West Nile virus in the United States

The West Nile virus quickly spread across the United States after the first reported cases in Queens, New York in 1999. The virus is believed to have entered in an infected bird or mosquito, although there is no clear evidence. The disease spread quickly through infected birds. Mosquitoes spread the disease to mammals. It was mainly noted in horses but also appeared in a number of other species. The first human cases usually followed within three months of the first appearance of infected birds in the area except where cold weather interrupted the mosquito vectors. Since the virus has become widely established in the U.S., an average of 130 deaths a year occurred.
Differences in surveillance and reporting between health departments and generally increased surveillance as the disease spread cause some problems in direct comparison of the number of cases and the mortality rate. The reported number of infected in 2009 was 720, but the estimated total number of infected the same year was 54,000.[2] The true mortality rate is thought to be much lower because most cases are so mild they go undiagnosed. Some estimates put severe cases at only 1% of all cases. It is believed that the elderly or people with weak immune systems are most vulnerable to serious illness or death if bitten by a mosquito infected by West Nile.[3] Most mild cases go undiagnosed. In addition, some more severe but non-neuroinvasive cases are not reported to the CDC. Some mild cases are discovered during blood donation screening. 1,039 West Nile-tainted blood donations were discovered between 2003 and mid-2005. 30 cases of West Nile from blood transfusion were known, the majority from 2002 before blood screening was instituted.
In the first ten years since the virus arrived in the U.S., over 1,100 deaths occurred with human cases reported from every U.S. state except Maine, Alaska and Hawaii. (Animal cases have been occasionally found in Maine and in Puerto Rico.)[4] In 2012, there was a widespread outbreak with the highest death toll and second-highest total case numbers. Maine and Puerto Rico reported one case each, the first time the disease was reported in those places.[5]
Discovery in the United States
In August 1999, the New York State Department of Environmental Conservation (NYSDEC) began receiving reports of large die-offs of crows in parks across New York City. On August 9th, dead wild crows were discovered outside both the Queens Zoo and the Bronx Zoo, prompting head pathologist Dr. Tracey McNamara to begin investigating what was going on.[6] At the same time, Dr. Deborah Asnis, an infectious disease specialist at Flushing Hospital Medical Center in Queens, noticed two male patients who were suffering from similar, unusual symptoms. The two patients, aged 60 and 75 respectively, were exhibiting sudden paralysis in their arms and legs, as well as disorientation and high fevers.[7][8] Lab testing also showed elevated numbers of white blood cells within the spinal fluid of both males.[7] Neither of the patients were responding to antiviral drugs.[8] Possible early hypothesizes included botulism, viral encephalitis, Guillain–Barré syndrome, or meningitis, but none of these illnesses exactly matched the symptoms.[7] Asnis decided to pursue a more concrete diagnosis by contacting authorities and other colleagues.[7]
Dr. Asnis contacted Dr. Marcelle Layton, the New York City Department of Health's chief epidemiologist, on Monday, August 23, 1999, to report her patients' symptoms.[7] Layton advised Asnis to send samples of the patients' blood and spinal fluid to the New York State Department of Health in Albany for further analysis.[7] Around the same time, Dr. McNamara identified a potential viral encephalitis in brain tissue from the dead crows and sent samples off for further testing.[6] Meanwhile, by Friday, August 27, just four days after Asnis had contacted Layton, two additional patients had been identified in Queens.[7] The number rose to eight by Sunday, August 29, at Flushing Hospital Medical Center and other hospitals in Queens.[7] All of the early patients resided within a few miles of one another. They were also frequent gardeners in the evenings.[7]
The Centers for Disease Control and Prevention (C.D.C.) initially identified the mystery illness as St. Louis encephalitis on September 3, 1999.[7] The city of New York began widespread spraying for mosquitos later that same day.[7] However, laboratory testing continued to determine a definitive cause of the symptoms.
On September 9th, Dr. McNamara contacted the C.D.C. with concerns that the epidemiologic pattern of this outbreak were not consistent with St. Louis encephalitis, which does not cause bird die-offs. Additionally, she reported that other known avian viral diseases would have resulted in the deaths of other bird species in the zoos (avian influenza and Newcastle disease would have killed chickens in the petting zoo and eastern equine encephalitis would have killed emus on exhibit). Since only corvids appeared to be dying, she suggested the possibility of a novel pathogen. The C.D.C. disagreed that the epidemiologic pattern was inconsistent and declined to test tissue samples from animal species. Instead, Dr. McNamara sent tissue samples to the National Veterinary Services Laboratory. On September 11th, they reported that the samples she submitted were positive for a flavivirus, marking the first time a virus in this genus was implicated in an animal disease.[6]
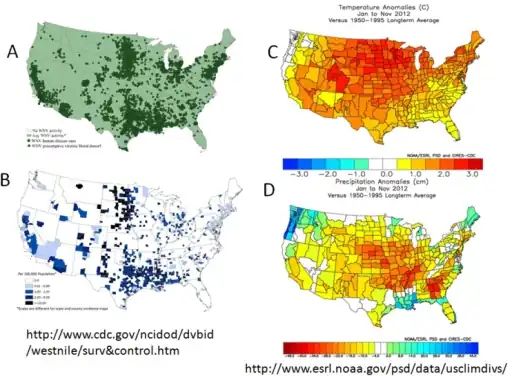
_Neuroinvasive_Disease_Incidence_9-2012.png.webp)
The U.S. federal government eventually revised its diagnosis from St. Louis encephalitis to West Nile virus on September 27, 1999, based on research by Dr. Duane J. Gubler, a C.D.C. expert on arborviruses, and their own testing on samples submitted by Dr. McNamara.[6][7]
Both Dr. McNamara and Dr. Asnis have been credited by health experts with the early identification of West Nile virus in the United States.[6][7] Their actions likely prevented a more widespread outbreak.[6][7][8] In their 2003 book, The New Killer Diseases: How the Alarming Evolution of Germs Threatens Us All, authors Elinor Levy and Mark Fischetti praised Dr. Asnis' response to the symptoms, writing that, "Asnis did something other doctors might not have bothered to do."[7] They elaborated that, "One of the worst problems with our disease-detection system is that many doctors never report cases of strange symptoms, either because they are unsure of the disease they are facing, they're ignorant of the reporting requirement, or they simply never get around to it. Deborah Asnis was highly conscientious."[7]
Recent cases
| Cases | Deaths | Mortality Rate of reported cases | |
|---|---|---|---|
| 1999 | 62 | 7 | 11% |
| 2000 | 21 | 2 | 10% |
| 2001 | 66 | 10 | 15% |
| 2002 | 4,156 | 284 | 7% |
| 2003 | 9,862 | 264 | 3% |
| 2004 | 2,539 | 100 | 4% |
| 2005 | 3,000 | 119 | 4% |
| 2006 | 4,269 | 177 | 4% |
| 2007 | 3,623 | 124 | 3% |
| 2008 | 1,356 | 44 | 3% |
| 2009 | 720 | 32 | 4% |
| 2010 | 1,021 | 57 | 6% |
| 2011 | 712 | 43 | 6% |
| 2012 | 5,674 | 286 | 5% |
| 2013 | 2,469 | 119 | 5% |
| 2014 | 2,205 | 97 | 4% |
| 2015 | 2,175 | 146 | 7% |
| 2016 | 2,149 | 106 | 5% |
| 2017 | 2,097 | 146 | 7% |
| 2018 | 2,647 | 167 | 6% |
| 2019* | 958 | 54 | 6% |
| 2020** | 540 | 33 | 6% |
Sources: Final Cumulative Maps & Data for 1999–2018 Archived 2017-10-27 at the Wayback Machine, Preliminary Maps & Data for 2019 Archived 2023-04-11 at the Wayback Machine, and West Nile Virus Disease Cases by State 2020 Archived 2022-08-22 at the Wayback Machine, Centers for Disease Control and Prevention
*2019 also had 104 presumptive cases observed in blood donors
** as of December 15, 2020, also 127 presumptive cases observed in blood donors During the years between 1999 and 2010, an estimate of 3 million people have been infected in the United States. Highest incidence rates are observed in states of the central great plains, with South Dakota, Wyoming and North Dakota leading in incidence.[9]
During the 2012 West Nile virus outbreak in Texas, 1,868 cases were reported. Male patients, persons >65 years of age, and minorities were at highest risk for neuroinvasive disease. At total of 1,868 cases including 844 (45%) WNND (West Nile neuroinvasive disease) cases and 89 deaths (case-fatality rate 5%). Dates of onset ranged from May 1, 2012, through December 6, 2012. The outbreak peaked during week 33 (mid-August) with 225 reported cases, which is historically the same peak for all reported WNV cases in Texas during 2002–2011. The median time from date of symptom onset to date of official report to TxDSHS was 27 days (range 6–274 days). Of the 254 counties in Texas, 135 (53%) reported a WNV case. The overall incidence rate for the state was 7.8 cases per 100,000 population. Almost half of the cases were reported from the northeastern quadrant of the state, including the Dallas/Fort Worth metroplex (902 [48%] cases): Dallas (396 [21%]), Tarrant (259 [14%]), Collin (64 [3%]), and Denton (183 [10%]) counties. These 4 counties had a combined incidence rate of 16 cases per 100,000 population.[10]
Maps of progression
The following maps show the progress of human cases of West Nile across the United States. States are colored according to the percentage of all U.S. West Nile cases they represented in that year. Zero percent (no cases) is colored white; less than 1% is blue; between 1% and 5% is green; between 5% and 10% is yellow, and greater than 10% of cases in a year is red.
 1999
1999 2000
2000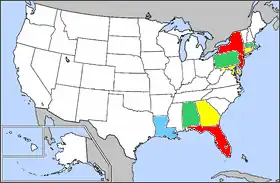 2001
2001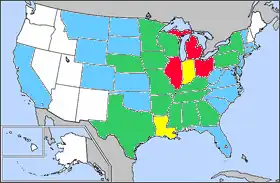 2002
2002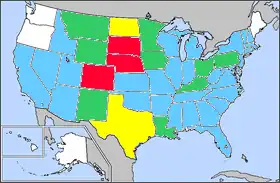 2003
2003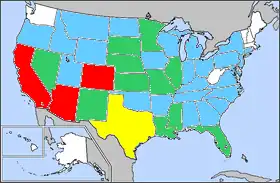 2004
2004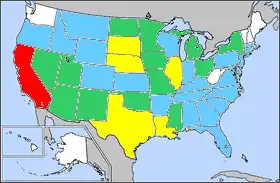 2005
2005
Counties of reported cases by year
 2001
2001 2002
2002 2003
2003 2006
2006 2007
2007 2008
2008 2009
2009 2010
2010 2011
2011 2012
2012 2013
2013 2014
2014 2015
2015 2016
2016
References
| Wikinews has related news: |
| Wikinews has related news: |
| Wikinews has related news: |
- ↑ "USGS Disease Maps". Archived from the original on 2017-05-17. Retrieved 2017-06-08.
- ↑ "West Nile Virus Activity – United States, 2009" Archived 2021-08-02 at the Wayback Machine (MMWR 59(25), July 2, 2010)
- ↑ "Why West Nile Virus is More Dangerous for Older People". 2015-07-23. Archived from the original on 2018-08-19. Retrieved 2023-04-14.
- ↑ West Nile activity maps Archived 2013-01-25 at the Wayback Machine, Centers for Disease Control and Prevention (CDC), 2009
- ↑ "West Nile Virus". CDC. Archived from the original on 11 July 2022. Retrieved 21 May 2013.
- 1 2 3 4 5 6 Wilson, James M.; McNamara, Tracey (2020-06-06). "The 1999 West Nile virus warning signal revisited". Intelligence and National Security. 35 (4): 519–526. doi:10.1080/02684527.2020.1750144. ISSN 0268-4527. S2CID 219092438. Archived from the original on 2023-04-20. Retrieved 2023-04-14.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 Roberts, Sam (2015-09-15). "Dr. Deborah Asnis, Who Sounded Alert on West Nile Virus Outbreak, Dies at 59". New York Times. Archived from the original on 2015-09-20. Retrieved 2015-10-08.
- 1 2 3 Colker, David (2015-09-21). "Deborah Asnis dies at 59; helped detect West Nile virus in U.S." Los Angeles Times. Archived from the original on 2015-10-17. Retrieved 2015-10-08.
- ↑ Peterson LR, Carson PJ, Biggerstaff BJ, Custer B, Borchardt SM, Busch MP (March 2013). "Estimated cumulative incidence of West Nile virus infection in US adults, 1999-2010". Epidemiol Infect. 141 (3): 591–595. doi:10.1017/S0950268812001070. PMC 9151873. PMID 22640592.
- ↑ Murray, KO; Ruktanonchai, D; Hesalroad, D; Fonken, E; Nolan, MS (2013-10-31). "West Nile Virus, Texas, USA, 2012". Emerging Infectious Diseases. Emerging Infectious Diseases. Volume 19, Number 11, 2013 November. 19 (11): 1836–8. doi:10.3201/eid1911.130768. PMC 3837649. PMID 24210089.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- CDC West Nile Virus Statistics, Surveillance, and Control Archived 2013-05-28 at the Wayback Machine
- West Nile Cases Drop as Immunities Emerge, Experts Say Archived 2023-04-20 at the Wayback Machine
- CDC Information Page For Current Cases and Deaths For West Nile Virus Archived 2000-09-14 at the Wayback Machine