Esophageal food bolus obstruction
| Esophageal food bolus obstruction | |
|---|---|
| Other names: Steakhouse syndrome[1] | |
.jpg.webp) | |
| Endoscopic image of patient with esophageal food bolus obstruction due to a grape in the setting of eosinophilic esophagitis | |
| Specialty | Emergency medicine, general surgery, gastroenterology |
An esophageal food bolus obstruction is a n obstruction of the esophagus by an swallowed foreign body.
It is usually associated with diseases that may narrow the lumen of the esophagus, such as eosinophilic esophagitis, Schatzki rings, peptic strictures, webs, or cancers of the esophagus; rarely it can be seen in disorders of the movement of the esophagus, such as nutcracker esophagus.
While some esophageal food boli can pass by themselves or with the assistance of medications, many require the use of endoscopy to push the obstructing food into the stomach, or remove. The use of glucagon, while common, has not been found to be useful.[2]
Other names include 'the steakhouse syndrome' and 'backyard barbeque syndrome'.[3]
Signs and symptoms
Many foods can lodge themselves in the esophagus, but the most common are meats such as steak, poultry, or pork[4] leading to the colourful description of the phenomenon as steakhouse syndrome.[1] People with food bolus obstruction typically display acute dysphagia (difficulty swallowing), often to the point that they cannot even swallow their saliva, leading to drooling. They may also experience chest pain, neck pain, regurgitation of food, or painful swallowing (odynophagia).[5]
Patients with esophageal food boluses are also at risk of complications, such as perforation of the esophagus, and aspiration into the lungs. As a result, urgent treatment of patients with high-risk features, or a lengthy duration of symptoms, is recommended.[6]
Risk factors

Food bolus obstruction is most commonly caused by Schatzki rings, which are mucosal rings of unknown cause in the lower esophagus.[1][7] Foodstuff jams into the esophagus due to the narrowing caused by the ring. An increasingly commonly recognized cause for esophageal food bolus obstruction is eosinophilic esophagitis, which is an inflammatory disorder of the mucosa of the esophagus, of unknown cause.[8][9] Many alterations caused by eosinophilic esophagitis can predispose to food boluses; these include the presence of multiple rings and narrowing of the lumen.[10] When considering esophageal dilation to treat a patient with food bolus obstruction, care must be made to look for features of eosinophilic esophagitis, as these patients are at a higher risk of dilation-associated complications.[11]
Other conditions that predispose to food bolus obstructions are esophageal webs, tracheoesophageal fistula/esophageal atresia (TOF/OA) and peptic strictures.[8] Food boluses are common in the course of illness in patients with esophageal cancer but are more difficult to treat as endoscopy to push the bolus is less safe. Patients with esophageal self-expandable metallic stents may present with food boluses lodged within the stent lumen. Rarely disorders of movement of the esophagus, such as nutcracker esophagus, can predispose to food bolus obstruction.[12]
Diagnosis

In terms of the diagnosis of Esophageal food bolus obstruction, the following is done:[13]
- Medical history
- Medical exam
- Chest radiograph
- Computed tomography
Treatment
Conservative
In an emergency room setting, someone with food bolus obstruction may be observed for a period to see if the food bolus passes spontaneously. This may be encouraged by giving carbonated drinks that release gas such as Coca-Cola, which may dislodge the food.[14]
While glucagon has been used in those with esophageal food bolus obstruction, evidence as of 2019 does not support its effectiveness, and its use may result in more side effects.[2] Older reviews considered it an acceptable option as long it does not lead to delays in arranging other treatments.[6][15] Other medications (hyoscine butylbromide, benzodiazepines and opioids) have been studied but the evidence is limited.[14] Hyoscine butylbromide (also known as Buscopan) is used intravenously as a treatment in some cases, although there is a small risk of serious side effects in people who may have underlying cardiac issues such as high blood pressure, tachycardia, or heart disease.[16]
Historical treatment of food bolus obstruction included administration of proteolytic enzymes (such as meat tenderizers) with the purpose of degrading the meat that was blocked; however, it is possible that these methods may increase the risk of perforation of the esophagus.[17] Other modalities rarely used now include removal of boluses using catheters,[18] and the use of large-bore tubes inserted into the esophagus to forcefully lavage it.[19]
Endoscopic
The standard treatment of food bolus obstruction is the use of endoscopy or fibre-optic cameras inserted by mouth into the esophagus.[6] Endoscopes can be used to diagnose the cause of the food bolus obstruction, as well as to remove the obstruction. Traditional endoscopic techniques involved the use of an overtube, a plastic tube inserted into the esophagus prior to the removal of the food bolus, in order to reduce the risk of aspiration into the lungs at the time of endoscopy.[8] However, the "push technique", which involves insufflating air into the esophagus, and gently pushing the bolus toward the stomach instead, has emerged as a common and safe way of removing the obstruction.[8][20]
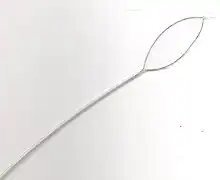
Other tools may be used to remove food boluses. The Roth Net is a mesh net that can be inserted through the endoscope, and opened and closed from the outside; it can be used to retrieve pieces of obstructed food. Snares, which are normally used to remove polyps can be used to macerate the food causing the obstruction. Dormia baskets, which are metal baskets used to remove stones from the common bile duct in a procedure known as endoscopic retrograde cholangiopancreatography, can be opened and closed from the outside in a similar manner to macerate food and facilitate removal. Forceps used for biopsies can also be employed in a similar manner.[20]
References
- 1 2 3 Stadler, J.; A. H. Hölscher; H. Feussner; J. Dittler; J. R. Siewert (December 1989). "The "steakhouse syndrome". Primary and definitive diagnosis and therapy". Surgical Endoscopy. 3 (4): 195–8. doi:10.1007/BF02171545. PMID 2623551. S2CID 6247162.
- 1 2 Peksa, GD; DeMott, JM; Slocum, GW; Burkins, J; Gottlieb, M (April 2019). "Glucagon for Relief of Acute Esophageal Foreign Bodies and Food Impactions: A Systematic Review and Meta-Analysis". Pharmacotherapy. 39 (4): 463–472. doi:10.1002/phar.2236. PMID 30779190. S2CID 73457663.
- ↑ Ginsberg, Gregory G. (February 2007). "Food Bolus Impaction". Gastroenterology & Hepatology. 3 (2): 85–86. ISSN 1554-7914. PMC 3099357. PMID 21960815.
- ↑ Baraka A, Bikhazi G (1975). "Oesophageal foreign bodies". British Medical Journal. 1 (5957): 561–3. doi:10.1136/bmj.1.5957.561. PMC 1672660. PMID 1139150.
- ↑ Nandi P, Ong GB (1978). "Foreign body in the oesophagus: review of 2394 cases". The British Journal of Surgery. 65 (1): 5–9. doi:10.1002/bjs.1800650103. PMID 623968. S2CID 43510040.
- 1 2 3 Ikenberry, Steven O.; Jue, Terry L.; Anderson, Michelle A.; Appalaneni, Vasundhara; Banerjee, Subhas; Ben-Menachem, Tamir; Decker, G. Anton; Fanelli, Robert D.; Fisher, Laurel R.; Fukami, Norio; Harrison, M. Edwyn; Jain, Rajeev; Khan, Khalid M.; Krinsky, Mary Lee; Maple, John T.; Sharaf, Ravi; Strohmeyer, Laura; Dominitz, Jason A. (June 2011). "Management of ingested foreign bodies and food impactions" (PDF). Gastrointestinal Endoscopy. 73 (6): 1085–1091. doi:10.1016/j.gie.2010.11.010. PMID 21628009. Archived (PDF) from the original on 2013-08-08. Retrieved 2022-06-30.
- ↑ Longstreth GF, Longstreth KJ, Yao JF (2001). "Esophageal food impaction: epidemiology and therapy. A retrospective, observational study". Gastrointestinal Endoscopy. 53 (2): 193–8. doi:10.1067/mge.2001.112709. PMID 11174291.
- 1 2 3 4 Kerlin P, Jones D, Remedios M, Campbell C (2007). "Prevalence of eosinophilic esophagitis in adults with food bolus obstruction of the esophagus". Journal of Clinical Gastroenterology. 41 (4): 356–61. doi:10.1097/01.mcg.0000225590.08825.77. PMID 17413601. S2CID 31233220.
- ↑ Cheung KM, Oliver MR, Cameron DJ, Catto-Smith AG, Chow CW (2003). "Esophageal eosinophilia in children with dysphagia". Journal of Pediatric Gastroenterology and Nutrition. 37 (4): 498–503. doi:10.1097/00005176-200310000-00018. PMID 14508223. S2CID 2288806.
- ↑ Cohen MS, Kaufman AB, Palazzo JP, Nevin D, Dimarino AJ, Cohen S (2007). "An audit of endoscopic complications in adult eosinophilic esophagitis". Clinical Gastroenterology and Hepatology. 5 (10): 1149–53. doi:10.1016/j.cgh.2007.05.017. PMID 17683993.
- ↑ Leclercq P, Marting A, Gast P (2007). "Eosinophilic esophagitis". New England Journal of Medicine. 357 (14): 1446, author reply 1446–7. doi:10.1056/NEJMc071646. PMC 2653291. PMID 17914050.
- ↑ Chae HS, Lee TK, Kim YW, et al. (2002). "Two cases of steakhouse syndrome associated with nutcracker esophagus". Diseases of the Esophagus. 15 (4): 330–3. doi:10.1046/j.1442-2050.2002.00271.x. PMID 12472482.
- ↑ Long, Brit; Koyfman, Alex; Gottlieb, Michael (May 2019). "Esophageal Foreign Bodies and Obstruction in the Emergency Department Setting: An Evidence-Based Review". The Journal of Emergency Medicine. 56 (5): 499–511. doi:10.1016/j.jemermed.2019.01.025. ISSN 0736-4679. Archived from the original on 14 March 2022. Retrieved 11 February 2023.
- 1 2 Leopard, D; Fishpool, S; Winter, S (Sep 2011). "The management of oesophageal soft food bolus obstruction: a systematic review". Annals of the Royal College of Surgeons of England. 93 (6): 441–4. doi:10.1308/003588411X588090. PMC 3369328. PMID 21929913.
- ↑ Chauvin, A; Viala, J; Marteau, P; Hermann, P; Dray, X (Jul 2013). "Management and endoscopic techniques for digestive foreign body and food bolus impaction". Digestive and Liver Disease. 45 (7): 529–42. doi:10.1016/j.dld.2012.11.002. PMID 23266207.
- ↑ "Hyoscine butylbromide (Buscopan) injection: risk of serious adverse effects in patients with underlying cardiac disease - GOV.UK". www.gov.uk. Archived from the original on 24 September 2017. Retrieved 16 March 2018.
- ↑ Ko HH, Enns R (October 2008). "Review of food bolus management". Can. J. Gastroenterol. 22 (10): 805–8. doi:10.1155/2008/682082. PMC 2661297. PMID 18925301.
- ↑ Dieter RA, Norbeck DE, Acuna A, Rogers J (1972). "Fogarty catheter removal of cervical esophageal meat bolus. Steak-eater's disease". Archives of Surgery. 105 (5): 790–1. doi:10.1001/archsurg.1972.04180110107028. PMID 5081553.
- ↑ Kozarek RA, Sanowski RA (1980). "Esophageal food impaction: description of a new method for bolus removal". Digestive Diseases and Sciences. 25 (2): 100–3. doi:10.1007/bf01308305. PMID 7353455. S2CID 26808585.
- 1 2 Katsinelos P, Kountouras J, Paroutoglou G, Zavos C, Mimidis K, Chatzimavroudis G (2006). "Endoscopic techniques and management of foreign body ingestion and food bolus impaction in the upper gastrointestinal tract: a retrospective analysis of 139 cases". Journal of Clinical Gastroenterology. 40 (9): 784–9. doi:10.1097/01.mcg.0000225602.25858.2c. PMID 17016132. S2CID 22304230.
External links
| Classification |
|---|