Lingual nerve
| Lingual nerve | |
|---|---|
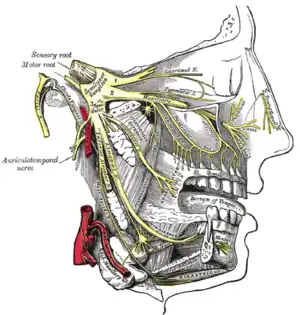 Distribution of the maxillary and mandibular nerves, and the submaxillary ganglion. | |
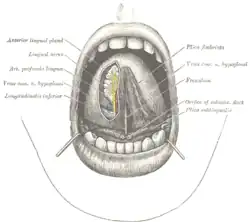 The mouth cavity. The apex of the tongue is turned upward, and on the right side a superficial dissection of its under surface has been made. | |
| Details | |
| From | mandibular nerve |
| Innervates | tongue |
| Identifiers | |
| Latin | nervus lingualis |
| MeSH | D008036 |
| TA98 | A14.2.01.081 |
| TA2 | 6267 |
| FMA | 53218 |
| Anatomical terms of neuroanatomy | |
The lingual nerve carries sensory innervation from the anterior two-thirds of the tongue. It contains fibres from both the mandibular division of the trigeminal nerve (CN V3) and from the facial nerve (CN VII). The fibres from the trigeminal nerve are for touch, pain and temperature (general sensation), and the ones from the facial nerve are for taste (special sensation).
Structure
The lingual nerve lies at first beneath the lateral pterygoid muscle, medial to and in front of the inferior alveolar nerve, and is occasionally joined to this nerve by a branch which may cross the internal maxillary artery.
The chorda tympani (a branch of the facial nerve, CN VII) joins it at an acute angle here, carrying taste fibers from the anterior two-thirds of the tongue and parasympathetic fibers to the submandibular ganglion.
The nerve then passes between the medial pterygoid muscle and the ramus of the mandible, and crosses obliquely to the side of the tongue beneath the constrictor pharyngis superior and styloglossus, and then between the hyoglossus and deep part of the submandibular gland; it finally runs from laterally to medially inferiorly crossing the duct of the submandibular gland, and along the tongue to its tip becoming the sublingual nerve, lying immediately beneath the mucous membrane.
A well known rhyme has been used by anatomy students for many years to remember some features of the lingual nerve anatomy mentioned above: "The Lingual Nerve, Describes a Curve, Across the Hyoglossus...
Function
The lingual nerve supplies general somatic afferent innervation from the mucous membrane of the anterior two-thirds (body) of the tongue, while the posterior one-third (root) is innervated by the glossopharyngeal. It also carries nerve fibers that are not part of the trigeminal nerve, including the chorda tympani nerve of the facial nerve, which provides special sensation (taste) to the anterior 2/3 part of the tongue as well as parasympathetic and sympathetic fibers.
The submandibular ganglion is suspended by two nerve filaments from the lingual nerve.
Clinical significance
Lingual nerve injuries
The most common cause of lingual nerve injuries is third molar (wisdom tooth) surgery, less commonly the lingual nerve can be injured by local anaesthetic dental injections (particularly inferior dental block injections) and sublingual or submandibular surgery.[1]
Any injury to sensory nerves can result in pain, altered sensation and/or numbness, but usually a combination of all three symptoms arises. This can have a significant negative effect on the patient's quality of life affecting their daily function and psychological health.[2]
Patients should be routinely warned about lingual nerve injuries prior to wisdom tooth and floor of mouth surgery. The risk associated with wisdom tooth surgery is commonly accepted to be 2% temporary and 0.2% permanent.[3]
Warning patients of nerve injury prior to administration of deep dental injections has a risk of injury in approximately 1:14,000 with 25% of these remaining persistent. Preoperative warning about these injuries is routinely undertaken in the US and Germany. This reflects good practice recommended by the Royal College of Anaesthetists (prior warning of potential nerve injury in relation to spinal and epidural blocks 1 on 24–57,000 risk)[4] and NHS patient.uk.com.[5]
Infiltration dentistry is a technique that may reduce the possibility of lingual nerve injuries by avoiding deep injections.[6]
Avoiding lingual access when undertaking wisdom tooth surgery will also avoid unnecessary lingual nerve injury[7][8][9]
See also
Additional images
 Mandible of human embryo 24 mm. long. Outer aspect.
Mandible of human embryo 24 mm. long. Outer aspect.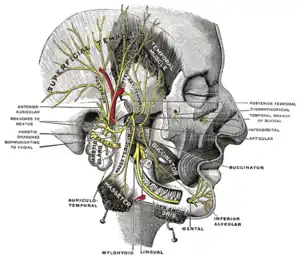 Mandibular division of the trifacial nerve.
Mandibular division of the trifacial nerve.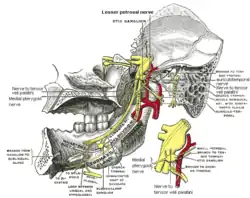 Mandibular division of trifacial nerve, seen from the middle line.
Mandibular division of trifacial nerve, seen from the middle line. Plan of the facial and intermediate nerves and their communication with other nerves.
Plan of the facial and intermediate nerves and their communication with other nerves. Hypoglossal nerve, cervical plexus, and their branches.
Hypoglossal nerve, cervical plexus, and their branches. Sympathetic connections of the submaxillary and superior cervical ganglia.
Sympathetic connections of the submaxillary and superior cervical ganglia. Lingual nerve
Lingual nerve Lingual nerve
Lingual nerve Mandibular nerve and bone. Deep dissection. Anterior view.
Mandibular nerve and bone. Deep dissection. Anterior view. Infratemporal fossa. Lingual and inferior alveolar nerve. Deep dissection. Anterolateral view
Infratemporal fossa. Lingual and inferior alveolar nerve. Deep dissection. Anterolateral view
References
![]() This article incorporates text in the public domain from page 895 of the 20th edition of Gray's Anatomy (1918)
This article incorporates text in the public domain from page 895 of the 20th edition of Gray's Anatomy (1918)
- ↑ Br Dent J. 2013 Oct;215(8):393-9. doi: 10.1038/sj.bdj.2013.993.
- ↑ http://www.quintpub.com/userhome/jop/jop_25_4_Renton_7.pdf%5B%5D
- ↑ sitecore\lewis.ashman@rcseng.ac.uk. "Recovering from Surgery — Royal College of Surgeons". Royal College of Surgeons. Retrieved 20 April 2018.
- ↑ "Archived copy" (PDF). Archived from the original (PDF) on 2014-04-16. Retrieved 2014-04-15.
{{cite web}}: CS1 maint: archived copy as title (link) - ↑ "Anaesthesia (UK) - Local and General anaesthesia information - Patient". Patient.
- ↑ J Am Dent Assoc. 2011 Sep;142 Suppl 3:19S-24S. The use of the mandibular infiltration anesthetic technique in adults. Meechan JG.
- ↑ J Oral Maxillofac Surg. 1995 Oct;53(10):1178-81. The relationship of the lingual nerve to the mandibular third molar region: an anatomic study. Pogrel MA1, Renaut A, Schmidt B, Ammar A.
- ↑ Br Dent J. 1996 Jun 22;180(12):456-61. Lingual nerve damage during lower third molar removal: a comparison of two surgical methods. Robinson PP1, Smith KG
- ↑ Eur J Dent Educ. 1999 May;3(2):52-5.The effect of surgical technique on lingual nerve damage during lower 3rd molar removal by dental students.Robinson PP, Loescher AR, Smith KG.
External links
- Anatomy figure: 27:03-05 at Human Anatomy Online, SUNY Downstate Medical Center
- MedEd at Loyola GrossAnatomy/h_n/cn/cn1/cnb3.htm
- lesson4 at The Anatomy Lesson by Wesley Norman (Georgetown University) (mandibularnerve)
- cranialnerves at The Anatomy Lesson by Wesley Norman (Georgetown University) (V)
- "Anatomy diagram: 05287.011-1". Roche Lexicon - illustrated navigator. Elsevier. Archived from the original on 2013-04-22.