Endometrial stromal sarcoma (low-grade)
| Endometrial stromal sarcoma | |
|---|---|
 | |
| Specialty | Oncology, gynecology |
| Symptoms | Abnormal uterine bleeding, pelvic pain, mass of the uterus, spread[1] |
| Usual onset | Females in their 50s[1] |
| Risk factors | Estrogen, tamoxifen, pelvic irradiation[1] |
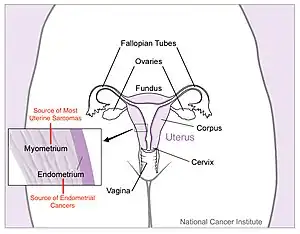
Low-grade endometrial stromal sarcoma (LGESS) is a type of cancer in the uterus.[2] It typically occurs in females in their 50s, and presents with abnormal uterine bleeding, pelvic pain, and mass of the uterus.[1] Local, nodal or distant spread to lungs may be found at first presentation.[1]
It is a subtype of endometrial stromal tumor belonging to the mesenchymal tumors of the main body of the uterus.[1] It is distinct to and less aggressive than high-grade endometrial stromal sarcoma.[2]
Taking estrogen for a long duration, tamoxifen use, and radiation to the pelvis, may increase the risk of developing LGESS.[1]
Pathology
Low-grade endometrial stromal sarcoma consists of cells resembling normal proliferative phase endometrium, but with infiltration or vascular invasion. These behave less[3] aggressively, sometimes metastasizing, with cancer stage the best predictor of survival. The cells express estrogen/progesterone-receptors.
Macroscopy
- Polypoid mass extending into broad ligament, ovaries and fallopian tubes.
- Lymphatic tumor plugs as yellow, ropy or ball-like masses.
Microscopy

- Monotonous ovoid cells to spindly cells with minimal cytoplasm.
- Prominent arterioles. Angiolymphatic invasion common.
- Up to 10-15 mitotic figures per 10 HPF in most active areas.
- Tongue-like infiltration between muscle bundles of myometrium.
- May exhibit myxoid, epithelioid and fibrous change.
- May have foam cells or hyalinization in the stroma.
Immunochemistry
- CD10+
- muscle markers (muscle specific actin MSA, smooth muscle actin SMA and desmin) positive in areas of smooth muscle differentiation
- CD117- (c-kit -)
- h-caldesmon-
Genetic features
A recurrent chromosomal translocation, t(7;17)(p15;q21), occurs in endometrial stromal sarcoma. This translocation leads to the fusion of two polycomb group genes, JAZF1 and JJAZ1, with production of a fusion transcript with anti-apoptotic properties. Even normal endometrial stroma cells express the fusion gene, derived not by translocation, but by the "stitching" together of m-RNAs. Thus, it appears that a pro-survival gene in the normal endometrium is somehow subverted to become pro-neoplastic.[4]
History
It was previously known as endolymphatic stromal myosis because of diffuse infiltration of myometrial tissue or the invasion of lymphatic channels.[5]
References
- 1 2 3 4 5 6 7 WHO Classification of Tumours Editorial Board, ed. (2020). "6. Tumours of the uterine corpus: low-grade endometrial stromal sarcoma". Female genital tumours: WHO Classification of Tumours. Vol. 4 (5th ed.). Lyon (France): International Agency for Research on Cancer. pp. 287–288. ISBN 978-92-832-4504-9. Archived from the original on 2022-06-17. Retrieved 2022-07-30.
- 1 2 Howitt, Brooke E.; Nucci, Marissa R. (2019). "1. Uterine mesenchymal lesions". In Zheng, Wenxin; Fadare, Oluwole; Quick, Charles Matthew; Shen, Danhua; Guo, Donghui (eds.). Gynecologic and Obstetric Pathology. Vol. 2. Springer: Springer. pp. 3–6. ISBN 978-981-13-3018-6. Archived from the original on 2022-08-01. Retrieved 2022-07-30.
- ↑ "What is Uterine Sarcoma?". Archived from the original on 2021-09-15. Retrieved 2021-09-17.
- ↑ Li H, et al. (2009). "Gene fusion and RNA trans-splicing in normal and neoplastic cells". Cell Cycle. 8 (2): 218–222. doi:10.4161/cc.8.2.7358. PMID 19158498.
- ↑ Kumar V, Abbas A, Fausto N, Aster J (2010). Robbins and Cotran Pathologic Basis of Disease. 8th edition. Philadelphia: Elsevier Saunders