Health in Morocco
Morocco became an independent country in 1956. At that time there were only 400 private practitioners and 300 public health physicians in the entire country. By 1992, the government had thoroughly improved their health care service and quality. Health care was made available to over 70% of the population. Programs and courses to teach health and hygiene have been introduced to inform parents and children on how to correctly care for their own and their families' health.
The first health care policy in Morocco was devised in 1959, with majority of the free healthcare services and management focused on the general public. The State provides funding and administration. The Ministry of Health runs the National Institutes and Laboratories, Basic Care Health Network and the Hospital Network. The Defence Department owns and runs its own hospitals, and local governments run city health services.[1]
The healthcare system is made up of AMO (Mandatory Health Insurance). AMO is split into two sections: CNSS (private)[2] and La CNOPS (public).[3] There is also RAMED, a health insurance program designed to support the low socioeconomic population from financial tragedy due to health related issues.[4]
The Moroccan health care system has four layers, the first being "primary healthcare". This includes clinics, health centres and local hospitals for public healthcare, and infirmaries and medical offices for private healthcare. The second section includes provincial and prefectural hospitals for public health, and specialised clinics and offices for private health. The third area includes hospitals in all major cities, and the fourth includes university hospitals. These centres have the most advanced equipment.
Background
Health care services in Morocco have evolved in line with the country’s epidemiological transition, facilitated by heightened surveillance of health-related conditions and the maturing role carried out by the private sector. Developments have evolved in line with the objectives outlined in the country’s long-term strategy, Vision 2020. Implemented in 2006, the strategy aims at achieving an efficient health care system by 2020. In its 2012-16 phase, reforms have aimed primarily at consolidating past gains but also addressing new needs, with a particular focus on restructuring emergency services, promoting family medicine, developing rural health care, extending national coverage schemes and human resource development.[6]
Health status
Diseases
Morocco has also made significant strides in reducing the prevalence of infectious diseases, and has eradicated polio, trachoma and malaria, thanks to a variety of programmes to raise awareness on how to treat and prevent communicable illnesses, in addition to expanded vaccination campaigns and the introduction of new medicines into the market. Though largely under control, diseases such as hepatitis are still prevalent and efforts are under way to curb the number of affected patients..[6]
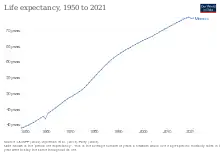
An even greater priority for the sector is non-communicable diseases. According to a recent study conducted by the Ministry of Health (Ministère de la Santé, MS) and the WHO, non-communicable diseases account for 75% of deaths, such as cardiovascular diseases (34%), diabetes (12%) and cancer (11%).[6] Improved longevity – with life expectancy increasing from an average 49.3 years in 1962 to 70.6 in 2012 – and changes in lifestyle and eating habits have meant that such diseases have been on the rise in the past few decades, claiming today three out of every four deaths in Morocco..[6]
Obesity
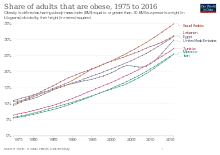
Adolescent girls are at a greater risk of becoming obese.[7] Obesity is linked to a greater availability of food, particularly from the West, and an increasingly sedentary lifestyle in urban areas. A woman who has a low level of schooling or no education in urban areas is significantly more likely to be obese. The general public is not aware of the medical conditions that result from obesity. Rather, female fatness is embraced, as it "is viewed as a sign of social status and is a cultural symbol of beauty, fertility, and prosperity".[7] Being thin is a sign of sickness or poverty.[8]
Maternal and child health care
Maternal health care in particular has improved significantly over the past 10 years, with the maternal mortality ratio dropping from 227 deaths per 100,000 live births to 112, and infant mortality declining from 40 deaths per 1000 live births to 30.2, according to the World Health Organization (WHO). This can in large part be attributed to efforts targeting better access to maternal and child health care services, as well as increased awareness on the necessity to seek medical assistance throughout pregnancy and after. [7] Being thin is a sign of sickness or poverty.[8]
In 2007 the Ministry of Health recognised the problem of maternal and child mortality. This led the ministry to implement the Maternal Mortality Strategy action plan of 2008–12, whose aim was to reduce the maternal mortality rate (MMR) from 227 to 50 deaths per 100,000 births. There were three points of improvement to help them try and achieve their goal. The first was to reduce any barriers preventing women from accessing emergency services. The second was to enhance the health care quality and the third was to improve governance. The Ministry of Health also began the maternal mortality surveillance system. This allowed them to collect and analyse data in 2009 which discovered that the goal of reducing the MMR to 50 would not be achievable by 2015. Because of this information, a new action plan for 2012-16 was introduced to reinforce management and target specific actions for rural and disadvantaged areas.[9]
Nutrition
Over the last 20 years nutrition has significantly changed with rapid changes due to demographic characteristics of the region, speedy urbanisation and social development of steady and significant economic growth. Morocco and the Middle East have the highest amount of excessive dietary energy intake. With a low rate of 4% of poverty prevalence and 19% of child malnutrition, Morocco has an 8% rate of child malnutrition. All these changes have significantly contributed to the dietary and physical activity of individuals living in the Middle East, reflecting changes with nutrition and the prevalence of these changes.[10]
Hospitals


There were 534 hospitals in Morocco in 2020. Only 33 of these hospitals provided tertiary care services in 2020.[11] In 2019, there were 20 inter-regional hospitals, 4 university psychiatry hospitals, 18 regional hospitals, 2 regional psychiatry hospitals, 7 oncology centers, 73 provincial hospitals, 4 provincial psychiatry hospitals, and 31 local hospitals.[12] Hospitals in Morocco include the following:[13]
See also
- The Stethoscope Revolution (Morocco)
- Arabic Wikipedia: Health in Morocco
- List of hospitals in Africa
References
- ↑ World Health Organization (2006). "Health system profile: Morocco" (PDF). Archived from the original (PDF) on 2016-08-03. Retrieved 2016-10-27.
- ↑ National Social Security Fund (2016). "Mandatory health insurance". Archived from the original on 2016-10-28. Retrieved 2016-10-28.
- ↑ Manager of Mandatory Health Insurance (2016). "National fund of social welfare organisations". Archived from the original on 2016-10-15. Retrieved 2016-10-28.
- ↑ Access Health International. "The RAMED project". Archived from the original on 2016-10-28. Retrieved 2016-10-28.
- ↑ Setayash, Hamidreza (2016). "Populations Reference Bureau". HIV in the Middle East: Low Prevalence but Not Low risk. Archived from the original on 2016-05-06. Retrieved 2016-05-11.
- 1 2 3 4 "Access to health care broadens in Morocco". Oxford Business Group. Archived from the original on 19 January 2021. Retrieved 11 July 2020.
- 1 2 3 Mokhtar, Najat; et al. (2001). Diet Culture and Obesity in North Africa.
- 1 2 Rguibi & R Belahsen, M. (2006). Fattening Practices Among Moroccan Saharawi Women.
- ↑ "Actions on social determinants and interventions in primary health to improve mother and child health and health equity in morocco". International Journal for Equity in Health. 15.
- ↑ Osman, Gala (2016). "Nutrition-health related patterns in the Middle East". Asian Pacific Journal of Clinical Nutrition. Archived from the original on January 19, 2021. Retrieved January 1, 2016.
- ↑ "Moroccan Hospital & Medical Installed Base Mapping Report 2020". Business Wire. June 19, 2020. Archived from the original on January 11, 2021. Retrieved January 8, 2021.
- ↑ "2019 Healthcare Sheet". Moroccan Ministry of Health. 2019. Retrieved January 19, 2021.
- ↑ "Hospitals in Morocco" (Map). Google Maps. Archived from the original on January 19, 2021. Retrieved January 18, 2021.
- 1 2 3 4 5 6 7 8 9 10 "Medical Assistance". US Embassy, Morocco. Archived from the original on December 6, 2020. Retrieved January 18, 2021.
- ↑ "CHU Cheikh Zaid (Oujda) Hospital". CHU Oujda. Archived from the original on 2020-02-25. Retrieved 2020-02-25.
- ↑ "CHU Hassan II (Fes) Hospital". CHU Hassan. Archived from the original on 2020-02-25. Retrieved 2020-02-25.
- 1 2 "Morocco expands hospital services with US$8 million OPEC Fund loan". The OPEC Fund for International Development. 9 February 2001. Retrieved 19 October 2012.
- ↑ "CHU Ibn-Roch Hospital". CHU Ibn-Rochd Hospital. Archived from the original on 2020-02-03. Retrieved 2020-02-25.
- ↑ "CHU Mohamed V (Rabat) Hospital". CHIS Rabat. Archived from the original on 2017-05-19. Retrieved 2021-01-19.
- ↑ "CHU Mohammed VI (Marrakesh) Hospital". CHU Marrakesh Hospital. Archived from the original on 2020-01-14. Retrieved 2020-02-25.
- ↑ "Morocco's Largest Private Hospital Opens to Public". HospiMedica. Archived from the original on January 19, 2021. Retrieved January 8, 2021.
External links
- World Health Organization (WHO): Morocco
- The State of the World's Midwifery - Morocco country profile
