In-water recompression
In-water recompression (IWR) or underwater oxygen treatment is the emergency treatment of decompression sickness (DCS) by returning the diver underwater to help the gas bubbles in the tissues, which are causing the symptoms, to resolve. It is a procedure that exposes the diver to significant risk which should be compared with the risk associated with the available options. Some authorities recommend that it is only to be used when the time to travel to the nearest recompression chamber is too long to save the victim's life, others take a more pragmatic approach, and accept that in some circumstances IWR is the best available option.[1][2] The risks may not be justified for case of mild symptoms likely to resolve spontaneously, or for cases where the diver is likely to be unsafe in the water, but in-water recompression may be justified in cases where severe outcomes are likely, if conducted by a competent and suitably equipped team.[3]
Carrying out in-water recompression when there is a nearby recompression chamber or without suitable equipment and training is never a desirable option.[1][2] The risk of the procedure is due to the diver suffering from DCS being seriously ill and may become paralysed, unconscious or stop breathing while under water. Any one of these events is likely to result in the diver drowning or asphyxiating or suffering further injury during a subsequent rescue to the surface. This risk can be reduced by improving airway security by using surface supplied gas and a helmet or full-face mask.[3]
Several schedules have been published for in-water recompression treatment, but little data on their efficacy is available.[3]
Background
Treatment of DCS utilizing the US Navy Treatment Table 6 with oxygen at 18m or an equivalent alternative is a widely recognised standard of care.[4][5][6][7] Ideally, treatment should take place in a chamber where there is no risk of drowning or hypothermia, and other medical problems can be managed conveniently. Significant delay to treatment, difficult transport, and facilities with limited experience may lead to consideration of on site treatment.[8] Surface oxygen for first aid has been proven to improve the efficacy of recompression and decreased the number of recompression treatments required when administered within four hours post dive.[9] IWR to 9 m breathing oxygen is one option that has shown success over the years[2][10][11] IWR is not without risk and should be undertaken with certain precautions.[1][2][12][13] IWR would only be suitable for an organised and disciplined group of divers with suitable equipment and practical training in the procedure.[1][2][3]
The principle behind IWR treatment is the same as that behind the treatment of DCS in a recompression chamber:[1][2] an increase in ambient pressure will reduce the volume of the bubbles allowing better blood transport downstream of the bubbles. If the casualty can breathe pure oxygen further improvements will occur because the increase in the proportion of oxygen in the blood may keep previously oxygen-starved tissues alive and the oxygen window will accelerate the removal of inert gases from the bubbles making the bubbles smaller. The unacceptable risks of oxygen toxicity convulsions can be reduced by recompressing to lower pressures and for shorter durations than otherwise preferred.[3]
The use of in-water oxygen at 6 meters has been shown to reduce bubble loads in divers compared to divers breathing oxygen on the surface.[14]
Brief history and risks
The Royal Australian Navy School of Underwater Medicine was charged to supervise the then non-sanctioned practice of IWR.[13][15] This charge was in response to the very long delays that were associated between the presentation of DCS and recompression treatment. Dr Edmonds also described the debates about underwater oxygen treatment for DCS that are not unlike current concerns. The issues include:
- Inappropriate cases for treatment,
- Oxygen toxicity,
- Emergency termination of treatment,
- Hypothermia
- Adequacy of equipment in remote areas,
- Seasickness,
- Operator expertise and training,
- Safety of the diving attendant and the boat tenders,
- Requirement for medical supervision,
- Transport availability,
- Misuse of equipment,
- Pulmonary barotrauma cases.
In 2018, a group of diving medical experts issued a consensus guideline on pre-hospital decompression sickness management and concluded that IWR is only appropriate in groups that have been trained in IWR techniques.[16]
Equipment
Some of the equipment needed includes:[1][2][3]
- a means of securely holding the casualty at a measured depth, such as a harness and 20 metre line with a 20 kg lead weight at the bottom and 40 litre buoy at the top
- a means of allowing the casualty to ascend slowly, such as loops in the line to which the harness could be clipped
- full face diving masks for the casualty and for an in-water tending diver including two-way communication to the surface and an umbilical gas supply
- surface supplied breathing gases including pure oxygen and air delivered to the casualty by umbilical
- voice communications equipment to the divers
- use IWR treatment "table"
In-water recompression tables
Six IWR treatment tables have been published in the scientific literature. Each of these methods have several commonalities including the use of a full face mask, a tender to supervise the diver during treatment, a weighted recompression line and a means of communication. The history of the three older methods for providing oxygen at 9 msw (30 fsw) was described in great detail by Drs. Pyle and Youngblood.[2] The fourth method for providing oxygen at 7.5 msw (25 fsw) was described by Richard Pyle at the 48th Annual UHMS Workshop on In-water Recompression in 1999.[1] The Clipperton method involves recompression to 9 msw (30 fsw) while the Clipperton(a) rebreather method involves a recompression to 30 msw (98 fsw).[17]
Australian in-water recompression table
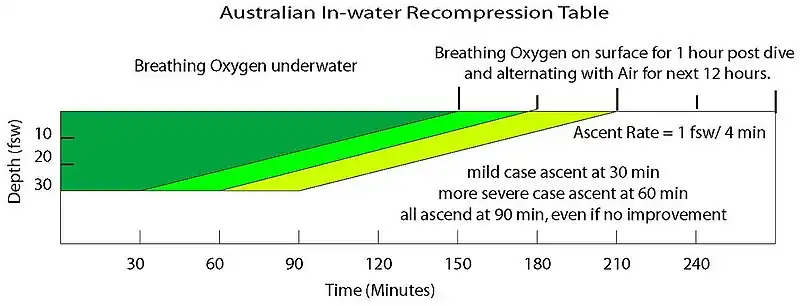
The Australian IWR Tables were developed by the Royal Australian Navy in the 1960s in response to their need for treatment in remote locations far away from recompression chambers. It was the shallow portion of the table developed for recompression chamber use.[13][15]
Oxygen is breathed the entire portion of the treatment without any air breaks and is followed by alternating periods (12 hours) of oxygen and air breathing on the surface.
Clipperton in-water recompression tables
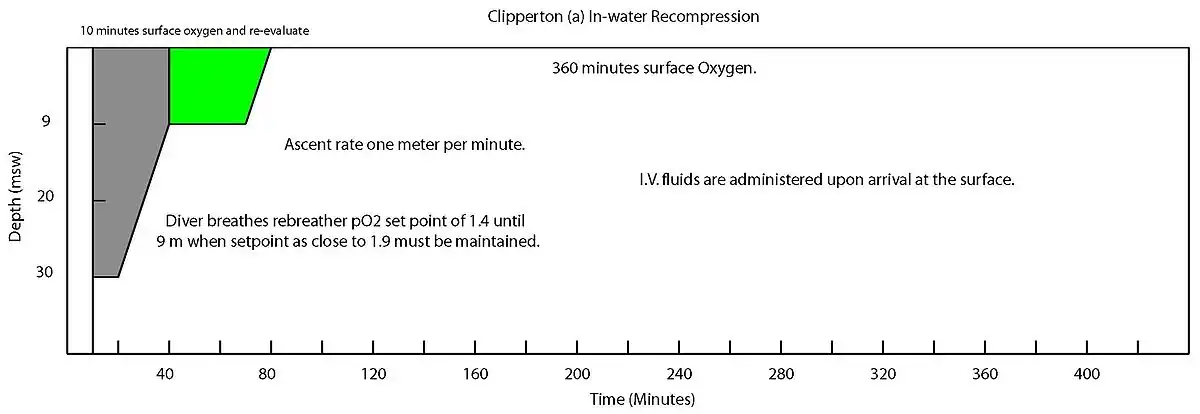
The Clipperton and Clipperton(a) methods were developed for use on a scientific mission to the atoll of Clipperton, 1,300 km from the Mexican coasts.[17] The two versions are based on the equipment available for treatment with the Clipperton(a) table being designed for use with rebreathers.
Both methods begin with 10 minutes of surface oxygen. For the Clipperton IWR table, oxygen is then breathed the entire portion of the treatment without any air breaks. For the Clipperton IWR table, descent is made to the initial treatment depth maintaining a partial pressure of 1.4 ATA. Oxygen breathing on the surface for 6 hours post treatment and intravenous fluids are also administered following both treatment tables.
Hawaiian in-water recompression table

The Hawaiian IWR table was first described by Farm et al. while studying the diving habits of Hawaii's diving fishermen.[11]
The initial portion of the treatment involves descent on air to the depth of relief plus 30 fsw or a maximum of 165 fsw for ten minutes. Ascent from initial treatment depth to 30 fsw occurs over 10 minutes. The diver then completes the treatment breathing oxygen and is followed by oxygen breathing on the surface for 30 minutes post treatment.
The Hawaiian IWR Table with Pyle modifications can be found in the proceedings of the DAN 2008 Technical Diving Conference.
Pyle in-water recompression table
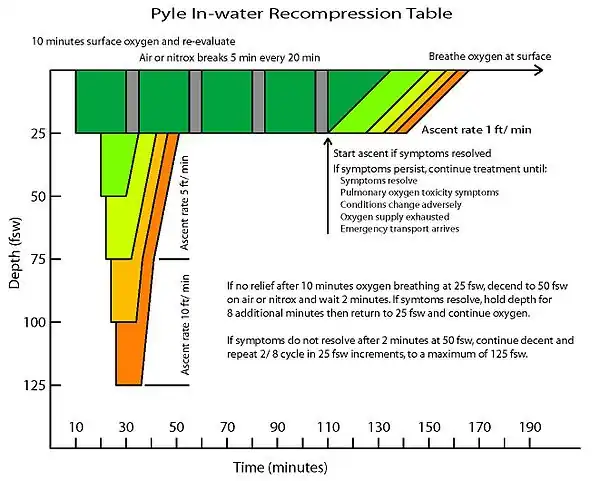
The Pyle IWR table was developed by Dr. Richard Pyle as a method for treating DCS in the field following scientific dives.[2]
This method begins with a 10-minute surface oxygen evaluation period. Compression to 25 fsw on oxygen for another 10-minute evaluation period. The table is best described by the treatment algorithm (Pyle IWR algorithm). This table does include alternating air breathing periods or "air breaks".
US Navy in-water recompression tables
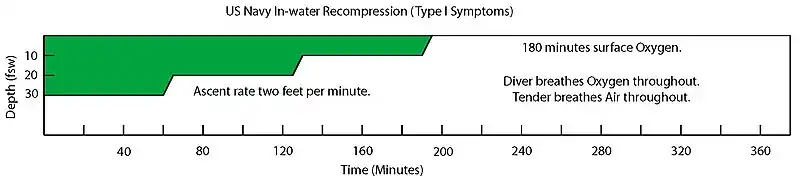
The US Navy developed two IWR treatment tables.[6] The table used depends on the symptoms diagnosed by the medical officer.
Oxygen is breathed the entire portion of the treatment without any air breaks and is followed by 3 hours of oxygen breathing on the surface.
Factors influencing a decision to use IWR
The decision of whether or not to attempt IWR is dependent on identifying the diver whose condition is serious enough to justify the risk, but whose clinical condition does not indicate that the risk is unacceptable. The risk may not be justified for mild DCI, if spontaneous recovery is probable whether the diver is recompressed or not, and surface oxygen is indicated for these cases. However, in these cases the risk of the recompression is also low, and early abandonment is also unlikely to cause further harm.[3]
The International Association of Nitrox and Technical Divers, in consultation with diving medical experts, has produced a decision map for field use by divers without medical training, but with training in the recommended procedures for IWR. Their application relies on history or gross observation alone, without a detailed neurological assessment.[3]
Contraindications
Some signs of decompression illness which suggest a risk of permanent injury are nevertheless considered contraindications for IWR. Hearing loss and vertigo displayed in isolation with no other symptoms of DCI can have been caused by inner ear barotrauma rather than DCI, and inner ear barotrauma is generally considered a contraindication for recompression. Even when caused by DCI, vertigo can make in-water treatment hazardous if accompanied by nausea and vomiting. A diver with a deteriorating level of consciousness or with a persisting reduced level of consciousness should also not be recompressed in-water nor should a diver who does not want to go back down, or with a history of oxygen toxicity in the preceding dives, or any physical injury or incapacitation which may make the procedure unsafe.[3]
"Informal" in-water recompression
Although in-water recompression is widely regarded as risky, and to be avoided, there is increasing evidence that technical divers who surface and demonstrate mild DCS symptoms may often get back into the water and breathe pure oxygen at a depth 20 feet/6 meters for a period of time to seek to alleviate the symptoms. This trend is noted in paragraph 3.6.5 of DAN's 2008 accident report.[18] The report also notes that whilst the reported incidents showed very little success, "[w]e must recognize that these calls were mostly because the attempted IWR failed. In case the IWR were successful, [the] diver would not have called to report the event. Thus we do not know how often IWR may have been used successfully."
See also
- Decompression practice – Techniques and procedures for safe decompression of divers
- Decompression (diving) – Adjusting to pressure changes in ascents
- Decompression sickness – Disorder caused by dissolved gases emerging from solution
- Hyperbaric treatment schedules – Planned sequences of hyperbaric pressure exposure using a specified breathing gas as medical treatment
References
- 1 2 3 4 5 6 7 Kay, E.; Spencer, M. P. (1999). In water recompression. 48th Undersea and Hyperbaric Medical Society Workshop. Vol. UHMS Publication Number RC103.C3. United States: Undersea and Hyperbaric Medical Society. p. 108. Archived from the original on 7 October 2008. Retrieved 8 June 2008.
- 1 2 3 4 5 6 7 8 9 Pyle, R. L.; Youngblood, D. A. (1995). "In-water Recompression as an emergency field treatment of decompression illness". AquaCorp. 11. Archived from the original on 20 August 2009. Retrieved 8 June 2008.
- 1 2 3 4 5 6 7 8 9 Doolette, D. J.; Mitchell, S. J. (June 2018). "In-water recompression". Diving Hyperb Med. 48 (2): 84–95. doi:10.28920/dhm48.2.84-95. PMC 6156824. PMID 29888380.
- ↑ Moon, R. E. (2000). "Recompression treatments should be to a pressure equivalent to 18 m depth. (Part 2 of 5 part Pro Con Debate)". South Pacific Underwater Medicine Society Journal. 30 (3). ISSN 0813-1988. OCLC 16986801. Retrieved 8 June 2008.
- ↑ Berghage, T. E.; Vorosmarti Jr, J.; Barnard, E. E. P. (1978). Recompression treatment tables used throughout the world by government and industry. US Naval Medical Research Center Technical Report (Report). Vol. NMRI-78-16. Archived from the original on 5 August 2009. Retrieved 8 June 2008.
- 1 2 US Navy Diving Manual, 6th revision. Washington, DC: US Naval Sea Systems Command. 2006. Retrieved 8 June 2008.
- ↑ Yarbrough, O. D.; Behnke, Albert R. (1939). "The treatment of compressed air illness using oxygen". J Ind Hyg Toxicol. 21: 213–218. ISSN 0095-9030.
- ↑ Brubakk, A. O. (2000). "On-site recompression treatment is acceptable for DCI. (Part 5 of 5 part Pro Con Debate)". South Pacific Underwater Medicine Society Journal. 30 (3). ISSN 0813-1988. OCLC 16986801. Retrieved 8 June 2008.
- ↑ Longphre, J. M.; DeNoble, P. J.; Moon, R. E.; Vann, R. D.; Freiberger, J. J. (2007). "First aid normobaric oxygen for the treatment of recreational diving injuries". Undersea and Hyperbaric Medicine. 34 (1): 43–9. ISSN 1066-2936. OCLC 26915585. PMID 17393938. Archived from the original on 13 June 2008. Retrieved 8 June 2008.
- ↑ Pyle, R. L. (1997). "In-water Recompression (Letter to Editor)". South Pacific Underwater Medicine Society Journal. 27 (3). ISSN 0813-1988. OCLC 16986801. Retrieved 8 June 2008.
- 1 2 Farm; Hayashi; Beckman (1986). Diving and decompression sickness treatment practices among Hawaii's diving fishermen (PDF). Sea Grant Technical Report (Report). Vol. UNIHI-TP-86-01. Retrieved 8 June 2008.
- ↑ Knight, J. (1984). "In-water oxygen recompression therapy for decompression sickness". South Pacific Underwater Medicine Society Journal. 14 (3). ISSN 0813-1988. OCLC 16986801.
- 1 2 3 Edmonds, C. (1979). "Underwater oxygen treatment of decompression sickness". South Pacific Underwater Medicine Society Journal. 9 (1). ISSN 0813-1988. OCLC 16986801. Retrieved 8 June 2008.
- ↑ Blatteau, J. E.; Pontier, J. M. (July 2009). "Effect of in-water recompression with oxygen to 6 msw versus normobaric oxygen breathing on bubble formation in divers". European Journal of Applied Physiology. 106 (5): 691–5. doi:10.1007/s00421-009-1065-y. PMID 19424716. S2CID 15838039.
- 1 2 Edmonds, C. (1995). "Underwater oxygen for treatment of decompression sickness: A review". South Pacific Underwater Medicine Society Journal. 25 (3). ISSN 0813-1988. OCLC 16986801. Archived from the original on 22 August 2009. Retrieved 8 June 2008.
- ↑ Mitchell SJ, Bennett MH, Bryson P, Butler FK, Doolette DJ, Holm JR, Kot J, Lafère P (March 2018). "Pre-hospital management of decompression illness: expert review of key principles and controversies". Diving Hyperb Med. 48 (1): 45–55. doi:10.28920/dhm48.1.45-55. PMC 6467826. PMID 29557102. Retrieved 2018-06-05.
- 1 2 Blatteau JE; Jean, F.; Pontier, J. M.; Blanche, E.; Bompar, J.; Meaudre, E.; Etienne, J. (August 2006). "[Decompression sickness accident management in remote areas. Use of immediate IWR therapy. Review and elaboration of a new protocol targeted for a mission at Clipperton atoll]". Ann Fr Anesth Reanim (in French). 25 (8): 874–83. doi:10.1016/j.annfar.2006.04.007. PMID 16860525.
- ↑ "Annual Diving Report:2008 edition" (PDF). Divers Alert Network. Retrieved 1 September 2009.
Further reading
- Mitchell SJ, Doolette DJ, Wachholz CJ, Vann RD (2005). Management of Mild or Marginal Decompression Illness in Remote Locations Workshop Proceedings. United States: Divers Alert Network. p. 240. Retrieved 2008-06-08.
- Elliott, D. (1997). "Treatment of decompression illness following mixed gas recreational dives". South Pacific Underwater Medicine Society Journal. 27 (2). ISSN 0813-1988. OCLC 16986801. Retrieved 2008-06-08.
- Gold D, Geater A, Aiyarak S, Juengprasert W, Chuchaisangrat B, Samakkaran A (1999). "The indigenous fisherman divers of Thailand: in-water recompression". Int Marit Health. 50 (1–4): 39–48. PMID 10970270.