Mucosal immunology

Mucosal immunology is the study of immune system responses that occur at mucosal membranes of the intestines, the urogenital tract, and the respiratory system.[1] The mucous membranes are in constant contact with a large number of microorganisms, food, and inhaled air antigens.[2] In healthy states, the mucosal immune system protects the organism against infectious pathogens but also maintains a tolerance towards non-harmful commensal microbes and benign environmental substances.[1] Disruption of this balance between tolerance and deprivation of pathogens can lead to various pathological conditions such as food allergies, irritable bowel syndrome, susceptibility to infections, and more.[2]
The mucosal immune system consists of a cellular component, humoral immunity, and defense mechanisms that prevent the invasion of microorganisms and harmful foreign substances into the body. These defense mechanisms can be divided into physical barriers (epithelial lining, mucus, cilia function, intestinal peristalsis, etc.) and chemical factors (pH, antimicrobial peptides, etc.).[3]
The integrity of the mucosal barrier is very important for the proper functioning of the immune system on the mucous membranes.[4] Barrier function is determined by several factors such as the age of the individual, genetics, types of mucins present on the mucosa, interactions between mast cells, nerves and neuropeptides, co-infection, etc. The integrity of barriers also depends on the immunosuppressive mechanisms implemented on the mucosa.[3] The mucosal barrier is formed due to the tight junctions between the epithelial cells of the mucosa and the presence of the mucus on the surface of these epithelial cells.[4] The mucins that form mucus not only offer protection from components on the mucosa by static shielding but also limit the immunogenicity of intestinal antigens by inducing an anti-inflammatory state in dendritic cells (DC).[5]
Because the mucosa surfaces are in constant contact with external antigens and microbiota there is a need for a large number of immune cells. For example, approximately 3/4 of all lymphocytes in the body are found in the mucous membranes. These immune cells reside in secondary lymphoid tissue, largely distributed through the mucosal surfaces.[3]
The mucosa-associated lymphoid tissue, or MALT, provides the organism with an important first line of defense. Along with the spleen and lymph nodes, the tonsils and MALT are also considered to be secondary lymphoid tissue.[6]
The cellular component found in the MALT is composed mostly of dendritic cells, macrophages, innate lymphoid cells, mucosal-associated invariant T cells, intraepithelial T cells, regulatory T cells (Treg), and IgA secreting plasma cells.[1][3][7]
Intraepithelial T cells, usually CD8+, reside between mucosal epithelial cells. These cells do not need primary activation like classic T cells. Instead upon recognition of antigen, these cells initiate their effector functions, resulting in faster removal of pathogens.[7] Tregs are very abundant on the mucous membranes and play a very important role in maintaining tolerance through various functions, especially through the production of anti-inflammatory cytokines.[8] Mucosal resident antigen-presenting cells (APCs) in healthy people show a tolerogenic phenotype.[9] These APCs do not express TLR2 or TLR4 on their surfaces. In addition, only negligible levels of the LPS receptor CD14 are normally present on these cells.[9] Mucosal dendritic cells determine the type of subsequent immune responses by the production of certain types of cytokines and the type of molecules involved in the co-stimulation.[3] Innate lymphoid cells are abundant in the mucosa where they, due to rapid cytokine production in response to tissue-derived signals, act as regulators of immunity, inflammation, and barrier homeostasis.[10]
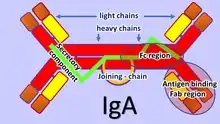
The adaptive mucosal immune system is involved in maintaining mucosal homeostasis through a mechanism of immune exclusion mediated by secretory antibodies (mostly IgA) that inhibit the penetration of invasive pathogens into the body's tissues and prevent the penetration of potentially dangerous exogenous proteins.[11] Another mechanism of adaptive mucosal immunity is the implementation of immunosuppressive mechanisms mediated mainly by Tergs to prevent local and peripheral hypersensitivity to harmless antigens, i.e. oral tolerance.[12]
The mucosal immune system provides three main functions:
- Serving as the body's first line of defense from harmful antigenic structures and infection.[3]
- Preventing systemic immune responses to commensal bacteria and food antigens.[2]
- Regulating appropriate immune responses to pathogens encountered on a daily basis.[2]
Basic immune response in the gut
In the gut, lymphoid tissue is dispersed in gut-associated lymphoid tissue (GALT). A large number of immune system cells in the intestines are found in dome-like structures called Peyer's patches.[13] Above the Peyer's patches is a single layer of epithelial cells, which together with the mucus form a barrier against microbial invasion into the underlying tissue. Antigen sampling is a key function of Peyer's patches. Above the Peyer's patches is a much thinner mucus layer that helps the antigen sampling.[13] Specialized phagocytic cells, called M cells, which are found in the epithelial layer of the Peyer's patches, can transport antigenic material across the intestinal barrier through the process of transcytosis.[14] The material transported in this way from the intestinal lumen can be then presented by the antigen-presenting cells present in the Peyer patches.[13][14] In addition, dendritic cells in Peyer patches can extend their dendrites through M cell specific transcellular pores and they can also capture translocated IgA immune complexes.[15] Dendritic cells then present the antigen to naïve T cells in the local mesenteric lymph nodes.[16]
If mucosal barrier homeostasis has not been violated and invasive pathogens are not present, dendritic cells induce tolerance in the gut due to induction of Tregs by secretion of TGF-β.[16] These Tregs further travel to the lamina propria of villi through lymphatic vessels. Here, Tregs produce IL-10, which affects other immune cells in the lamina propria toward a tolerogenic state.[16]
However, if the homeostasis of the intestinal barrier is disturbed in any way, it leads to inflammation. The epithelium in direct contact with bacteria is activated and begins to produce danger-associated molecular patterns (DAMPs).[16] Alarm molecules released from epithelial cells activate immune cells.[16][17] Dendritic cells and macrophages are activated in this environment and they produce key pro-inflammatory cytokines such as IL-6, IL-12, and IL-23 which further activates more immune cells and direct them toward a pro-inflammatory state.[17] Furthermore, the activated effector cells then produce TNF, IFNγ, and IL-17.[17] Neutrophils are attracted to the affected area and begin to perform their effector functions.[1] After the ongoing infection has been removed, the inflammatory response must be stopped to restore homeostasis.[16] The damaged tissue is healed and everything returns to its natural state of tolerance.[16]
Neonatal mucosal immunology
At birth, the neonate's mucosal immune system is relatively undeveloped and needs the colonization of intestinal flora to promote its development.[6] The composition of the microbiota stabilizes around the age of 3.[2] In the neonatal period and in early childhood interaction of host immunity with the microbiome is critical, during this interaction various arms of immunity are educated, which contribute to the homeostasis of the organism and it also determines the future setting of the immune system, i.e. its susceptibility to infections and inflammatory diseases.[2][3] For example, the B cell line in the intestinal mucosa is regulated by extracellular signals from commensal microbes that affect the intestinal immunoglobulin repertoire.[18] A high diversity of microbiota in early childhood protects the body from the induction of mucosal IgE, which is associated with allergy development.[19]
Mucosal vaccines
Because of its front-line status within the immune system, the mucosal immune system is being investigated for use in vaccines for various afflictions,[20] including HIV[21] and allergies.[20]
See also
References
- 1 2 3 4 "Mucosal immunology - Latest research and news". www.nature.com. Retrieved 2016-11-08.
- 1 2 3 4 5 6 Zheng, Danping; Liwinski, Timur; Elinav, Eran (June 2020). "Interaction between microbiota and immunity in health and disease". Cell Research. 30 (6): 492–506. doi:10.1038/s41422-020-0332-7. ISSN 1001-0602. PMC 7264227. PMID 32433595.
- 1 2 3 4 5 6 7 Brandtzaeg, Per (2009), Brandtzaeg, P.; Isolauri, E.; Prescott, S.L. (eds.), "'ABC' of Mucosal Immunology", Nestle Nutrition Workshop Series. Paediatric Programme, Nestlé Nutrition Institute Workshop Series: Pediatric Program, Basel: KARGER, 64: 23–43, doi:10.1159/000235781, ISBN 978-3-8055-9167-6, PMID 19710513, retrieved 2022-01-13
- 1 2 Okumura, Ryu; Takeda, Kiyoshi (December 2018). "Maintenance of intestinal homeostasis by mucosal barriers". Inflammation and Regeneration. 38 (1): 5. doi:10.1186/s41232-018-0063-z. ISSN 1880-8190. PMC 5879757. PMID 29619131.
- ↑ Shan, Meimei; Gentile, Maurizio; Yeiser, John R.; Walland, A. Cooper; Bornstein, Victor U.; Chen, Kang; He, Bing; Cassis, Linda; Bigas, Anna; Cols, Montserrat; Comerma, Laura (2013-10-25). "Mucus Enhances Gut Homeostasis and Oral Tolerance by Delivering Immunoregulatory Signals". Science. 342 (6157): 447–453. Bibcode:2013Sci...342..447S. doi:10.1126/science.1237910. ISSN 0036-8075. PMC 4005805. PMID 24072822.
- 1 2 Torow, N; Marsland, B J; Hornef, M W; Gollwitzer, E S (January 2017). "Neonatal mucosal immunology". Mucosal Immunology. 10 (1): 5–17. doi:10.1038/mi.2016.81. ISSN 1933-0219. PMID 27649929. S2CID 3556125.
- 1 2 Olivares-Villagómez, Danyvid; Van Kaer, Luc (April 2018). "Intestinal Intraepithelial Lymphocytes: Sentinels of the Mucosal Barrier". Trends in Immunology. 39 (4): 264–275. doi:10.1016/j.it.2017.11.003. PMC 8056148. PMID 29221933.
- ↑ Richert-Spuhler, Laura E.; Lund, Jennifer M. (2015), "The Immune Fulcrum", Progress in Molecular Biology and Translational Science, Elsevier, 136: 217–243, doi:10.1016/bs.pmbts.2015.07.015, ISBN 978-0-12-803415-6, PMC 4769439, PMID 26615099
- 1 2 Koenig, J. E.; Spor, A.; Scalfone, N.; Fricker, A. D.; Stombaugh, J.; Knight, R.; Angenent, L. T.; Ley, R. E. (2011-03-15). "Succession of microbial consortia in the developing infant gut microbiome". Proceedings of the National Academy of Sciences. 108 (Supplement_1): 4578–4585. Bibcode:2011PNAS..108.4578K. doi:10.1073/pnas.1000081107. ISSN 0027-8424. PMC 3063592. PMID 20668239.
- ↑ Sonnenberg, Gregory F.; Hepworth, Matthew R. (October 2019). "Functional interactions between innate lymphoid cells and adaptive immunity". Nature Reviews Immunology. 19 (10): 599–613. doi:10.1038/s41577-019-0194-8. ISSN 1474-1733. PMC 6982279. PMID 31350531.
- ↑ Chen, Kang; Magri, Giuliana; Grasset, Emilie K.; Cerutti, Andrea (July 2020). "Rethinking mucosal antibody responses: IgM, IgG and IgD join IgA". Nature Reviews Immunology. 20 (7): 427–441. doi:10.1038/s41577-019-0261-1. ISSN 1474-1733. PMID 32015473. S2CID 211017339.
- ↑ Traxinger, Brianna R.; Richert-Spuhler, Laura E.; Lund, Jennifer M. (2021-11-29). "Mucosal tissue regulatory T cells are integral in balancing immunity and tolerance at portals of antigen entry". Mucosal Immunology: 1–10. doi:10.1038/s41385-021-00471-x. ISSN 1933-0219. PMC 8628059. PMID 34845322.
- 1 2 3 Mörbe, Urs M.; Jørgensen, Peter B.; Fenton, Thomas M.; von Burg, Nicole; Riis, Lene B.; Spencer, Jo; Agace, William W. (July 2021). "Human gut-associated lymphoid tissues (GALT); diversity, structure, and function". Mucosal Immunology. 14 (4): 793–802. doi:10.1038/s41385-021-00389-4. ISSN 1933-0219. PMID 33753873. S2CID 232322692.
- 1 2 Dillon, Andrea; Lo, David D. (2019-07-02). "M Cells: Intelligent Engineering of Mucosal Immune Surveillance". Frontiers in Immunology. 10: 1499. doi:10.3389/fimmu.2019.01499. ISSN 1664-3224. PMC 6614372. PMID 31312204.
- ↑ Stagg, Andrew J. (2018-12-06). "Intestinal Dendritic Cells in Health and Gut Inflammation". Frontiers in Immunology. 9: 2883. doi:10.3389/fimmu.2018.02883. ISSN 1664-3224. PMC 6291504. PMID 30574151.
- 1 2 3 4 5 6 7 Tordesillas, Leticia; Berin, M. Cecilia (October 2018). "Mechanisms of Oral Tolerance". Clinical Reviews in Allergy & Immunology. 55 (2): 107–117. doi:10.1007/s12016-018-8680-5. ISSN 1080-0549. PMC 6110983. PMID 29488131.
- 1 2 3 Chistiakov, Dimitry A.; Bobryshev, Yuri V.; Kozarov, Emil; Sobenin, Igor A.; Orekhov, Alexander N. (2015-01-13). "Intestinal mucosal tolerance and impact of gut microbiota to mucosal tolerance". Frontiers in Microbiology. 5: 781. doi:10.3389/fmicb.2014.00781. ISSN 1664-302X. PMC 4292724. PMID 25628617.
- ↑ Wesemann, Duane R.; Portuguese, Andrew J.; Meyers, Robin M.; Gallagher, Michael P.; Cluff-Jones, Kendra; Magee, Jennifer M.; Panchakshari, Rohit A.; Rodig, Scott J.; Kepler, Thomas B.; Alt, Frederick W. (September 2013). "Microbial colonization influences early B-lineage development in the gut lamina propria". Nature. 501 (7465): 112–115. Bibcode:2013Natur.501..112W. doi:10.1038/nature12496. ISSN 0028-0836. PMC 3807868. PMID 23965619.
- ↑ The Integrative HMP (iHMP) Research Network Consortium (May 2019). "The Integrative Human Microbiome Project". Nature. 569 (7758): 641–648. Bibcode:2019Natur.569..641I. doi:10.1038/s41586-019-1238-8. ISSN 0028-0836. PMC 6784865. PMID 31142853.
- 1 2 Wild, C.; Wallner, M.; Hufnagl, K.; Fuchs, H.; Hoffmann-Sommergruber, K.; Breiteneder, H.; Scheiner, O.; Ferreira, F.; Wiedermann, U. (January 2007). "A recombinant allergen chimer as novel mucosal vaccine candidate for prevention of multi-sensitivities". Allergy. 62 (1): 33–41. doi:10.1111/j.1398-9995.2006.01245.x. ISSN 0105-4538. PMID 17156339. S2CID 9883901.
- ↑ Kozlowski, Pamela A.; Aldovini, Anna (2019-04-12). "Mucosal Vaccine Approaches for Prevention of HIV and SIV Transmission". Current Immunology Reviews. 15 (1): 102–122. doi:10.2174/1573395514666180605092054. PMC 6709706. PMID 31452652.
Works cited
- Helbert, Matthew (2016-06-17). Immunology for Medical Students. Elsevier. ISBN 978-0-7020-6801-0.