Aberrations of the eye
The eye, like any other optical system, suffers from a number of specific optical aberrations. The optical quality of the eye is limited by optical aberrations, diffraction and scatter.[1] Correction of spherocylindrical refractive errors has been possible for nearly two centuries following Airy's development of methods to measure and correct ocular astigmatism. It has only recently become possible to measure the aberrations of the eye and with the advent of refractive surgery it might be possible to correct certain types of irregular astigmatism.
The appearance of visual complaints such as halos, glare and monocular diplopia after corneal refractive surgery has long been correlated with the induction of optical aberrations. Several mechanisms may explain the increase in the amount of higher-order aberrations with conventional eximer laser refractive procedures: a change in corneal shape toward oblateness or prolateness (after myopic and hyperopic ablations respectively), insufficient optical zone size and imperfect centration. These adverse effects are particularly noticeable when the pupil is large.[2]
Wavefront approach to aberrations of the eye

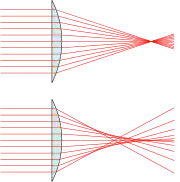
A wavefront is a surface over which an optical disturbance has a constant phase. Rays and wavefronts are two mutually complementary approaches to light propagation. Wavefronts are always normal (perpendicular) to the rays.
For light to converge to a perfect point, the wavefront emerging from the optical system must be a perfect sphere centered on the image point. The distance in micrometers between the actual wavefront and the ideal wavefront is the wavefront aberration, which is the standard method of showing the aberrations of the eye. Therefore, aberrations of the eye are the difference between two surfaces: the ideal and the actual wavefront.
Aberration of normal eyes
In normal population the dominant aberrations are the ordinary second-order spherocylindrical focus errors, which are called refractive errors. Higher order aberrations are a relatively small component, comprising about 10% of the eye's total aberrations.[3] High order aberrations increase with age and mirror symmetry exists between the right and the left eyes.[4]
Several studies have reported a compensation of the aberration of the cornea by the aberration of the crystalline lens. The spherical aberration of the cornea is usually positive whereas the young crystalline lens exhibits a negative spherical aberration. Besides, there is strong evidence of compensation for aberrations between the cornea and intraocular optics in cases of astigmatism (horizontal/vertical) and horizontal coma. The balance of corneal and internal aberrations is a typical example of creating two coupling optical systems.[5]
The accommodative response of the eye results in changes to the lens shape and substantially affects the wavefront aberration pattern. Most eyes show positive spherical aberration when unaccomodated with a trend toward negative spherical aberration on accommodation.[1]
Low order aberrations
Low order aberrations include Myopia (positive defocus), hyperopia (negative defocus), and regular astigmatism. Other lower-order aberrations are non- visually significant aberrations known as first order aberrations, such as prisms and zero-order aberrations (piston). Low order aberrations account for approximately 90% of the overall wave aberration in the eye.[5][6]
High order aberrations
There are numerous higher-order aberrations, of which only spherical aberration, coma and trefoil are of clinical interest.
Spherical aberration is the cause of night myopia and is commonly increased after myopic LASIK and surface ablation. It results in halos around point images. Spherical aberration exacerbates myopia in low light (night myopia). In brighter conditions, the pupil constricts, blocking the more peripheral rays and minimizing the effect of spherical aberration. As the pupil enlarges, more peripheral rays enter the eye and the focus shifts anteriorly, making the patient slightly more myopic in low-light conditions. In general, the increase in overall wave aberration with pupil size has been reported to increase to approximately the second power of the pupil radius. This is because most wave aberration is due to 2nd order aberrations, which have a square radius dependency.[5] The effect of spherical aberration increases as the fourth power of the pupil diameter. Doubling pupil diameter increases spherical aberration 16 times.[7] Thus, a small change in pupil size can cause a significant change in refraction. This possibility should be considered in patients who have fluctuating vision despite well-healed corneas following keratorefractive surgery.
Coma is common in patients with decentred corneal grafts, keratoconus, and decentred laser ablations.
Trefoil produces less degradation in image quality compared with coma of similar RMS magnitude.[6]
Assessment and quantitative expression of ocular aberrations
Assessment
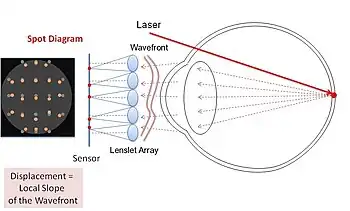
Many techniques for measuring the eye's aberrations have been described, The most common technique is Shack-Hartmann aberrometry. Other methods include Tscherning systems, ray tracing and Skiascopy methods.[2][8]
Quantitative expression
RMS
Quantitative comparisons between different eyes and conditions are usually made using RMS (root mean square). To measure RMS for each type of aberration involves squaring the difference between the aberration and mean value and averaging it across the pupil area. Different kinds of aberrations may have equal RMS across the pupil but have different effects on vision, therefore, RMS error is unrelated to visual performance. The majority of eyes have total RMS values less than 0.3 µm.[6]
Zernike polynomials
The most common method of classifying the shapes of aberration maps is to consider each map as the sum of fundamental shapes or basis functions. One popular set of basis functions are the Zernike polynomials.[2] Each aberration may be positive or negative in value and induces predictable alterations in the image quality.[9] Because there is no limit to the number of terms that may be used by Zernike polynomials, vision scientists use the first 15 polynomials, based on the fact that they are enough to obtain a highly accurate description of the most common aberrations found in human eye.[10] Among these the most important Zernike coefficients affecting visual quality are coma, spherical aberration, and trefoil.[6]
Zernike polynomials are usually expressed in terms of polar coordinates (ρ,θ), where ρ is radial coordinate and θ is the angle. The advantage of expressing the aberrations in terms of these polynomials includes the fact that the polynomials are independent of one another. For each polynomial the mean value of the aberration across the pupil is zero and the value of the coefficient gives the RMS error for that particular aberration (i.e. the coefficients show the relative contribution of each Zernike mode to the total wavefront error in the eye).[4] However these polynomials have the disadvantage that their coefficients are only valid for the particular pupil diameter they are determined for.
In each Zernike polynomial , the subscript n is the order of aberration, all the Zernike polynomials in which n=3 are called third-order aberrations and all the polynomials with n=4, fourth order aberrations and so on. and are usually called secondary Astigmatism and should not cause confusion. The superscript m is called the angular frequency and denotes the number of times the Wavefront pattern repeats itself.[4]
List of Zernike modes and their common names:[11]
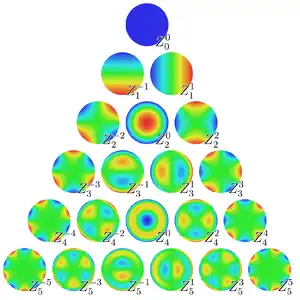
| Zernike Term | Name |
|---|---|
| Piston | |
| , | Tilt (Prism) |
| Defocus | |
| , | Astigmatism |
| , | Secondary Astigmatism |
| Spherical aberration | |
| , | Coma |
| , | Trefoil |
| , | Quadrafoil |
Management
Low order aberrations (hyperopia, Myopia and regular astigmatism), are correctable by eyeglasses, soft contact lenses and refractive surgery. Neither spectacles nor soft contact lenses nor routine keratorefractive surgery adequately corrects high order aberrations. Significant high order aberration usually requires a rigid gas-permeable contact lens for optimal visual rehabilitation.[6]
Customized Wavefront-guided refractive corneal laser treatments are designed to reduce existing aberrations and to help prevent the creation of new aberrations.[6] The wavefront map of the eye may be transferred to a Lasik system and enable the surgeon to treat the aberration. Perfect alignment of the treatment and the pupil on which the Wavefront is measured is required, which is usually achieved through iris feature detection. An efficient eye tracking system and small spot size laser is necessary for treatment . Wavefront customization of ablation increases the depth of ablation because additional corneal tissue must be ablated to compensate for the high order aberrations.[2] Actual results with Wavefront guided LASIK showed that not only it cannot remove HOA but also the optical aberrations are increased. However, the amount of increase in aberrations are less than conventional Lasik.[12] Corneal optical aberrations after photorefractive keratectomy with a larger ablation zone and a transition zone are less pronounced and more physiologic than those associated with first-generation (5 mm) ablations with no transition zone.[13] An upcoming systematic review will seek to compare the safety and effectiveness of wavefront excimer laser refractive surgery with conventional excimer laser refractive surgery, and will measure differences in residual higher order aberrations between the two procedures.[14]
Aspherical intraocular lenses (IOLs) have been used clinically to compensate for positive corneal spherical aberrations. Although Aspherical IOLs may give better contrast sensitivity, it is doubtful, whether they have a beneficial effect on distance visual acuity. Conventional (not Aspherical) IOLs give better depth of focus and better near vision. The reason for improved depth of focus in conventional lenses is linked to residual spherical aberration. The small improvement in depth of focus with the conventional IOLs enhances uncorrected near vision and contribute to reading ability.[15]
Wavefront customized lenses can be used in eyeglasses. Based on Wavefront map of the eye and with the use of laser a lens is shaped to compensate for the aberrations of the eye and then put in the eyeglasses. Ultraviolet Laser can alter the refractive index of curtain lens materials such as epoxy polymer on a point by point basis in order to generate the desired refractive profile.[1]
Wavefront customized contact lenses can theoretically correct HOA. The rotation and decentration reduces the predictability of this method.[1]
See also
- Optical aberrations
- Wavefront
- Zernike polynomials
References
- 1 2 3 4 Cerviño, A; Hosking, SL; Montes-Mico, R; Bates, K (Jun 2007). "Clinical ocular wavefront analyzers". Journal of Refractive Surgery. 23 (6): 603–16. doi:10.3928/1081-597X-20070601-12. PMID 17598581.
- 1 2 3 4 Dimitri T. Azar; Damien Gatinel; Thang Hoang-Xuan (2007). Refractive surgery (2nd ed.). Philadelphia: Mosby Elsevier. ISBN 978-0-323-03599-6.
- ↑ Lawless, MA; Hodge, C (Apr 2005). "Wavefront's role in corneal refractive surgery". Clinical & Experimental Ophthalmology. 33 (2): 199–209. doi:10.1111/j.1442-9071.2005.00994.x. PMID 15807834. S2CID 39844061.
- 1 2 3 Charman, WN (Jun 2005). "Wavefront technology: past, present and future". Contact Lens & Anterior Eye : The Journal of the British Contact Lens Association. 28 (2): 75–92. doi:10.1016/j.clae.2005.02.003. PMID 16318838.
- 1 2 3 Lombardo, M; Lombardo, G (Feb 2010). "Wave aberration of human eyes and new descriptors of image optical quality and visual performance". Journal of Cataract and Refractive Surgery. 36 (2): 313–31. doi:10.1016/j.jcrs.2009.09.026. PMID 20152616.
- 1 2 3 4 5 6 Basic and Clinical Science Course, Section 13: Refractive Surgery (2011-2012. ed.). American Academy of Ophthalmology. 2011–2012. pp. 7–9. ISBN 978-1615251209.
- ↑ Basic and Clinical Science Course, Section 3: Clinical Optics (2011-2012 last major rev. 2010-2012. ed.). American Academy of Ophthalmology. 2011–2012. p. 100. ISBN 978-1615251100.
- ↑ Myron Yanoff; Jay S. Duker (2009). Ophthalmology (3rd ed.). Mosby Elsevier. p. 104. ISBN 978-0-323-04332-8.
- ↑ Applegate, RA; Thibos, LN; Hilmantel, G (Jul 2001). "Optics of aberroscopy and super vision". Journal of Cataract and Refractive Surgery. 27 (7): 1093–107. CiteSeerX 10.1.1.597.7451. doi:10.1016/s0886-3350(01)00856-2. PMID 11489582. S2CID 29323497.
- ↑ Thibos, LN; Applegate, RA; Schwiegerling, JT; Webb, R (Sep–Oct 2000). "Report from the VSIA taskforce on standards for reporting optical aberrations of the eye". Journal of Refractive Surgery. 16 (5): S654–5. PMID 11019893.
- ↑ Wyant, James C. "Zernike Polynomials".
- ↑ Kohnen, T; Bühren, J; Kühne, C; Mirshahi, A (Dec 2004). "Wavefront-guided LASIK with the Zyoptix 3.1 system for the correction of myopia and compound myopic astigmatism with 1-year follow-up: clinical outcome and change in higher order aberrations". Ophthalmology. 111 (12): 2175–85. doi:10.1016/j.ophtha.2004.06.027. PMID 15582071.
- ↑ Endl, MJ; Martinez, CE; Klyce, SD; McDonald, MB; Coorpender, SJ; Applegate, RA; Howland, HC (Aug 2001). "Effect of larger ablation zone and transition zone on corneal optical aberrations after photorefractive keratectomy". Archives of Ophthalmology. 119 (8): 1159–64. doi:10.1001/archopht.119.8.1159. PMID 11483083.
- ↑ Li SM, Kang MT, Zhou Y, Wang NL, Lindsley K (2017). "Wavefront excimer laser refractive surgery for adults with refractive errors". Cochrane Database Syst Rev. 6: CD012687. doi:10.1002/14651858.CD012687. PMC 6481747.
- ↑ Nanavaty, MA; Spalton, DJ; Boyce, J; Saha, S; Marshall, J (Apr 2009). "Wavefront aberrations, depth of focus, and contrast sensitivity with aspheric and spherical intraocular lenses: fellow-eye study". Journal of Cataract and Refractive Surgery. 35 (4): 663–71. doi:10.1016/j.jcrs.2008.12.011. PMID 19304086. S2CID 10016253.