Costochondritis
| Costochondritis | |
|---|---|
| Other names: Costosternal syndrome,[1] anterior chest wall syndrome,[1] costosternal chondrodynia,[2] parasternal chondrodynia[1] | |
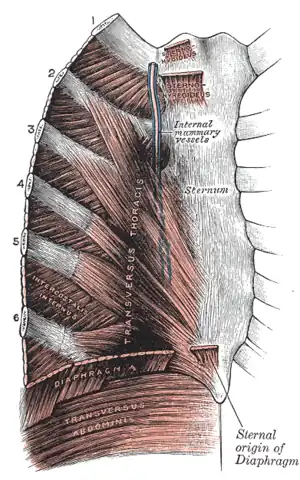 | |
| The costal cartilages | |
| Specialty | Emergency medicine |
| Symptoms | Pain and tenderness at the costal cartilage[3] |
| Duration | Weeks to months[1] |
| Risk factors | Repetitive physical activities, preceding cough[3][1] |
| Diagnostic method | Based on symptoms after ruling out other causes[4][5] |
| Differential diagnosis | Heart attack, angina, heartburn, pneumonia, pulmonary embolism, shingles, Tietze's syndrome[4][1] |
| Treatment | NSAIDs, ice and heat, physiotherapy[5][1] |
| Prognosis | Good[5] |
| Frequency | ~25% of chest pain[1] |
Costochondritis is chest wall pain at the costal cartilage, the structure that connects each rib to the sternum.[5] The pain is generally localized and can be recreated by pushing on the area.[4] Multiple areas of cartilage may be involved.[1] Pain may be worsened with certain movements and taking a deep breath.[5] The quality of the pain may be sharp or dull.[5] Costochondritis typically resolves with time, though may recur.[5]
Risk factors include repetitive physical activities or a preceding cough.[3][1] Diagnosis involves ruling out other conditions that may present similarly including: heart attack, angina, heartburn, pneumonia, and pulmonary embolism.[5][4] Vital signs are generally normal.[5] The underlying mechanism is believed to involved inflammation.[1] If swelling is involved the condition is known as Tietze's syndrome, a term which maybe used interchangeably but is considered a separate disease.[1][6]
Chest pain is considered a medical emergency until life-threatening diseases are ruled out.[5] Treatment of costochondritis may include rest, ice and heat, paracetamol (acetaminophen), and nonsteroidal anti-inflammatory medication (NSAIDs).[1] Persistent cases may be managed with physiotherapy[5] or local steroid injections.[1] Costochondritis represents about 13 to 36%% of cases of chest pain.[4][1] Both children and adults may be affected.[1]
Signs and symptoms
Pain or tenderness to palpation usually occurs on the sides of the sternum, affects multiple ribs, and is often worsened with coughing, deep breathing, or physical activity.[6][7] On physical examination, a physician inspects and feels the patient for swollen or tender areas, and can often produce the pain of costochondritis by moving the patient's rib cage or arms.[6][1][8][9]
A factor that may aid in the differentiation of costochondritis from Tietze syndrome is the location of the pain on the sternum. Costochondritis typically affects the third, fourth, and fifth costosternal joints in contrast to Tietze's syndrome, which usually affects the second or third costosternal joint.[8] Pain from costochondritis typically resolves within one year.[10]
Causes
In most cases of costochondritis, no cause is identified.[2][6][11] However, it may be the result of physical trauma (due to direct injury, strenuous lifting, or severe bouts of coughing), associated with scoliosis, ankylosing spondylitis, rheumatoid arthritis, osteoarthritis, or a tumor (benign or cancerous).[12]
Infection of the costosternal joint may cause costochondritis in rare cases. Most cases of infectious costochondritis are caused by Actinomyces, Staphylococcus aureus, Candida albicans, and Salmonella. In rare cases, Escherichia coli can be a cause of infectious costochondritis.[13] There are reports of an associated with chest binding, as practiced by some members of the transgender community.[14]
Pathogenesis
The pathogenesis underlying the development of costochondritis remains unclear. Proposed mechanisms of injury include neurogenic inflammation, muscular imbalance, increased muscular pull on the rib,[10] mechanical dysfunction at the costotransverse joint of the rib,[10] or a derangement of the mechanical structure of the costochondral junction.[15]
Diagnosis
Diagnosis is based on symptoms after ruling out other potential causes.[4][5] Pain that can be produced by pushing on the chest wall does not rule out a heart attack.[1]
Differential diagnosis
Other causes of chest pain similar to that produced by costochondritis may include:[15][16]
- Cardiac:
- Gastrointestinal:[11]
- Musculoskeletal:
- Fibromyalgia
- Rib fracture
- Ankylosing spondylitis
- Bone metastasis from cancers such as prostate cancer, breast cancer, plasmacytoma, and sarcomas[8]
- Reactive arthritis[8]
- Psychogenic:
- Respiratory:
- Other:
Treatment
Costochondritis may be treated rest, ice, heat, and pain medications.[1] Medication may include nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or paracetamol (acetaminophen).[1] Persistent cases may be managed with physiotherapy[5] or local steroid injections.[1] In severe cases opioids, tricyclic antidepressantss such as amitriptyline, or gabapentin may be used.[18] While steroids by mouth or by injection may be used for cases unresponsive to NSAIDs; this treatment has not been well studied.[19] Rest from stressful physical activity is often advised during the recovery period.[1]
Epidemiology
Costochondritis is a common condition and is responsible for 30% of emergency room chest-pain-related visits. One-fifth of visits to the primary care physician are for musculoskeletal chest pain; of this 20% of primary care office visits, 13% are due to costochondritis.[15] Costochondritis cases are most often seen in people older than age 40 and occur more often in women than in men.[8]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 Proulx, AM; Zryd, TW (2009). "Costochondritis: diagnosis and treatment". American Family Physician. 80 (6): 617–620. PMID 19817327.
- 1 2 Mayo Clinic Staff (2012). "Costochondritis Definition". Mayo Clinic. Archived from the original on 2 January 2014. Retrieved 26 December 2012.
- 1 2 3 Stochkendahl, MJ; Christensen, HW (2010). "Chest pain in focal musculoskeletal disorders". The Medical Clinics of North America. 94 (2): 259–273. doi:10.1016/j.mcna.2010.01.007. PMID 20380955.
- 1 2 3 4 5 6 McConaghy, JR; Oza, RS (1 February 2013). "Outpatient diagnosis of acute chest pain in adults". American family physician. 87 (3): 177–82. PMID 23418761.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Schumann, JA; Sood, T; Parente, JJ (January 2020). "Costochondritis". PMID 30422526.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 3 4 Jindal, A; Singhi, S (2011). "Acute chest pain". Indian Journal of Pediatrics. 78 (10): 1262–1267. doi:10.1007/s12098-011-0413-1. PMID 21541647.
- ↑ Mayo Clinic Staff (2012). "Costochondritis:Symptoms". Mayo Clinic. Archived from the original on 12 December 2013. Retrieved 26 December 2012.
- 1 2 3 4 5 Fauci, Anthony S.; Eugene Braunwald; Dennis L. Kasper; Stephen L. Hauser; Dan L. Longo; J. Larry Jameson; Joseph Loscalzo (2008). Chapter 330. Arthritis Associated with Systemic Disease, and Other Arthritides Harrison's principles of internal medicine (17th ed.). New York: McGraw-Hill. ISBN 978-0-07-147693-5.
- ↑ Mayo Clinic Staff (2012). "Costochondritis:Tests and diagnosis". Mayo Clinic. Archived from the original on 12 December 2013. Retrieved 26 December 2012.
- 1 2 3 Sik EC, Batt ME, Heslop LM (March–April 2009). "Atypical chest pain in athletes". Curr Sports Med Rep. 8 (2): 52–8. doi:10.1249/JSR.0b013e31819c7d01. PMID 19280769.
- 1 2 3 Ricker Polsdorfer, M.D. (2012). "Costochondritis". Keck Medical Center of USC. Archived from the original on 26 May 2013. Retrieved 30 December 2012.
- ↑ Mayo Clinic Staff (2012). "Causes". Mayo Clinic. Archived from the original on 19 May 2017. Retrieved 26 December 2012.
- ↑ Sakran, W; Bisharat, N (2011). "Primary Chest Wall Abscess Caused by Escherichia coli Costochondritis". Am J Med Sci. 342 (3): 241–6. doi:10.1097/MAJ.0b013e31821bc1b0. PMID 21681074.
- ↑ McClean Clinic (2014). "Consequences of Chest Binding". McClean Clinic. Archived from the original on 1 November 2020. Retrieved 24 October 2016.
- 1 2 3 Ayloo A, Cvengros T, Marella S (December 2013). "Evaluation and treatment of musculoskeletal chest pain". Prim Care (Review). 40 (4): 863–87. doi:10.1016/j.pop.2013.08.007. PMID 24209723.
- ↑ "Costochondritis Diagnosis Differential". BMJ Publishing Group. 2012. Archived from the original on 1 June 2009. Retrieved 26 December 2012.
- ↑ Seferović PM, Ristić AD, Maksimović R, Simeunović DS, Milinković I, Seferović Mitrović JP, Kanjuh V, Pankuweit S, Maisch B (May 2013). "Pericardial syndromes: an update after the ESC guidelines 2004". Heart Fail Rev. (Review). 18 (3): 255–66. doi:10.1007/s10741-012-9335-x. PMID 22855353.
- ↑ "Treatments and drugs". Mayo Clinic. 2012. Archived from the original on 9 December 2013. Retrieved 26 December 2012.
- ↑ Gandhi V, Costello J (August 2012). "Towards evidence based emergency medicine: best BETs from the Manchester Royal Infirmary. BET 3: The use of corticosteroids in the management of costochondritis". Emerg Med J (Review). 29 (8): 686. doi:10.1136/emermed-2012-201590.4. PMID 22787240.
External links
| Classification | |
|---|---|
| External resources |
- Benign Tender Chest Wall Pain of Costosternal Joints Inflammation at patient.info Archived 2015-10-21 at the Wayback Machine