Sacubitril/valsartan
 | |
| Combination of | |
|---|---|
| Sacubitril | Neprilysin inhibitor |
| Valsartan | Angiotensin II receptor antagonist |
| Names | |
| Trade names | Entresto, Azmarda, Neparvis, others |
| Other names | LCZ696 |
| Clinical data | |
| Drug class | Angiotensin receptor-neprilysin inhibitor (ARNi)[1] |
| Main uses | Heart failure[2] |
| Side effects | Low blood pressure, cough, kidney problems, high potassium, angioedema[1] |
| Pregnancy category | |
| Routes of use | By mouth |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a615039 |
| Legal | |
| License data | |
| Legal status | |
| Chemical and physical data | |
| Formula | C96H120N12Na6O21 |
| Molar mass | 1916.018 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Sacubitril/valsartan, sold under the brand name Entresto among others, is a combination medication used for heart failure with reduced ejection fraction.[2] It may be used to replace an ACE inhibitor or an angiotensin receptor blocker.[2] It is taken by mouth.[2]
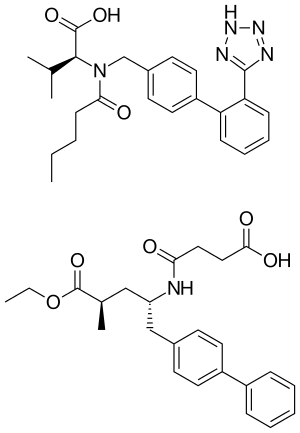
Common side effects include low blood pressure, cough, kidney problems, and high potassium.[1] Other side effects may include angioedema.[1] Use in pregnancy may harm the baby.[1] It contains sacubitril, a neprilysin inhibitor, and valsartan, a angiotensin receptor blocker.[1] The combination is sometimes known as an "angiotensin receptor-neprilysin inhibitor" (ARNi).[1]
Sacubitril/valsartan was approved for medical use in the United States and Europe in 2015.[7][1] It was approved in Australia in 2016.[3] In the United States it costs about 575 USD per month as of 2021.[9] This amount in the United Kingdom costs the NHS about £92.[2]
Medical uses
Reduced ejection fraction
Sacubitril/valsartan can be used instead of an ACE inhibitor or an angiotensin receptor blocker alone in people with heart failure and a reduced left ventricular ejection fraction (LVEF),[10][11] alongside other standard therapies (e.g. beta-blockers) for heart failure.[12][13][14]
People who exhibit symptoms of NYHA Class II or III heart failure and are still symptomatic despite maximally tolerated dose of an ACE inhibitor or ARB alone, may be considered for sacubitril/valsartan dual therapy to decrease the risk of cardiovascular-related and all-cause mortality.[15] Mortality benefits have only been observed to date in those with LVEF less than 35%.[16][15] Changing 100 people from an ACE inhibitor or angiotensin II receptor antagonist to sacubitril/valsartan for 2.3 years would prevent three deaths, five hospitalizations for heart failure, and eleven hospitalizations overall.[14]
Normal ejection fraction
In those with heart failure with a preserved LVEF (HFpEF), a LVEF of 45% or more, it failed to reduce hospitalisation related to heart failure or reducing death from cardiovascular causes.[16] A Cochrane review of us in HFpEF found evidence is also lacking to support use of ACE Inhibitors, ARBs or ARNIs in people with HFpEF, and that the mainstay medication for HFpEF still remains the treatment of co-morbidities such as high blood pressure or other triggers for decompensation.[17]
Dosage
It is generally started at 24/26 mg twice per day and may be increased up to 97/103 mg twice per day.[2]
Side effects
Common side effects [>1%] include hyperkalaemia [high potassium levels in the blood, a known side effect of Valsartan], hypotension [low blood pressure, common in vasodilators and extracellular fluid volume reducers], a persistent dry cough and renal impairment [reduced kidney function].[15][16][18]
Angioedema, a rare but more serious reaction, can occur in some patients [<1%] and involves swelling of the face and lips.[15][16][18] Angioedema is more common in black patients.[15] Sacubitril/Valsartan should not be taken within 36 hours of an Angiotensin Converting Enzyme Inhibitor to reduce the risk of developing Angioedema.[15]
The side effect profile in trials of sacubitril/valsartan compared to valsartan alone or enalapril [an angiotensin converting enzyme inhibitor] is very similar, with the incidence of hypotension slightly higher in sacubitril/valsartan, the risk comparable for angioedema, and the chance of hyperkalaemia, renal impairment and cough slightly lower.[15][16][18]
Sacubitril/valsartan is contraindicated in pregnancy because it contains valsartan, a known risk for birth defects.[6]
Pharmacology
Valsartan blocks the angiotensin II receptor type 1 (AT1). This receptor is found on both vascular smooth muscle cells, and on the zona glomerulosa cells of the adrenal gland which are responsible for aldosterone secretion. In the absence of AT1 blockade, angiotensin causes both direct vasoconstriction and adrenal aldosterone secretion, the aldosterone then acting on the distal tubular cells of the kidney to promote sodium reabsorption which expands extracellular fluid (ECF) volume. Blockade of (AT1) thus causes blood vessel dilation and reduction of ECF volume.[19][20]
Sacubitril is a prodrug that is activated to sacubitrilat (LBQ657) by de-ethylation via esterases.[21] Sacubitrilat inhibits the enzyme neprilysin,[22] a neutral endopeptidase that degrades vasoactive peptides, including natriuretic peptides, bradykinin, and adrenomedullin. Thus, sacubitril increases the levels of these peptides, causing blood vessel dilation and reduction of ECF volume via sodium excretion.[23]
Despite these actions, neprilysin inhibitors have been found to have limited efficacy in the treatment of hypertension and heart failure when taken on their own.[24][25] This is attributed to a reduction in enzymatic breakdown of angiotensin II by the reduction of neprilysin activity, which results in an increase in systemic angiotensin II levels and the negation of the positive effects of this drug family in cardiovascular disease treatment.[25] Combined treatment with a neprilysin inhibitor and an angiotensin converting enzyme (ACE) inhibitor has been shown to be effective in reducing angiotensin II levels, and demonstrated superiority in lowering blood pressure compared to ACE inhibition alone.[26] However, due to an increase in bradykinins from the inhibition of both ACE and neprilysin, there was a threefold increase in relative risk of angioedema compared with ACE inhibition alone following this combination treatment.[26] The combination of a neprilysin inhibitor with an angiotensin receptor blocker instead of the ACE inhibitor has been shown to have a comparable risk of angioedema, whilst also demonstrating superiority in treating moderate-severe heart failure to ACE inhibitor treatment.[14][27]
Neprilysin also has a role in clearing the protein amyloid beta from the cerebrospinal fluid, and its inhibition by sacubitril has shown increased levels of AB1-38 in healthy subjects (Entresto 194/206 for two weeks). Amyloid beta is considered to contribute to the development of Alzheimer's disease, and there exist concerns that sacubitril may promote the development of Alzheimer's disease.[6][28]
Chemistry
Sacubitril/valsartan is co-crystallized sacubitril and valsartan, in a one-to-one molar ratio. One sacubitril/valsartan complex consists of six sacubitril anions, six valsartan dianions, 18 sodium cations, and 15 molecules of water, resulting in the molecular formula C288H330N36Na18O48·15H2O and a molecular mass of 5748.03 g/mol.[29][30]
The substance is a white powder consisting of thin hexagonal plates. It is stable in solid form as well as in aqueous (water) solution with a pH of 5 to 7, and has a melting point of about 138 °C (280 °F).[30]
History
During its development by Novartis, Entresto was known as LCZ696.[11] It was approved under the FDA's priority review process on 7 July 2015.[13] It was also approved in Europe in 2015.[7]
Society and culture
Trial design
There was controversy over the PARADIGM-HF trial—the Phase III trial on the basis of which the drug was approved by the FDA. For example, both Richard Lehman, a physician who writes a weekly review of key medical articles for the BMJ Blog and a December 2015, report from the Institute for Clinical and Economic Review (ICER) found that the risk–benefit ratio was not adequately determined because the design of the clinical trial was too artificial and did not reflect people with heart failure that doctors usually encounter.[31]: 28 [32] In 2019, the PIONEER-HF and PARAGON-HF trials studied the effect of sacubitril/valsartan in 800 patients recently hospitalised with severe heart failure and 4800 patients with less severe symptoms of heart failure respectively.[18][16] The medication consistently demonstrated similar levels of safety, with higher rates of very low blood pressure, compared to current treatments across all three trials in a variety of patients, however it has only shown effectiveness in those with more advanced heart failure.[15][16][18] In December 2015, Steven Nissen and other thought leaders in cardiology said that the approval of sacubitril/valsartan had the greatest impact on clinical practice in cardiology in 2015, and Nissen called the drug "a truly a breakthrough approach."[33]
One 2015 review stated that sacubitril/valsartan represents "an advancement in the chronic treatment of heart failure with reduced ejection fraction" but that widespread clinical success with the drug will require taking care to use it in appropriate patients, specifically those with characteristics similar to those in the clinical trial population.[34] Another 2015 review called the reductions in mortality and hospitalization conferred by sacubitril/valsartan "striking", but noted that its effects in heart failure people with hypertension, diabetes, chronic kidney disease, and the elderly needed to be evaluated further.[35]
Economics
The wholesale cost to the National Health Service (NHS) in the UK is approximately GB£1,200 per person per year as of 2017.[36] The wholesale cost in the United States is US$4,560 per year as of 2015.[31] Similar class generic drugs without sacubitril, such as valsartan alone, cost approximately US$48 a year.[37] One industry-funded analysis found a cost of US$45,017 per Quality-adjusted life year (QALY).[38]
Research
The PARADIGM-HF trial (in which Milton Packer was one of the principal investigators) compared treatment with sacubitril/valsartan to treatment with enalapril.[39] People with heart failure and reduced LVEF (10,513) were sequentially treated on a short-term basis with enalapril and then with sacubitril/valsartan. Those that were able to tolerate both regimens (8442, 80%) were randomly assigned to long-term treatment with either enalapril or sacubitril/valsartan. Participants were mainly white (66%), male (78%), middle aged (median 63.8 +/- 11 years) with NYHA stage II (71.6%) or stage III (23.1%) heart failure.[40]
The trial was stopped early after a prespecified interim analysis revealed a reduction in the primary endpoint of cardiovascular death or heart failure in the sacubitril/valsartan group relative to those treated with enalapril. Taken individually, the reductions in cardiovascular death and heart failure hospitalizations retained statistical significance.[14] Relative to enalapril, sacubitril/valsartan provided reductions[40][41] in
- the composite endpoint of cardiovascular death or hospitalization for heart failure (incidence 21.8% vs 26.5%)
- cardiovascular death (incidence 13.3% vs 16.5%)
- first hospitalization for worsening heart failure (incidence 12.8% vs 15.6%), and
- all-cause mortality (incidence 17.0% vs 19.8%)
Limitations of the trial include scarce experience with initiation of therapy in hospitalized patients and in those with NYHA heart failure class IV symptoms.[42][43] Additionally the trial compared a maximal dose of valsartan (plus sacubitril) with a sub-maximal dose of enalapril, and was thus not directly comparable with current gold-standard use of ACE inhibitors in heart failure, diminishing the validity of the trial results.[44][45]
References
- 1 2 3 4 5 6 7 8 "Sacubitril and Valsartan Monograph for Professionals". Drugs.com. Archived from the original on 4 January 2020. Retrieved 9 October 2021.
- 1 2 3 4 5 6 BNF (80 ed.). BMJ Group and the Pharmaceutical Press. September 2020 – March 2021. p. 207. ISBN 978-0-85711-369-6.
- 1 2 3 "Entresto 24/26 tablets, Entresto 49/51 tablets, Entresto 97/103 tablets (sacubitril/valsartan) Product Information". Therapeutic Goods Administration (TGA). Novartis. Archived from the original on 11 November 2020. Retrieved 21 September 2020.
- ↑ "Sacubitril / valsartan (Entresto) Use During Pregnancy". Drugs.com. 20 November 2019. Archived from the original on 17 April 2021. Retrieved 21 September 2020.
- ↑ "Entresto 24 mg/26 mg film-coated tablets - Summary of Product Characteristics (SmPC)". (emc). Archived from the original on 24 January 2021. Retrieved 21 September 2020.
- 1 2 3 "Entresto- sacubitril and valsartan tablet, film coated". DailyMed. 14 June 2020. Archived from the original on 19 April 2020. Retrieved 21 September 2020.
- 1 2 3 "Entresto EPAR". European Medicines Agency (EMA). Archived from the original on 27 February 2021. Retrieved 21 September 2020.
- ↑ "Neparvis EPAR". European Medicines Agency (EMA). Archived from the original on 28 December 2020. Retrieved 23 September 2020.
- ↑ "Entresto Prices, Coupons & Savings Tips - GoodRx". GoodRx. Retrieved 9 October 2021.
- ↑ Chang HY, Chen KC, Fong MC, Feng AN, Fu HN, Huang KC, et al. (September 2019). "Recovery of left ventricular dysfunction after sacubitril/valsartan: predictors and management". J Cardiol. 75 (3): 233–241. doi:10.1016/j.jjcc.2019.08.005. PMID 31563433.
- 1 2 Hubers SA, Brown NJ (March 2016). "Combined Angiotensin Receptor Antagonism and Neprilysin Inhibition". Circulation. 133 (11): 1115–24. doi:10.1161/CIRCULATIONAHA.115.018622. PMC 4800749. PMID 26976916.
- ↑ Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Colvin MM, et al. (27 September 2016). "2016 ACC/AHA/HFSA Focused Update on New Pharmacological Therapy for Heart Failure: An Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America". Circulation. 134 (13): e282–93. doi:10.1161/CIR.0000000000000435. PMID 27208050.
- 1 2 "FDA approves new drug to treat heart failure" (Press release). U.S. Food and Drug Administration (FDA). 7 July 2015. Archived from the original on 26 January 2018.
- 1 2 3 4 McMurray JJ, et al. (30 August 2014). "Angiotensin–Neprilysin Inhibition versus Enalapril in Heart Failure". N Engl J Med. 371 (11): 993–1004. doi:10.1056/NEJMoa1409077. hdl:2336/552372. PMID 25176015. Archived from the original on 28 June 2021. Retrieved 6 May 2021.
- 1 2 3 4 5 6 7 8 McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, et al. (September 2014). "Angiotensin–Neprilysin Inhibition versus Enalapril in Heart Failure". New England Journal of Medicine. 371 (11): 993–1004. doi:10.1056/NEJMoa1409077. hdl:2336/552372. ISSN 0028-4793. PMID 25176015.
- 1 2 3 4 5 6 7 Solomon SD, McMurray JJ, Anand IS, Ge J, Lam CS, Maggioni AP, et al. (October 2019). "Angiotensin–Neprilysin Inhibition in Heart Failure with Preserved Ejection Fraction" (PDF). New England Journal of Medicine. 381 (17): 1609–1620. doi:10.1056/NEJMoa1908655. ISSN 0028-4793. PMID 31475794. Archived (PDF) from the original on 5 May 2020. Retrieved 6 May 2021.
- ↑ Martin N, Manoharan K, Thomas J, Davies C, Lumbers RT. Beta-blockers and inhibitors of the renin-angiotensin aldosterone system for chronic heart failure with preserved ejection fraction. Cochrane Database of Systematic Reviews 2018, Issue 6. Art. No.: CD012721. DOI: 10.1002/14651858.CD012721.pub2. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD012721.pub2/epdf/full
- 1 2 3 4 5 Velazquez EJ, Morrow DA, DeVore AD, Duffy CI, Ambrosy AP, McCague K, et al. (February 2019). "Angiotensin–Neprilysin Inhibition in Acute Decompensated Heart Failure". New England Journal of Medicine. 380 (6): 539–548. doi:10.1056/NEJMoa1812851. ISSN 0028-4793. PMID 30415601.
- ↑ Mutschler E, Schäfer-Korting M (2001). Arzneimittelwirkungen (in Deutsch) (8 ed.). Stuttgart: Wissenschaftliche Verlagsgesellschaft. p. 579. ISBN 978-3-8047-1763-3.
- ↑ Zouein FA, de Castro Brás LE, da Costa DV, Lindsey ML, Kurdi M, Booz GW (2013). "Heart Failure with Preserved Ejection Fraction". J. Cardiovasc. Pharmacol. 62 (1): 13–21. doi:10.1097/FJC.0b013e31829a4e61. PMC 3724214. PMID 23714774.
- ↑ Solomon SD. "HFpEF in the Future: New Diagnostic Techniques and Treatments in the Pipeline". Boston. p. 48. Archived from the original on 12 September 2014. Retrieved 26 January 2012.
- ↑ Gu J, Noe A, Chandra P, Al-Fayoumi S, Ligueros-Saylan M, Sarangapani R, Maahs S, Ksander G, Rigel DF, Jeng AY, Lin TH, Zheng W, Dole WP (2010). "Pharmacokinetics and pharmacodynamics of LCZ696, a novel dual-acting angiotensin receptor-neprilysin inhibitor (ARNi)". J Clin Pharmacol. 50 (4): 401–14. doi:10.1177/0091270009343932. PMID 19934029. S2CID 24853279.
- ↑ Schubert-Zsilavecz M, Wurglics M. "Neue Arzneimittel 2010/2011" (in Deutsch).
- ↑ Bevan EG, Connell JM, Doyle J, Carmichael HA, Davies DL, Lorimer AR, et al. (July 1992). "Candoxatril, a neutral endopeptidase inhibitor: efficacy and tolerability in essential hypertension". Journal of Hypertension. 10 (7): 607–13. doi:10.1097/00004872-199207000-00002. PMID 1321186. S2CID 23507064.
- 1 2 Richards AM, Wittert GA, Crozier IG, Espiner EA, Yandle TG, Ikram H, et al. (April 1993). "Chronic inhibition of endopeptidase 24.11 in essential hypertension: evidence for enhanced atrial natriuretic peptide and angiotensin II". Journal of Hypertension. 11 (4): 407–16. doi:10.1097/00004872-199304000-00011. PMID 8390508. S2CID 25333484.
- 1 2 Kostis JB, Packer M, Black HR, Schmieder R, Henry D, Levy E (February 2004). "Omapatrilat and enalapril in patients with hypertension: the Omapatrilat Cardiovascular Treatment vs. Enalapril (OCTAVE) trial". American Journal of Hypertension. 17 (2): 103–11. doi:10.1016/j.amjhyper.2003.09.014. PMID 14751650.
- ↑ Velazquez EJ, Morrow DA, DeVore AD, Duffy CI, Ambrosy AP, McCague K, et al. (February 2019). "Angiotensin–Neprilysin Inhibition in Acute Decompensated Heart Failure". The New England Journal of Medicine. 380 (6): 539–48. doi:10.1056/NEJMoa1812851. PMID 30415601.
- ↑ Patel N, Gluck J (2017). "Is Entresto good for the brain?". World J Cardiol. 9 (7): 594–599. doi:10.4330/wjc.v9.i7.594. PMC 5545143. PMID 28824789.
- ↑ Monge M, Lorthioir A, Bobrie G, Azizi M (2013). "New drug therapies interfering with the renin-angiotensin-aldosterone system for resistant hypertension". J Renin Angiotensin Aldosterone Syst. 14 (4): 285–9. doi:10.1177/1470320313513408. PMID 24222656.
- 1 2 Lili Feng, L; et al. (2012). "LCZ696: a dual-acting sodium supramolecular complex". Tetrahedron Letters. 53 (3): 275–276. doi:10.1016/j.tetlet.2011.11.029.
- 1 2 Ollendorf DA, Tarlochan Sandhu A, Chapman R, Heidenreich PA, Russo E, Shore KK, Synnott P, Travers K, Weissberg J, Pearson SD (1 December 2015). "CardioMEMS HF System (St. Jude Medical, Inc.) and Sacubitril/Valsartan (Entresto, Novartis AG) for management of congestive heart failure: effectiveness, value, and value-based price benchmarks : final report". 101672986. Archived from the original on 29 August 2021. Retrieved 6 May 2021.
- ↑ Richard Lehman's journal review—8 September 2014. NEJM 4 Sep 2014. Archived 16 May 2021 at the Wayback Machine Vol 371. The BMJ, 8 September 2014.
- ↑ Roger Sergel for Medpage Today. 5 Game-Changers in Cardiology in 2015: Entresto Archived 27 June 2021 at the Wayback Machine
- ↑ Lillyblad MP (2015). "Dual Angiotensin Receptor and Neprilysin Inhibition with Sacubitril/Valsartan in Chronic Systolic Heart Failure: Understanding the New PARADIGM". Ann Pharmacother. 49 (11): 1237–51. doi:10.1177/1060028015593093. PMID 26175499. S2CID 28918702.
- ↑ Bavishi C, Messerli FH, Kadosh B, Ruilope LM, Kario K (2015). "Role of neprilysin inhibitor combinations in hypertension: insights from hypertension and heart failure trials" (PDF). Eur. Heart J. 36 (30): 1967–73. doi:10.1093/eurheartj/ehv142. PMID 25898846. Archived (PDF) from the original on 29 April 2019. Retrieved 6 May 2021.
- ↑ "Entresto". MIMS. Archived from the original on 5 August 2017. Retrieved 25 July 2017.
- ↑ Pollack A (30 August 2014). "New Novartis Drug Effective in Treating Heart Failure". The New York Times. Archived from the original on 5 May 2021. Retrieved 6 May 2021.
- ↑ Gaziano TA, Fonarow GC, Claggett B, Chan WW, Deschaseaux-Voinet C, Turner SJ, Rouleau JL, Zile MR, McMurray JJ, Solomon SD (1 September 2016). "Cost-effectiveness Analysis of Sacubitril/Valsartan vs Enalapril in Patients With Heart Failure and Reduced Ejection Fraction". JAMA Cardiology. 1 (6): 666–72. doi:10.1001/jamacardio.2016.1747. PMID 27438344.
- ↑ Husten L (31 March 2014). "Novartis Trial Was Stopped Early Because Of A Significant Drop In Cardiovascular Mortality". Forbes. Archived from the original on 24 June 2021. Retrieved 6 May 2021.
- 1 2 King JB, Bress AP, Reese AD, Munger MA (2015). "Neprilysin Inhibition in Heart Failure with Reduced Ejection Fraction: A Clinical Review". Pharmacotherapy. 35 (9): 823–37. doi:10.1002/phar.1629. PMID 26406774. S2CID 6363036.
- ↑ Drescher CS, Desai AS (3 March 2017). "Sacubitril/Valsartan Combination Drug: 2 Years Later". American College of Cardiology. Archived from the original on 24 June 2021. Retrieved 6 May 2021.
- ↑ Havakuk O, Elkayam U (July 2017). "Angiotensin Receptor-Neprilysin Inhibition". J. Cardiovasc. Pharmacol. Ther. 22 (4): 356–364. doi:10.1177/1074248416683049. ISSN 1074-2484. PMID 28587583. S2CID 4066142.
- ↑ Perez AL, Kittipibul V, Tang WH, Starling RC (June 2017). "Patients Not Meeting PARADIGM-HF Enrollment Criteria Are Eligible for Sacubitril/Valsartan on the Basis of FDA Approval: The Need to Close the Gap". JACC Heart Fail. 5 (6): 460–463. doi:10.1016/j.jchf.2017.03.007. PMID 28571599.
- ↑ "Richard Lehman's journal review—8 September 2014". The BMJ. 8 September 2014. Archived from the original on 11 February 2018. Retrieved 20 May 2019.
- ↑ Ahn R, Prasad V (2018). "Do limitations in the design of PARADIGM-HF justify the slow real world uptake of sacubitril/valsartan (Entresto)?" (PDF). Cardiovascular Drugs and Therapy. 32 (6): 633–5. doi:10.1007/s10557-018-6830-x. PMID 30232657. S2CID 52298581. Archived (PDF) from the original on 1 November 2020. Retrieved 6 May 2021.
External links
| Identifiers: |
|---|
- "Sacubitril mixture with valsartan". Drug Information Portal. U.S. National Library of Medicine. Archived from the original on 4 January 2020. Retrieved 6 May 2021.
- AusPAR for sacubitril / valsartan salt complex (PDF) (Report). Therapeutic Goods Administration (TGA). September 2016. Archived (PDF) from the original on 29 August 2021. Retrieved 6 May 2021.