A, Lehert P, Wulffelé MG, van der Kolk J, Bets D, Verburg J, Donker AJ, Stehouwer CD (May 2010). "Long term treatment with metformin in patients with type 2 diabetes and risk of vitamin B-12 deficiency: randomised placebo controlled trial". BMJ. 340: c2181. doi:10.1136/bmj.c2181. PMC 2874129. PMID 20488910.
- ↑ Ting RZ, Szeto CC, Chan MH, Ma KK, Chow KM (October 2006). "Risk factors of vitamin B(12) deficiency in patients receiving metformin". Archives of Internal Medicine. 166 (18): 1975–9. doi:10.1001/archinte.166.18.1975. PMID 17030830.
- ↑ Nathan DM, Buse JB, Davidson MB, et al. (January 2009). "Medical management of hyperglycaemia in type 2 diabetes mellitus: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes". Diabetologia. 52 (1): 17–30. doi:10.1007/s00125-008-1157-y. PMID 18941734.
- ↑ Stang M, Wysowski DK, Butler-Jones D (June 1999). "Incidence of lactic acidosis in metformin users". Diabetes Care. 22 (6): 925–7. doi:10.2337/diacare.22.6.925. PMID 10372243.
- ↑ Salpeter SR, Greyber E, Pasternak GA, Salpeter EE (November 2003). "Risk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitus: systematic review and meta-analysis". Archives of Internal Medicine. 163 (21): 2594–602. doi:10.1001/archinte.163.21.2594. PMID 14638559.
- ↑ Inzucchi SE, Lipska KJ, Mayo H, et al. (2014). "Metformin in patients with type 2 diabetes and kidney disease: a systematic review". JAMA. 312 (24): 2668–75. doi:10.1001/jama.2014.15298. PMC 4427053. PMID 25536258.
- ↑ "FDA Drug Safety Communication: FDA revises warnings regarding use of the diabetes medicine metformin in certain patients with reduced kidney function". U.S. Food and Drug Administration (FDA). 14 November 2017. Archived from the original on 25 May 2021. Retrieved 21 December 2018.
- 1 2 Shu AD, Myers MG, Shoelson SE (2005). "Chapter 29: Pharmacology of the Endocrine Pancreas". In Golan ED, Tashjian AH, Armstrong EJ, Galanter JM, Armstrong AW, Arnaout RA, Rose HS (eds.). Principles of pharmacology: the pathophysiologic basis of drug therapy. Philadelphia: Lippincott, Williams & Wilkins. pp. 540–41. ISBN 978-0-7817-4678-6.
- 1 2 Kirpichnikov D, McFarlane SI, Sowers JR (July 2002). "Metformin: an update". Annals of Internal Medicine. 137 (1): 25–33. doi:10.7326/0003-4819-137-1-200207020-00009. PMID 12093242.
- ↑ Davis SN (2006). "Chapter 60: Insulin, Oral Hypoglycemic Agents, and the Pharmacology of the Endocrine Pancreas". In Brunton L, Lazo J, Parker K (eds.). Goodman & Gilman's The Pharmacological Basis of Therapeutics (11th ed.). New York: McGraw-Hill. ISBN 978-0-07-142280-2.
- ↑ Teale KF, Devine A, Stewart H, Harper NJ (July 1998). "The management of metformin overdose". Anaesthesia. 53 (7): 698–701. doi:10.1046/j.1365-2044.1998.436-az0549.x. PMID 9771180.
- ↑ Forrester MB (July 2008). "Adult metformin ingestions reported to Texas poison control centers, 2000-2006". Human & Experimental Toxicology. 27 (7): 575–83. CiteSeerX 10.1.1.1031.9486. doi:10.1177/0960327108090589. PMID 18829734.
- ↑ Suchard JR, Grotsky TA (August 2008). "Fatal metformin overdose presenting with progressive hyperglycemia". The Western Journal of Emergency Medicine. 9 (3): 160–4. PMC 2672258. PMID 19561734.
- 1 2 Calello DP, Liu KD, Wiegand TJ, Roberts DM, Lavergne V, Gosselin S, Hoffman RS, Nolin TD, Ghannoum M (August 2015). "Extracorporeal Treatment for Metformin Poisoning: Systematic Review and Recommendations From the Extracorporeal Treatments in Poisoning Workgroup". Critical Care Medicine. 43 (8): 1716–30. doi:10.1097/CCM.0000000000001002. PMID 25860205.
- ↑ Liu A, Coleman SP (November 2009). "Determination of metformin in human plasma using hydrophilic interaction liquid chromatography-tandem mass spectrometry". Journal of Chromatography B. 877 (29): 3695–700. doi:10.1016/j.jchromb.2009.09.020. PMID 19783231.
- ↑ R. Baselt, Disposition of Toxic Drugs and Chemicals in Man, 8th edition, Biomedical Publications, Foster City, CA, 2008, pp. 939–940.
- ↑ Somogyi A, Stockley C, Keal J, Rolan P, Bochner F (May 1987). "Reduction of metformin renal tubular secretion by cimetidine in man". British Journal of Clinical Pharmacology. 23 (5): 545–51. doi:10.1111/j.1365-2125.1987.tb03090.x. PMC 1386190. PMID 3593625.
- 1 2 3 4 5 6 7 8 Bristol-Myers Squibb (27 August 2008). "Glucophage (metformin hydrochloride tablets) Label Information" (PDF). U.S. Food and Drug Administration (FDA). Archived (PDF) from the original on 22 September 2010. Retrieved 8 December 2009.
- ↑ Jayasagar G, Krishna Kumar M, Chandrasekhar K, Madhusudan Rao C, Madhusudan Rao Y (2002). "Effect of cephalexin on the pharmacokinetics of metformin in healthy human volunteers". Drug Metabolism and Drug Interactions. 19 (1): 41–8. doi:10.1515/dmdi.2002.19.1.41. PMID 12222753.
- ↑ May M, Schindler C (April 2016). "Clinically and pharmacologically relevant interactions of antidiabetic drugs". Therapeutic Advances in Endocrinology and Metabolism. 7 (2): 69–83. doi:10.1177/2042018816638050. PMC 4821002. PMID 27092232.
- 1 2 Rena G, Pearson ER, Sakamoto K (September 2013). "Molecular mechanism of action of metformin: old or new insights?". Diabetologia. 56 (9): 1898–906. doi:10.1007/s00125-013-2991-0. PMC 3737434. PMID 23835523.
- 1 2 Burcelin R (May 2014). "The antidiabetic gutsy role of metformin uncovered?". Gut. 63 (5): 706–7. doi:10.1136/gutjnl-2013-305370. PMID 23840042.
- ↑ Madiraju AK, Erion DM, Rahimi Y, Zhang XM, Braddock DT, Albright RA, Prigaro BJ, Wood JL, Bhanot S, MacDonald MJ, Jurczak MJ, Camporez JP, Lee HY, Cline GW, Samuel VT, Kibbey RG, Shulman GI (June 2014). "Metformin suppresses gluconeogenesis by inhibiting mitochondrial glycerophosphate dehydrogenase". Nature. 510 (7506): 542–6. Bibcode:2014Natur.510..542M. doi:10.1038/nature13270. PMC 4074244. PMID 24847880.
- ↑ Pappachan JM, Viswanath AK (January 2017). "Medical Management of Diabesity: Do We Have Realistic Targets?". Curr. Diab. Rep. 17 (1): 4. doi:10.1007/s11892-017-0828-9. PMID 28101792.
- ↑ Triggle CR, Ding H (2017). "Metformin is not just an antihyperglycaemic drug but also has protective effects on the vascular endothelium". Acta Physiologica. 219 (1): 138–151. doi:10.1111/apha.12644. PMID 26680745.
- ↑ Lord JM, Flight IH, Norman RJ (October 2003). "Metformin in polycystic ovary syndrome: systematic review and meta-analysis". BMJ. 327 (7421): 951–3. doi:10.1136/bmj.327.7421.951. PMC 259161. PMID 14576245.
- ↑ Hundal RS, Krssak M, Dufour S, Laurent D, Lebon V, Chandramouli V, Inzucchi SE, Schumann WC, Petersen KF, Landau BR, Shulman GI (December 2000). "Mechanism by which metformin reduces glucose production in type 2 diabetes". Diabetes. 49 (12): 2063–9. doi:10.2337/diabetes.49.12.2063. PMC 2995498. PMID 11118008.
- ↑ Zhou G, Myers R, Li Y, Chen Y, Shen X, Fenyk-Melody J, Wu M, Ventre J, Doebber T, Fujii N, Musi N, Hirshman MF, Goodyear LJ, Moller DE (October 2001). "Role of AMP-activated protein kinase in mechanism of metformin action". The Journal of Clinical Investigation. 108 (8): 1167–74. doi:10.1172/JCI13505. PMC 209533. PMID 11602624.
- ↑ Towler MC, Hardie DG (February 2007). "AMP-activated protein kinase in metabolic control and insulin signaling". Circulation Research. 100 (3): 328–41. doi:10.1161/01.RES.0000256090.42690.05. PMID 17307971.
- ↑ Kim YD, Park KG, Lee YS, Park YY, Kim DK, Nedumaran B, Jang WG, Cho WJ, Ha J, Lee IK, Lee CH, Choi HS (February 2008). "Metformin inhibits hepatic gluconeogenesis through AMP-activated protein kinase-dependent regulation of the orphan nuclear receptor SHP". Diabetes. 57 (2): 306–14. doi:10.2337/db07-0381. PMID 17909097.
- ↑ Zhang L, He H, Balschi JA (July 2007). "Metformin and phenformin activate AMP-activated protein kinase in the heart by increasing cytosolic AMP concentration". American Journal of Physiology. Heart and Circulatory Physiology. 293 (1): H457–66. doi:10.1152/ajpheart.00002.2007. PMID 17369473.
- ↑ Miller RA, Chu Q, Xie J, Foretz M, Viollet B, Birnbaum MJ (February 2013). "Biguanides suppress hepatic glucagon signalling by decreasing production of cyclic AMP". Nature. 494 (7436): 256–60. Bibcode:2013Natur.494..256M. doi:10.1038/nature11808. PMC 3573218. PMID 23292513.
- ↑ Collier CA, Bruce CR, Smith AC, Lopaschuk G, Dyck DJ (July 2006). "Metformin counters the insulin-induced suppression of fatty acid oxidation and stimulation of triacylglycerol storage in rodent skeletal muscle". American Journal of Physiology. Endocrinology and Metabolism. 291 (1): E182–9. doi:10.1152/ajpendo.00272.2005. PMID 16478780.
- ↑ Bailey CJ, Turner RC (February 1996). "Metformin". The New England Journal of Medicine. 334 (9): 574–9. doi:10.1056/NEJM199602293340906. PMID 8569826.
- ↑ Fantus IG, Brosseau R (October 1986). "Mechanism of action of metformin: insulin receptor and postreceptor effects in vitro and in vivo". The Journal of Clinical Endocrinology and Metabolism. 63 (4): 898–905. doi:10.1210/jcem-63-4-898. PMID 3745404.
- ↑ Musi N, Hirshman MF, Nygren J, Svanfeldt M, Bavenholm P, Rooyackers O, Zhou G, Williamson JM, Ljunqvist O, Efendic S, Moller DE, Thorell A, Goodyear LJ (July 2002). "Metformin increases AMP-activated protein kinase activity in skeletal muscle of subjects with type 2 diabetes". Diabetes. 51 (7): 2074–81. doi:10.2337/diabetes.51.7.2074. PMID 12086935.
- 1 2 Nikolakis G, Kyrgidis A, Zouboulis CC (2019). "Is There a Role for Antiandrogen Therapy for Hidradenitis Suppurativa? A Systematic Review of Published Data". American Journal of Clinical Dermatology. 20 (4): 503–13. doi:10.1007/s40257-019-00442-w. ISSN 1175-0561. PMID 31073704.
- ↑ Luque-Ramírez M, Nattero-Chávez L, Ortiz Flores AE, Escobar-Morreale HF (March 2018). "Combined oral contraceptives and/or antiandrogens versus insulin sensitizers for polycystic ovary syndrome: a systematic review and meta-analysis". Hum. Reprod. Update. 24 (2): 225–241. doi:10.1093/humupd/dmx039. PMID 29293982.
- ↑ Weersma RK, Zhernakova A, Fu J (May 2020). "Interaction between drugs and the gut microbiome". Gut. doi:10.1136/gutjnl-2019-320204. PMID 32409589.
- ↑ MacNeil LT, Schertzer JD, Steinberg GR (January 2020). "Bacteria transmit metformin-associated lifespan extension". Nat Rev Endocrinol. 16 (1): 9–10. doi:10.1038/s41574-019-0278-3. PMID 31645681.
- ↑ Jones GR, Molloy MP (June 2020). "Metformin, Microbiome and Protection Against Colorectal Cancer". Dig. Dis. Sci. doi:10.1007/s10620-020-06390-4. PMID 32533543.
- 1 2 Heller JB (2007). "Metformin overdose in dogs and cats" (PDF). Veterinary Medicine (April): 231–33. Archived from the original (PDF) on 23 October 2007.
- ↑ Rosilio C, Ben-Sahra I, Bost F, Peyron JF (May 2014). "Metformin: a metabolic disruptor and anti-diabetic drug to target human leukemia". Cancer Letters. 346 (2): 188–96. doi:10.1016/j.canlet.2014.01.006. PMID 24462823.
- 1 2 Pryor R, Cabreiro F (November 2015). "Repurposing metformin: an old drug with new tricks in its binding pockets". The Biochemical Journal. 471 (3): 307–22. doi:10.1042/bj20150497. PMC 4613459. PMID 26475449.
- ↑ Graham GG, Punt J, Arora M, Day RO, Doogue MP, Duong JK, Furlong TJ, Greenfield JR, Greenup LC, Kirkpatrick CM, Ray JE, Timmins P, Williams KM (February 2011). "Clinical pharmacokinetics of metformin". Clinical Pharmacokinetics. 50 (2): 81–98. doi:10.2165/11534750-000000000-00000. PMID 21241070.
- 1 2 Robert F, Fendri S, Hary L, Lacroix C, Andréjak M, Lalau JD (June 2003). "Kinetics of plasma and erythrocyte metformin after acute administration in healthy subjects". Diabetes & Metabolism. 29 (3): 279–83. doi:10.1016/s1262-3636(07)70037-x. PMID 12909816.
- ↑ Tilley, Jefferson; Grimsby, Joseph; Erickson, Shawn; Berthel, Steven (2010). "Diabetes Drugs: Present and Emerging". Burger's Medicinal Chemistry and Drug Discovery. doi:10.1002/0471266949.bmc198. ISBN 978-0471266945.
- 1 2 Werner E, Bell J (1922). "The preparation of methylguanidine, and of ββ-dimethylguanidine by the interaction of dicyandiamide, and methylammonium and dimethylammonium chlorides respectively". J. Chem. Soc., Trans. 121: 1790–95. doi:10.1039/CT9222101790.
- ↑ Shapiro SL, Parrino VA, Freedman L (1959). "Hypoglycemic Agents. I Chemical Properties of β-Phenethylbiguanide. A New Hypoglycemic Agent". J Am Chem Soc. 81 (9): 2220–25. doi:10.1021/ja01518a052.
- ↑ "Procédé de préparation de chlorhydrate de diméthylbiguanide". Patent FR 2322860 (in French). 1975.
{{cite journal}}: CS1 maint: unrecognized language (link) - ↑ Pharmaceutical Manufacturing Encyclopedia (Sittig's Pharmaceutical Manufacturing Encyclopedia). Vol. 3 (3rd ed.). Norwich, NY: William Andrew. 2007. p. 2208. ISBN 978-0-8155-1526-5.
- 1 2 Witters LA (October 2001). "The blooming of the French lilac". The Journal of Clinical Investigation. 108 (8): 1105–7. doi:10.1172/JCI14178. PMC 209536. PMID 11602616.
- ↑ See Chemical Abstracts, v.23, 42772 (1929) Slotta KH, Tschesche R (1929). "Über Biguanide, II.: Die blutzucker-senkende Wirkung der Biguanide". Berichte der Deutschen Chemischen Gesellschaft (A and B Series). 62 (6): 1398–1405. doi:10.1002/cber.19290620605.
- 1 2 Campbell IW, ed. (September 2007). "Metformin – life begins at 50: A symposium held on the occasion of the 43rd Annual Meeting of the European Association for the Study of Diabetes, Amsterdam, The Netherlands, September 2007". The British Journal of Diabetes & Vascular Disease. 7 (5): 247–52. doi:10.1177/14746514070070051001.
- ↑ Dawes GS, Mott JC (March 1950). "Circulatory and respiratory reflexes caused by aromatic guanidines". British Journal of Pharmacology and Chemotherapy. 5 (1): 65–76. doi:10.1111/j.1476-5381.1950.tb00578.x. PMC 1509951. PMID 15405470.
- ↑ About Eusebio Y. Garcia, see: Carteciano J (2005). "Search for DOST-NRCP Dr. Eusebio Y. Garcia Award". Philippines Department of Science and Technology. Archived from the original on 24 October 2009. Retrieved 5 December 2009.
- ↑ Quoted from Chemical Abstracts, v.45, 24828 (1951) Garcia EY (1950). "Fluamine, a new synthetic analgesic and antiflu drug". J Philippine Med Assoc. 26 (7): 287–93. PMID 14779282.
- ↑ About Janusz Supniewski, see: Wołkow PP, Korbut R (April 2006). "Pharmacology at the Jagiellonian University in Kracow, short review of contribution to global science and cardiovascular research through 400 years of history" (PDF). Journal of Physiology and Pharmacology. 57 Suppl 1: 119–36. PMID 16766803. Archived from the original (PDF) on 24 October 2009. Retrieved 22 December 2009.
- ↑ See Chemical Abstracts, v. 52, 22272 (1958) Supniewski J, Chrusciel T (1954). "[N-dimethyl-di-guanide and its biological properties]". Archivum Immunologiae et Therapiae Experimentalis (in Polish). 2: 1–15. PMID 13269290.
{{cite journal}}: CS1 maint: unrecognized language (link) - ↑ Quoted from Chemical Abstracts, v.49, 74699 (1955) Supniewski J, Krupinska J (1954). "[Effect of biguanide derivatives on experimental cowpox in rabbits]". Bulletin de l'Academie Polonaise des Sciences, Classe 3: Mathematique, Astronomie, Physique, Chimie, Geologie et Geographie (in French). 2(Classe II): 161–65.
{{cite journal}}: CS1 maint: unrecognized language (link) - 1 2 3 Bailey CJ, Day C (2004). "Metformin: its botanical background". Practical Diabetes International. 21 (3): 115–17. doi:10.1002/pdi.606. Archived from the original on 17 December 2012.
- ↑ Hadden DR (October 2005). "Goat's rue—French lilac—Italian fitch—Spanish sainfoin: gallega officinalis and metformin: the Edinburgh connection" (PDF). The Journal of the Royal College of Physicians of Edinburgh. 35 (3): 258–60. PMID 16402501. Archived (PDF) from the original on 25 October 2020. Retrieved 2 August 2020.
- ↑ Lucis OJ (January 1983). "The status of metformin in Canada". Canadian Medical Association Journal. 128 (1): 24–6. PMC 1874707. PMID 6847752.
- ↑ "FDA Approves New Diabetes Drug" (Press release). U.S. Food and Drug Administration (FDA). 30 December 1994. Archived from the original on 29 September 2007. Retrieved 6 January 2007.
- ↑ "Drug Approval Package: Glucophage (metformin)" (PDF). U.S. Food and Drug Administration (FDA). Archived (PDF) from the original on 5 February 2020. Retrieved 8 January 2007.
- ↑ Posselt M, Jaeger A, Schaper JL, Radke M, Benskin JP (December 2018). "Determination of polar organic micropollutants in surface and pore water by high-resolution sampling-direct injection-ultra high performance liquid chromatography-tandem mass spectrometry". Environ. Sci.: Process. Impacts. 20 (12): 1716–1727. doi:10.1039/C8EM00390D. PMID 30350841.
- 1 2 Christofides, Elena A. (July 2019). "Practical Insights Into Improving Adherence to Metformin Therapy in Patients With Type 2 Diabetes". Clinical Diabetes : A Publication of the American Diabetes Association. 37 (3): 234–241. doi:10.2337/cd18-0063. ISSN 0891-8929. PMC 6640881. PMID 31371854. Archived from the original on 29 August 2021. Retrieved 2 August 2020.
- 1 2 Dharam, Kaushik; Jeffrey Karnes, R.; Eisenberg, Manuel S.; Rangel, Laureano J.; Carlson, Rachel E.; Bergstralh, Eric J. (January 2014). "Impact Of Metformin On Prostate Cancer Outcomes After Radical Prostatectomy". Urologic oncology. 32 (1): 43.e1–43.e7. doi:10.1016/j.urolonc.2013.05.005. ISSN 1078-1439. PMC 4006350. PMID 23810664. Archived from the original on 28 August 2021. Retrieved 2 August 2020.
Metformin use at time of RP was extracted from the Mayo Clinic electronic medical record (EMR) by searching in the 3 months prior to the RP for the terms- metformin, Glucophage®, Glumetza®, Riomet®, Fortamet®, Obimet®, Gluformin®, Dianben®, Diabex®, Diaformin® or Metsol®.
- 1 2 3 "Metformin". Drugs.com. Archived from the original on 28 November 2020. Retrieved 17 July 2020.
- ↑ Bailey CJ, Day C (June 2009). "Fixed-dose single tablet antidiabetic combinations". Diabetes, Obesity & Metabolism. 11 (6): 527–33. doi:10.1111/j.1463-1326.2008.00993.x. PMID 19175373.
- ↑ Sheehan, Michael T. (July 2003). "Current Therapeutic Options in Type 2 Diabetes Mellitus: A Practical Approach". Clinical Medicine and Research. 1 (3): 189–200. ISSN 1539-4182. PMC 1069045. PMID 15931309. Archived from the original on 28 August 2021. Retrieved 2 August 2020.
- ↑ "FDA Approves GlaxoSmithKline's Avandamet (rosiglitazone maleate and metformin HCl), The Latest Advancement in the Treatment of Type 2 Diabetes" (Press release). GlaxoSmithKline. 12 October 2002. Archived from the original on 21 January 2007. Retrieved 27 December 2006.
- ↑ "Drugs@FDA: FDA-Approved Drugs". www.accessdata.fda.gov. Archived from the original on 21 March 2021. Retrieved 21 July 2020.
- ↑ "2009 Top 200 branded drugs by total prescriptions" (PDF). Archived from the original (PDF) on 14 July 2011. (96.5 KB). Drug Topics (17 June 2010). Retrieved 2 September 2010.
- ↑ "Questions and Answers about the Seizure of Paxil CR and Avandamet" (Press release). U.S. Food and Drug Administration. 4 March 2005. Archived from the original on 14 October 2007. Retrieved 27 December 2006.
- ↑ "Teva Pharm announces settlement of generic Avandia, Avandamet, and Avandaryl litigation with GlaxoSmithKline" (Press release). Reuters. 27 September 2007. Archived from the original on 3 May 2021. Retrieved 17 February 2009.
- ↑ Nissen SE, Wolski K (June 2007). "Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes". The New England Journal of Medicine. 356 (24): 2457–71. doi:10.1056/NEJMoa072761. PMID 17517853.
- ↑ "European Medicines Agency recommends suspension of Avandia, Avandamet and Avaglim". News and Events. European Medicines Agency. 17 September 2018. Archived from the original on 24 September 2015.
- ↑ "Call to 'suspend' diabetes drug". BBC News. 23 September 2010. Archived from the original on 24 September 2010.
- ↑ "Drugs banned in India". Central Drugs Standard Control Organization, Dte.GHS, Ministry of Health and Family Welfare, Government of India. Archived from the original on 21 February 2015. Retrieved 17 September 2013.
- ↑ "Diabetes drug withdrawn". Stuff.co.nz. NZPA. 17 February 2011. Archived from the original on 13 October 2013. Retrieved 5 November 2011.
- ↑ Harris, Gardiner (19 February 2010). "Controversial Diabetes Drug Harms Heart, U.S. Concludes". The New York Times. Archived from the original on 19 March 2017.
- ↑ "Most Popular E-mail Newsletter". USA Today. 24 May 2011. Archived from the original on 20 July 2018. Retrieved 2 August 2020.
- ↑ "Glaxo's Avandia Cleared From Sales Restrictions by FDA". Bloomberg. Archived from the original on 9 November 2014.
- ↑ "FDA requires removal of certain restrictions on the diabetes drug Avandia". U.S. Food and Drug Administration (FDA) (Press release). 25 November 2013. Archived from the original on 4 May 2015.
- ↑ "US agency reverses stance on controversial diabetes drug". Archived from the original on 11 December 2015.
- ↑ "Glubrava EPAR". European Medicines Agency (EMA). Archived from the original on 9 June 2021. Retrieved 31 March 2020.
- ↑ "Competact EPAR". European Medicines Agency (EMA). Archived from the original on 9 June 2021. Retrieved 31 March 2020.
- ↑ "Pioglitazone (marketed as Actos, Actoplus Met, Duetact, and Oseni) Information". U.S. Food and Drug Administration (FDA). 11 January 2017. Archived from the original on 17 January 2021. Retrieved 31 March 2020.
- ↑ "FDA Drug Safety Communication: FDA revises warnings regarding use of the diabetes medicine metformin in certain patients with reduced kidney function". U.S. Food and Drug Administration (FDA). 3 April 2013. Archived from the original on 25 May 2021. Retrieved 31 March 2020.
- ↑ "FDA Drug Safety Communication: Updated FDA review concludes that use of type 2 diabetes medicine pioglitazone may be linked to an increased risk of bladder cancer". U.S. Food and Drug Administration (FDA). 4 August 2011. Archived from the original on 26 January 2021. Retrieved 31 March 2020.
- ↑ "Janumet- sitagliptin and metformin hydrochloride tablet, film coated". DailyMed. 12 August 2019. Archived from the original on 9 June 2021. Retrieved 15 May 2020.
- ↑ "Janumet EPAR". European Medicines Agency (EMA). Archived from the original on 9 June 2021. Retrieved 15 May 2020.
- ↑ "Kombiglyze XR- saxagliptin and metformin hydrochloride tablet, film coated, extended release". DailyMed. 24 October 2019. Archived from the original on 25 September 2020. Retrieved 15 May 2020.
- ↑ "Komboglyze EPAR". European Medicines Agency (EMA). Archived from the original on 30 October 2020. Retrieved 15 May 2020.
- ↑ "Kazano- alogliptin and metformin hydrochloride tablet, film coated". DailyMed. 14 June 2019. Archived from the original on 9 June 2021. Retrieved 15 May 2020.
- ↑ "Vipdomet EPAR". European Medicines Agency (EMA). Archived from the original on 9 June 2021. Retrieved 15 May 2020.
- ↑ "Jentadueto EPAR". European Medicines Agency (EMA). 17 September 2018. Archived from the original on 9 June 2021. Retrieved 31 March 2020.
- ↑ "Jentadueto- linagliptin and metformin hydrochloride tablet, film coated". DailyMed. 18 July 2019. Archived from the original on 9 June 2021. Retrieved 31 March 2020.
- 1 2 Grant, Joan S.; Graven, Lucinda J. (11 July 2016). "Progressing From Metformin to Sulfonylureas or Meglitinides". Workplace Health & Safety. 64 (9): 433–439. doi:10.1177/2165079916644263. ISSN 2165-0799. Archived from the original on 28 August 2021. Retrieved 2 August 2020.
- ↑ "The Use of Medicines in the United States: Review of 2010" (PDF). Archived (PDF) from the original on 22 April 2011. (1.79 MB). IMS Institute for Healthcare Informatics (April 2011). Retrieved 28 April 2011.
- ↑ "Drug Approval Package: PrandiMet (repaglinide/metformin HCI fixed-dose combination) NDA 22386". www.accessdata.fda.gov. Archived from the original on 21 July 2020. Retrieved 21 July 2020.
- ↑ "Drugs@FDA: FDA-Approved Drugs". www.accessdata.fda.gov. Archived from the original on 22 July 2020. Retrieved 21 July 2020.
- ↑ "Drugs@FDA: FDA-Approved Drugs". www.accessdata.fda.gov. Archived from the original on 22 March 2021. Retrieved 21 July 2020.
- ↑ Panikar V, Chandalia HB, Joshi SR, Fafadia A, Santvana C (November 2003). "Beneficial effects of triple drug combination of pioglitazone with glibenclamide and metformin in type 2 diabetes mellitus patients on insulin therapy". The Journal of the Association of Physicians of India. 51: 1061–4. PMID 15260389.
- ↑ "Statement from Janet Woodcock, M.D., director of FDA's Center for Drug Evaluation and Research, on impurities found in diabetes drugs outside the U.S." U.S. Food and Drug Administration (FDA). 5 December 2019. Archived from the original on 18 January 2021. Retrieved 4 February 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ "Recalls and safety alerts". Health Canada evaluating NDMA in metformin drugs. 5 December 2019. Archived from the original on 17 April 2020. Retrieved 4 February 2020.
- ↑ "Laboratory Tests - Metformin". U.S. Food and Drug Administration (FDA). 3 February 2020. Archived from the original on 25 February 2020. Retrieved 4 February 2020.
- ↑ "FDA Updates and Press Announcements on NDMA in Metformin". U.S. Food and Drug Administration (FDA). 4 February 2020. Archived from the original on 25 February 2020. Retrieved 4 February 2020.
- ↑ "APO-Metformin (2020-02-04)". Health Canada. 4 February 2020. Archived from the original on 27 December 2020. Retrieved 2 June 2020.
- ↑ "Ranbaxy Metformin Product Recall (2020-02-26)". Health Canada. 26 February 2020. Archived from the original on 26 November 2020. Retrieved 2 June 2020.
- ↑ "Jamp-Metformin Product Recall (2020-03-10)". Health Canada. 10 March 2020. Archived from the original on 26 November 2020. Retrieved 2 June 2020.
- ↑ "FDA Alerts Patients and Health Care Professionals to Nitrosamine Impurity Findings in Certain Metformin Extended-Release Products" (Press release). U.S. Food and Drug Administration (FDA). 28 May 2020. Archived from the original on 22 March 2021. Retrieved 2 June 2020.
- ↑ "Questions and Answers: NDMA impurities in metformin products". U.S. Food and Drug Administration (FDA). 28 May 2020. Archived from the original on 2 March 2021. Retrieved 5 June 2020.
- ↑ "Amneal Pharmaceuticals LLC Issues Voluntary Nationwide Recall of Metformin Hydrochloride Extended Release Tablets, USP, 500 mg and 750 mg, Due to Detection of N-Nitrosodimethylamine (NDMA) Impurity". U.S. Food and Drug Administration (FDA). 29 May 2020. Archived from the original on 16 January 2021. Retrieved 2 June 2020.
- ↑ "Apotex Corp. Issues Voluntary Nationwide Recall of Metformin Hydrochloride Extended-Release Tablets 500mg Due to the Detection of N-nitrosodimethylamine (NDMA)". U.S. Food and Drug Administration (FDA). 27 May 2020. Archived from the original on 4 March 2021. Retrieved 2 June 2020.
- ↑ "Teva Pharmaceuticals USA, Inc. Initiates Voluntary Nationwide Recall of Metformin Hydrochloride Extended-Release Tablets USP 500 mg and 750 mg Due to Detection of N-Nitrosodimethylamine (NDMA)". U.S. Food and Drug Administration (FDA). 2 June 2020. Archived from the original on 21 January 2021. Retrieved 5 June 2020.
- ↑ "Marksans Pharma Limited Issues Voluntary Nationwide Recall of Metformin Hydrochloride Extended-Release Tablets, USP 500mg, Due to the Detection of N-Nitrosodimethylamine (NDMA)". U.S. Food and Drug Administration (FDA). 2 June 2020. Archived from the original on 23 January 2021. Retrieved 5 June 2020.
- ↑ Cavazzoni, Patrizia (28 May 2020). "Re: Docket No. FDA-2020-P-0978" (PDF). U.S. Food and Drug Administration (FDA). Archived (PDF) from the original on 8 February 2021. Retrieved 2 June 2020.
- 1 2 3 "Laboratory Tests - Metformin". U.S. Food and Drug Administration (FDA). 5 June 2020. Archived from the original on 22 April 2021. Retrieved 5 June 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ Inc, Lupin Pharmaceuticals. "Lupin Pharmaceuticals, Inc. Issues Voluntarily Nationwide Recall of Metformin Hydrochloride Extended-Release Tablets, 500mg and 1000mg Due to the Detection of N-Nitrosodimethylamine (NDMA) Impurity". www.prnewswire.com. Archived from the original on 9 June 2021. Retrieved 9 July 2020.
- ↑ Marchesini G, Brizi M, Bianchi G, Tomassetti S, Zoli M, Melchionda N (September 2001). "Metformin in non-alcoholic steatohepatitis". Lancet. 358 (9285): 893–4. doi:10.1016/S0140-6736(01)06042-1. PMID 11567710.
- ↑ Socha P, Horvath A, Vajro P, Dziechciarz P, Dhawan A, Szajewska H (May 2009). "Pharmacological interventions for nonalcoholic fatty liver disease in adults and in children: a systematic review". Journal of Pediatric Gastroenterology and Nutrition. 48 (5): 587–96. doi:10.1097/MPG.0b013e31818e04d1. PMID 19412008.
- 1 2 Angelico F, Burattin M, Alessandri C, Del Ben M, Lirussi F (January 2007). Angelico F (ed.). "Drugs improving insulin resistance for non-alcoholic fatty liver disease and/or non-alcoholic steatohepatitis". Cochrane Database of Systematic Reviews. 24 (1): CD005166. doi:10.1002/14651858.CD005166.pub2. PMID 17253544. (Retracted, see doi:10.1002/14651858.cd005166.pub3. If this is an intentional citation to a retracted paper, please replace
{{Retracted}}with{{Retracted|intentional=yes}}.) - ↑ Ibáñez L, Ong K, Valls C, Marcos MV, Dunger DB, de Zegher F (August 2006). "Metformin treatment to prevent early puberty in girls with precocious pubarche". The Journal of Clinical Endocrinology and Metabolism. 91 (8): 2888–91. doi:10.1210/jc.2006-0336. PMID 16684823.
- ↑ Ben Sahra I, Le Marchand-Brustel Y, Tanti JF, Bost F (May 2010). "Metformin in cancer therapy: a new perspective for an old antidiabetic drug?". Molecular Cancer Therapeutics. 9 (5): 1092–9. doi:10.1158/1535-7163.MCT-09-1186. PMID 20442309.
- ↑ Malek M, Aghili R, Emami Z, Khamseh ME (September 2013). "Risk of cancer in diabetes: the effect of metformin". ISRN Endocrinology. 2013: 636927. doi:10.1155/2013/636927. PMC 3800579. PMID 24224094.
- 1 2 Campbell JM, Bellman SM, Stephenson MD, Lisy K (November 2017). "Metformin reduces all-cause mortality and diseases of ageing independent of its effect on diabetes control: A systematic review and meta-analysis". Ageing Research Reviews. 40: 31–44. doi:10.1016/j.arr.2017.08.003. PMID 28802803.
- ↑ Gantois I, Popic J, Khoutorsky A, et al. (January 2019). "Metformin for Treatment of Fragile X Syndrome and Other Neurological Disorders". Annu. Rev. Med. 70: 167–181. doi:10.1146/annurev-med-081117-041238. PMID 30365357.
- ↑ Barzilai N, Crandall JP, Kritchevsky SB, et al. (June 2016). "Metformin as a Tool to Target Aging". Cell Metabolism. 23 (6): 1060–5. doi:10.1016/j.cmet.2016.05.011. PMC 5943638. PMID 27304507.
Further reading
- Markowicz-Piasecka M, Huttunen KM, Mateusiak L, et al. (2017). "Is Metformin a Perfect Drug? Updates in Pharmacokinetics and Pharmacodynamics". Curr. Pharm. Des. 23 (17): 2532–2550. doi:10.2174/1381612822666161201152941. PMID 27908266.
- McCreight LJ, Bailey CJ, Pearson ER (March 2016). "Metformin and the gastrointestinal tract". Diabetologia. 59 (3): 426–35. doi:10.1007/s00125-015-3844-9. PMC 4742508. PMID 26780750.
- Moin T, Schmittdiel JA, Flory JH, et al. (October 2018). "Review of Metformin Use for Type 2 Diabetes Prevention". Am J Prev Med. 55 (4): 565–574. doi:10.1016/j.amepre.2018.04.038. PMC 6613947. PMID 30126667.
- Rena G, Hardie DG, Pearson ER (September 2017). "The mechanisms of action of metformin". Diabetologia. 60 (9): 1577–1585. doi:10.1007/s00125-017-4342-z. PMC 5552828. PMID 28776086.
- Sanchez-Rangel E, Inzucchi SE (September 2017). "Metformin: clinical use in type 2 diabetes". Diabetologia. 60 (9): 1586–1593. doi:10.1007/s00125-017-4336-x. PMID 28770321.
- Zhou J, Massey S, Story D, et al. (September 2018). "Metformin: An Old Drug with New Applications". Int J Mol Sci. 19 (10): 2863. doi:10.3390/ijms19102863. PMC 6213209. PMID 30241400.
- Zhou T, Xu X, Du M, et al. (October 2018). "A preclinical overview of metformin for the treatment of type 2 diabetes". Biomed. Pharmacother. 106: 1227–1235. doi:10.1016/j.biopha.2018.07.085. PMID 30119191.
External links
| External sites: |
|
|---|---|
| Identifiers: |