Autonomic dysreflexia
| Autonomic dysreflexia | |
|---|---|
| Other names: Autonomic hyperreflexia, mass reflex[1] | |
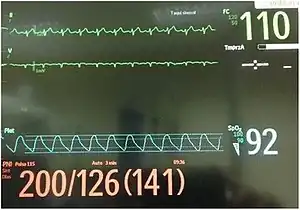 | |
| Vital signs in a person with autonomic dysreflexia after atropine was given for a slow heart rate[2] | |
| Specialty | Neurology |
| Symptoms | Episodes of high blood pressure, headache, slow heart rate, sweating above injury[3] |
| Complications | Stroke, intracranial bleed, pulmonary edema, seizures[3] |
| Usual onset | Month to year post injury[3] |
| Causes | Spinal cord injury[3] |
| Risk factors | Injury above T6[3] |
| Diagnostic method | Based on symptom together with a 25 mmHg increase in SBP[3] |
| Differential diagnosis | Cushing's syndrome, hyperthyroid, nephrotic syndrome, drug use[3] |
| Prevention | Education[1] |
| Treatment | Sit the person upright, removing any constrictive clothing, address the trigger[4][5] |
| Medication | Nitroglycerin, prazosin, nifedipine, hydralazine[4][5][3] |
| Frequency | ~45% of injuries above T6[3] |
| Deaths | 22%[6] |
Autonomic dysreflexia (AD) is a condition that may occur after a spinal cord injury.[3] Symptoms include episodes of high blood pressure which may result in headaches.[3] During these episoids sweating above the level of injury, stuffy nose, low heart rate, and anxiety may also occur.[3] Onset is often a month to a year after injury.[3] Multiple episodes may occur a day.[3] Complications may include stroke, intracranial bleed, pulmonary edema, and seizures.[3]
It most commonly occurs with lesions above the T6 spinal cord level, although there are reports with as low as T10.[3] The risk is greater the higher the level of injury.[3] Common triggers for attacks include urinary tract infections, urinary retention, constipation, and hemorrhoids.[3][4] The underlying mechanism involves over activity of the sympathetic nervous system with a lack of compensatory parasympathetic response.[3] Diagnosis may be based on symptoms together with blood pressure measurement.[3]
It is a medical emergency.[4] Initial treatment involves sitting the person upright, removing any constrictive clothing, and addressing whatever triggered the episode.[4][5] This may require a urinary catheter or digital disimpaction of the bowels.[5][6] If blood pressure remains above 150 mmHg, medications such as nitroglycerin, prazosin, nifedipine, or hydralazine may be used.[4][5][3] Other measures may include injecting botox into the bladder.[5] Prevention involves education regarding potential precipitating events.[1]
Autonomic dysreflexia occurs in 20 to 70% of people with a spinal cord injury above T6.[3] It is associated with a 22% risk of death.[6] The condition was first described in 1860 by Hilton.[7] Many people with the condition carry medications to treat the condition out in the community.[6]
Signs and symptoms
This condition is distinct and usually episodic, with the people potentially experiencing remarkably high blood pressure, intense headaches, profuse sweating, facial erythema, goosebumps, nasal stuffiness, a "feeling of doom" or apprehension, and blurred vision.[8] An elevation of 20 mm Hg over baseline systolic blood pressure, with a potential source below the neurological level of injury, meets the current definition of dysreflexia.[9]
Complications
Autonomic dysreflexia can become chronic and recurrent, often in response to longstanding medical problems like soft tissue pressure injuries or hemorrhoids. Long term therapy may include alpha blockers or calcium channel blockers.
Complications of severe acute hypertension can include seizures, pulmonary edema, myocardial infarction, or cerebral hemorrhage. Additional organs that may be affected include the kidneys and retinas of the eyes.[8]
Causes
The first episode of autonomic dysreflexia may occur weeks to years after spinal cord injury takes place, but most people at risk (80%) develop their first episode within the first year after injury. Early AD tends to be associated with less severe increases in blood pressure.
One common causative factor may be an undetected urinary tract infection. The difficulty in assessing this may be complicated with the usage of indwelling or suprapubic catheters. Other causes include medication side effects and various disease processes. The use of stimulants such as cocaine and amphetamines which can result in urinary retention, and the use of CNS depressants and other psychoactive drugs can also lead to urinary retention and constipation thus leading to autonomic dysreflexia when in use over an extended period of time.
Pain
Painful stimuli are the primary initiators of AD. (Note: Not all noxious stimuli will cause AD. Some otherwise severe noxious stimuli in normal people, e.g. broken bones, may not result in AD, and may in fact even go unnoticed.) However, different studies have found that activation of pain receptors in muscle and skin below the lesion in spinal cord injured individuals did not trigger AD.[10][11] These studies suggests that not all noxious stimuli are reliable triggers of AD, and because non-noxious stimuli can also trigger AD, attribution of an episode of AD to noxious stimuli may cause clinicians to overlook underlying non-noxious triggers. As a result, non-noxious trigger factors remain undetected, prolonging an episode of AD. They concluded that when deducing the potential causes of AD it is important to consider non-noxious sources of stimulation in addition to noxious triggers. Current assessment of autonomic dysreflexia in patients with known causative factors include palpation of the bladder and bowel and can also include bladder scan.
Mechanism
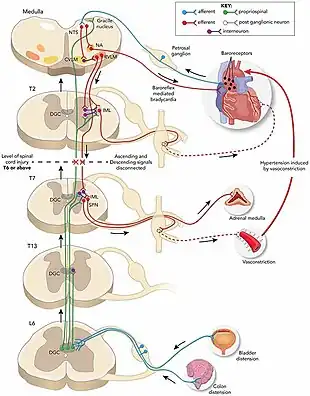
Supraspinal vasomotor neurons send projections to the intermediolateral cell column, which is composed of sympathetic preganglionic neurons (SPN) through the T1-L2 segments.[5] The supraspinal neurons act on the SPN and its tonic firing, modulating its action on the peripheral sympathetic chain ganglia and the adrenal medulla.[5] The sympathetic ganglia act directly on the blood vessels they innervate throughout the body, controlling vessel diameter and resistance, while the adrenal medulla indirectly controls the same action through the release of epinephrine and norepinephrine.[5] The descending autonomic pathways, which are responsible for the supraspinal communication with the SPN, are interrupted resulting in decreased sympathetic outflow below the level of the injury.[5] In this circumstance, the SPN is controlled only by spinal influences.[5] The first couple of weeks after a spinal injury, the decreased sympathetic outflow causes reduced blood pressure and sympathetic reflex.[5] Eventually, synaptic reorganization and plasticity of SPN develops into an overly sensitive state, which results in abnormal reflex activation of SPN due to afferent stimuli, such as bowel or bladder distension.[5] Reflex activation results in systemic vasoconstriction below the spinal cord disruption. The peripheral arterial vasoconstriction and hypertension activates the baroreceptors, resulting in a parasympathetic surge originating in the central nervous system, which inhibits the sympathetic outflow; however, the parasympathetic signal is unable to transmit below the level of the spinal cord lesion.[13] This results in vasodilation, flushing, pupillary constriction and nasal stuffiness above the spinal lesion, while there's piloerection, pale and cool skin below the lesion due to the prevailing sympathetic outflow.[13] Reason this issue is much more prominent for lesions at or above the T6 level is because the Splanchnic nerves emerge from the T5 level and below. Loss of brain's control over T6 and below causes splanchnic arteries to reflexively vasoconstrict and since the Splanchnic arteries are the body's largest reservoir for circulating blood, their vasocontriction dramatically affects the blood pressure of the body.
Diagnosis
The symptoms are usually not subtle, although asymptomatic events have been documented. Autonomic dysreflexia differs from autonomic instability, the various modest cardiac and neurological changes that accompany a spinal cord injury, including bradycardia, orthostatic hypotension, and ambient temperature intolerance. In autonomic dysreflexia, patients will experience hypertension, sweating, spasms (sometimes severe spasms) and erythema (more likely in upper extremities) and may suffer from headaches and blurred vision. Mortality is rare with AD, but morbidity such as stroke, retinal hemorrhage and pulmonary edema if left untreated can be quite severe. Older patients with very incomplete spinal cord injuries and systolic hypertension without symptoms are usually experiencing essential hypertension, not autonomic dysreflexia. Aggressive treatment of these elderly patients with rapidly acting antihypertensive medications can have disastrous results.
Treatment
Proper treatment of autonomic dysreflexia involves administration of anti-hypertensives along with immediate determination and removal of the triggering stimuli. Often, sitting the patient up and dangling legs over the bedside can reduce blood pressures below dangerous levels and provide partial symptom relief. Tight clothing and stockings should be removed. Straight catheterization of the bladder or relief of a blocked urinary catheter tube may resolve the problem. The rectum should be cleared of stool impaction, using anaesthetic lubricating jelly. If the noxious precipitating trigger cannot be identified, drug treatment is needed to decrease elevating intracranial pressure until further studies can identify the cause.
Commonly used medications include sublingual nitrates 1 to 2 sprays every 20 min or 10 mg nifedipine every 20 min.[6] Other options include hydralazine or clonidine. Topical nitroglycerin ointment may also be used—an inch or two can be applied to the chest wall or forehead, and wiped off when blood pressures begin to normalize.[14] Autonomic dysreflexia is abolished temporarily by spinal or general anaesthesia. These treatments are used during obstetric delivery of women with autonomic dysreflexia.
People should be monitored for two hours after an episode has improved.[6]
Prognosis
The cause of autonomic dysreflexia itself can be life-threatening, and must also be completely investigated and treated appropriately to prevent unnecessary morbidity and mortality.
The Consortium for Spinal Cord Medicine has developed evidence-based clinical practice guidelines for the management of autonomic dysreflexia in adults, children, and pregnant women. There is also a consumer version of this guideline.
References
- 1 2 3 Consortium for Spinal Cord Medicine (2002). "Acute management of autonomic dysreflexia: individuals with spinal cord injury presenting to health-care facilities". The Journal of Spinal Cord Medicine. 25 Suppl 1: S67–88. PMID 12051242.
- ↑ Leão, P; Figueiredo, P (2016). "Autonomic hyperreflexia after spinal cord injury managed successfully with intravenous lidocaine: a case report". Patient safety in surgery. 10: 10. doi:10.1186/s13037-016-0098-5. PMID 26985238.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 Allen, KJ; Leslie, SW (January 2021). "Autonomic Dysreflexia". PMID 29494041.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 3 4 5 6 Krassioukov A, Warburton DE, Teasell R, Eng JJ (April 2009). "A systematic review of the management of autonomic dysreflexia after spinal cord injury". Archives of Physical Medicine and Rehabilitation. 90 (4): 682–95. doi:10.1016/j.apmr.2008.10.017. PMC 3108991. PMID 19345787.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Eldahan KC, Rabchevsky AG (January 2018). "Autonomic dysreflexia after spinal cord injury: Systemic pathophysiology and methods of management". Autonomic Neuroscience. 209: 59–70. doi:10.1016/j.autneu.2017.05.002. PMC 5677594. PMID 28506502.
- 1 2 3 4 5 6 Cowan, H; Lakra, C; Desai, M (2020-10-02). "Autonomic dysreflexia in spinal cord injury". BMJ (Clinical research ed.). 371: m3596. doi:10.1136/bmj.m3596. PMID 33008797.
- ↑ Atlee, John L. (2007-01-01). Complications in Anesthesia. Elsevier Health Sciences. p. 853. ISBN 978-1-4160-2215-2. Archived from the original on 2021-08-27. Retrieved 2021-05-30.
- 1 2 Vallès M, Benito J, Portell E, Vidal J (December 2005). "Cerebral hemorrhage due to autonomic dysreflexia in a spinal cord injury patient". Spinal Cord. 43 (12): 738–40. doi:10.1038/sj.sc.3101780. PMID 16010281.
- ↑ Krassioukov, Andrei; Biering-Sørensen, Fin; Donovan, William; Kennelly, Michael; Kirshblum, Steven; Krogh, Klaus; Alexander, Marca Sipski; Vogel, Lawrence; Wecht, Jill (2012). "International standards to document remaining autonomic function after spinal cord injury". The Journal of Spinal Cord Medicine. 35 (4): 201–210. doi:10.1179/1079026812Z.00000000053. PMC 3425876. PMID 22925746.
- ↑ Burton AR, Brown R, Macefield VG (October 2008). "Selective activation of muscle and skin nociceptors does not trigger exaggerated sympathetic responses in spinal-injured subjects". Spinal Cord. 46 (10): 660–5. doi:10.1038/sc.2008.33. PMID 18427566.
- ↑ Marsh DR, Weaver LC (June 2004). "Autonomic dysreflexia, induced by noxious or innocuous stimulation, does not depend on changes in dorsal horn substance p". Journal of Neurotrauma. 21 (6): 817–28. doi:10.1089/0897715041269605. PMID 15253807.
- ↑ Michael, Felicia M.; Patel, Samir P.; Rabchevsky, Alexander G. (2019-11-08). "Intraspinal Plasticity Associated With the Development of Autonomic Dysreflexia After Complete Spinal Cord Injury". Frontiers in Cellular Neuroscience. 13: 505. doi:10.3389/fncel.2019.00505.
- 1 2 Youmans and Winn neurological surgery. Winn, H. Richard (Seventh ed.). Philadelphia, PA. 30 November 2016. ISBN 9780323287821. OCLC 963181140.
{{cite book}}: CS1 maint: others (link) - ↑ Solinsky, R.; Bunnell, A. E.; Linsenmeyer, T. A.; Svircev, J. N.; Engle, A.; Burns, S. P. (2017). "Pharmacodynamics and effectiveness of topical nitroglycerin at lowering blood pressure during autonomic dysreflexia". Spinal Cord. 55 (10): 911–914. doi:10.1038/sc.2017.58. PMID 28585557.
External links
| Classification | |
|---|---|
| External resources |