MHealth

mHealth (also written as m-health or mhealth) is an abbreviation for mobile health, a term used for the practice of medicine and public health supported by mobile devices.[1] The term is most commonly used in reference to using mobile communication devices, such as mobile phones, tablet computers and personal digital assistants (PDAs), and wearable devices such as smart watches, for health services, information, and data collection.[2] The mHealth field has emerged as a sub-segment of eHealth, the use of information and communication technology (ICT), such as computers, mobile phones, communications satellite, patient monitors, etc., for health services and information.[3] mHealth applications include the use of mobile devices in collecting community and clinical health data, delivery/sharing of healthcare information for practitioners, researchers and patients, real-time monitoring of patient vital signs, the direct provision of care (via mobile telemedicine) as well as training and collaboration of health workers.[4][5]
While mHealth has application for industrialized nations, the field has emerged in recent years as largely an application for developing countries, stemming from the rapid rise of mobile phone penetration in low-income nations. The field, then, largely emerges as a means of providing greater access to larger segments of a population in developing countries, as well as improving the capacity of health systems in such countries to provide quality healthcare.[6] Within the mHealth space, projects operate with a variety of objectives, including increased access to healthcare and health-related information (particularly for hard-to-reach populations); improved ability to diagnose and track diseases; timelier, more actionable public health information; and expanded access to ongoing medical education and training for health workers.[3][7]
Definitions

mHealth broadly encompasses the use of mobile telecommunication and multimedia technologies as they are integrated within increasingly mobile and wireless health care delivery systems. The field broadly encompasses the use of mobile telecommunication and multimedia technologies in health care delivery. The term mHealth was coined by Robert Istepanian as use of "emerging mobile communications and network technologies for healthcare".[8] A definition used at the 2010 mHealth Summit of the Foundation for the National Institutes of Health (FNIH) was "the delivery of healthcare services via mobile communication devices".[9] The GSM Association representing the worldwide mobile communications industry published a report on mHealth in 2010 describing a new vision for healthcare and identified ways in which mobile technology might play a role in innovating healthcare delivery systems and healthcare system cost management.[10]
While there are some projects that are considered solely within the field of mHealth, the linkage between mHealth and eHealth is unquestionable. For example, an mHealth project that uses mobile phones to access data on HIV/AIDS rates would require an eHealth system in order to manage, store, and assess the data. Thus, eHealth projects many times operate as the backbone of mHealth projects.[3]
In a similar vein, while not clearly bifurcated by such a definition, eHealth can largely be viewed as technology that supports the functions and delivery of healthcare, while mHealth rests largely on providing healthcare access.[9] Because mHealth is by definition based on mobile technology such as smartphones, healthcare, through information and delivery, can better reach areas, people, and/or healthcare practitioners with previously limited exposure to certain aspects of healthcare.
Medical uses
mHealth apps are designed to support diagnostic procedures, to aid physician decision-making for treatments, and to advance disease-related education for physicians and people under treatment.[11] Mobile health has much potential in medicine and, if used in conjunction with human factors may improve access to care, the scope, and quality of health care services that can be provided. Some applications of mobile health may also improve the ability to improve accountability in healthcare and improve continuum of care by connecting interdisciplinary team members.[12]
mHealth is one aspect of eHealth that is pushing the limits of how to acquire, transport, store, process, and secure the raw and processed data to deliver meaningful results. mHealth offers the ability of remote individuals to participate in the health care value matrix, which may not have been possible in the past. Participation does not imply just consumption of health care services. In many cases remote users are valuable contributors to gather data regarding disease and public health concerns such as outdoor pollution, drugs and violence.
While others exist, the 2009 UN Foundation and Vodafone Foundation[3] report presents seven application categories within the mHealth field:[6]
- Education and awareness
- Helpline
- Diagnostic and treatment support
- Communication and training for healthcare workers
- Disease and epidemic outbreak tracking
- Remote monitoring
- Remote data collection
Education and awareness
Education and awareness programs within the mHealth field are largely about the spreading of mass information from source to recipient through short message services (SMS). In education and awareness applications, SMS messages are sent directly to users' phones to offer information about various subjects, including testing and treatment methods, availability of health services, and disease management. SMSs provide an advantage of being relatively unobtrusive, offering patients confidentiality in environments where disease (especially HIV/AIDS) is often taboo. Additionally, SMSs provide an avenue to reach far-reaching areas—such as rural areas—which may have limited access to public health information and education, health clinics, and a deficit of healthcare workers.[3][7]
Helpline
Helpline typically consists of a specific phone number that any individual is able to call to gain access to a range of medical services. These include phone consultations, counseling, service complaints, and information on facilities, drugs, equipment, and/or available mobile health clinics.[3]
Diagnostic support, treatment support, communication and training for healthcare workers
Diagnostic and treatment support systems are typically designed to provide healthcare workers in remote areas advice about diagnosis and treatment of patients. While some projects may provide mobile phone applications—such as a step-by-step medical decision tree systems—to help healthcare workers diagnose, other projects provide direct diagnosis to patients themselves. In such cases, known as telemedicine, patients might take a photograph of a wound or illness and allow a remote physician to diagnose to help treat the medical problem. Both diagnosis and treatment support projects attempt to mitigate the cost and time of travel for patients located in remote areas.[3]
mHealth projects within the communication and training for healthcare workers subset involve connecting healthcare workers to sources of information through their mobile phone. This involves connecting healthcare workers to other healthcare workers, medical institutions, ministries of health, or other houses of medical information. Such projects additionally involve using mobile phones to better organize and target in-person training. Improved communication projects attempt to increase knowledge transfer amongst healthcare workers and improve patient outcomes through such programs as patient referral processes.[3] For example, the systematic use of mobile instant messaging for the training and empowerment of health professionals has resulted in higher levels of clinical knowledge and fewer feelings of professional isolation.[13]
Disease surveillance, remote data collection, and epidemic outbreak tracking
Projects within this area operate to utilize mobile phones' ability to collect and transmit data quickly, cheaply, and relatively efficiently. Data concerning the location and levels of specific diseases (such as malaria, HIV/AIDS, TB, Avian Flu) can help medical systems or ministries of health or other organizations identify outbreaks and better target medical resources to areas of greatest need. Such projects can be particularly useful during emergencies, in order to identify where the greatest medical needs are within a country[3]
Policymakers and health providers at the national, district, and community level need accurate data in order to gauge the effectiveness of existing policies and programs and shape new ones. In the developing world, collecting field information is particularly difficult since many segments of the population are rarely able to visit a hospital, even in the case of severe illness. A lack of patient data creates an arduous environment in which policy makers can decide where and how to spend their (sometimes limited) resources. While some software within this area is specific to a particular content or area, other software can be adapted to any data collection purpose.
Treatment support and medication compliance for patients, including chronic disease management
Remote monitoring and treatment support allows for greater involvement in the continued care of patients. Recent studies seem to show also the efficacy of inducing positive and negative affective states, using smart phones.[2] Within environments of limited resources and beds—and subsequently a 'outpatient' culture—remote monitoring allows healthcare workers to better track patient conditions, medication regimen adherence, and follow-up scheduling. Such projects can operate through either one- or two-way communications systems. Remote monitoring has been used particularly in the area of medication adherence for AIDS,[14][15] cardiovascular disease,[16][17] chronic lung disease,[17] diabetes,[18][3][19] antenatal mental health,[20] mild anxiety,[21] and tuberculosis.[14] Technical process evaluations have confirmed the feasibility of deploying dynamically tailored, SMS-based interventions designed to provide ongoing behavioral reinforcement for persons living with HIV.[22] among others.
In conclusion, the use of mobile phone technology (in combination with a web-based interface) in health care results in an increase in convenience and efficiency of data collection, transfer, storage and analysis management of data as compared with paper-based systems. Formal studies and preliminary project assessments demonstrate this improvement of efficiency of healthcare delivery by mobile technology.[23] Nevertheless, mHealth should not be considered as a panacea for healthcare.[24] Possible organizational issues include the ensuring of appropriate use and proper care of the handset, lost or stolen phones, and the important consideration of costs related to the purchase of equipment. There is therefore a difficulty in comparison in weighing up mHealth interventions against other priority and evidence-based interventions.[25]
Criticism and concerns
The extensive practice of mhealth research has sparked criticism, for example on the proliferation of fragmented pilot studies in low- and middle-income countries, which is also referred to as "pilotitis."[26] The extent of un-coordinated pilot studies prompted for instance the Ugandan Director General Health Services Dr Jane Ruth Aceng in 2012 to issue a notice that, "in order to jointly ensure that all eHealth efforts are harmonized and coordinated, I am directing that ALL eHealth projects/Initiatives be put to halt."[27] The assumptions that justify mhealth initiatives have also been challenged in recent sociological research. For example, mobile phones have been argued to be less widely accessible and usable than is often portrayed in mhealth-related publications;[28] people integrate mobile phones into their health behavior without external intervention;[29] and the spread of mobile phones in low- and middle-income countries itself can create new forms of digital and healthcare exclusion, which mhealth interventions (using mobile phones as a platform) cannot overcome and potentially accentuate.[30] Mhealth has also been argued to alter the practice of healthcare and patient-physician relationships as well as how bodies and health are being represented.[31][32] Another widespread concern relates to privacy and data protection, for example in the context of electronic health records.[32][33]
Studies looking into the perceptions and experiences of primary healthcare professionals using mheath have found that most health care professionals appreciated being connected to their colleagues, however some prefer face to face communication.[12] Some healthcare workers also felt that while reporting was improved and team members who require help or training could be more easily identified, some healthcare professionals did not feel comfortable being monitored continuously.[12] A proportion of healthcare professionals prefer paper reporting.[12] The use of mobile apps may sometimes lead to healthcare professionals spending more time performing additional tasks such as filling out electronic forms and may generate more workload in some cases.[12] Some healthcare professionals also do not feel comfortable with work-related contact from patients/clients outside of business hours (however some professionals did find this useful for emergencies).[12]
Communicating with clients/patients while using a mobile device may need to be considered.[12] A decrease in eye contact and the potential to miss non-verbal cues due to concentrating on a screen while speaking with patients is a potential consideration.[12]
Society and Culture
Healthcare in low- and middle-income countries

Middle income and especially low-income countries face a plethora of constraints in their healthcare systems.[35] These countries face a severe lack of human and physical resources, as well as some of the largest burdens of disease, extreme poverty, and large population growth rates. Additionally, healthcare access to all reaches of society is generally low in these countries.[36]
According to a World Health Organization (WHO) report from June 2011, higher-income countries show more mHealth activity than do lower-income countries (as consistent with eHealth trends in general). Countries in the European Region are currently the most active and those in the African Region the least active. The WHO report findings also included that mHealth is most easily incorporated into processes and services that historically use voice communication through conventional telephone networks. The report[37] was the result of a mHealth survey module designed by researchers at the Earth Institute's Center for Global Health and Economic Development,[38] Columbia University.
The WHO notes an extreme deficit within the global healthcare workforce. The WHO notes critical healthcare workforce shortages in 57 countries—most of which are characterized as developing countries—and a global deficit of 2.4 million doctors, nurses, and midwives.[39] The WHO, in a study of the healthcare workforce in 12 countries of Africa, finds an average density of physicians, nurses and midwives per 1000 population of 0.64.[40] The density of the same metric is four times as high in the United States, at 2.6.[41]
The burden of disease is additionally much higher in low- and middle-income countries than high-income countries. The burden of disease, measured in disability-adjusted life year (DALY), which can be thought of as a measurement of the gap between current health status and an ideal situation where everyone lives into old age, free of disease and disability, is about five times higher in Africa than in high-income countries.[42] In addition, low- and middle-income countries are forced to face the burdens of both extreme poverty and the growing incidence of chronic diseases, such as diabetes and heart disease, an effect of new-found (relative) affluence.[3]
Considering poor infrastructure and low human resources, the WHO notes that the healthcare workforce in sub-Saharan Africa would need to be scaled up by as much as 140% to attain international health development targets such as those in the Millennium Declaration.[43]
The WHO, in reference to the healthcare condition in sub-Saharan Africa, states:
The problem is so serious that in many instances there is simply not enough human capacity even to absorb, deploy and efficiently use the substantial additional funds that are considered necessary to improve health in these countries.[43]
Mobile technology has made a recent and rapid appearance into low- and middle-income nations.[44] While, in the mHealth field, mobile technology usually refers to mobile phone technology, the entrance of other technologies into these nations to facilitate healthcare are also discussed here.
Health and development
The link between health and development can be found in three of the Millennium Development Goals (MDGs), as set forth by the United Nations Millennium Declaration in 2000. The MDGs that specifically address health include reducing child mortality; improving maternal health; combating HIV and AIDS, malaria, and other diseases; and increasing access to safe drinking water.[45] A progress report published in 2006 indicates that childhood immunization and deliveries by skilled birth attendants are on the rise, while many regions continue to struggle to achieve reductions in the prevalence of the diseases of poverty including malaria, HIV and AIDS and tuberculosis.[46]
Healthcare in developed countries
In developed countries, healthcare systems have different policies and goals in relation to the personal and population health care goals.
In the US and EU many patients and consumers use their cell phones and tablets to access health information and look for healthcare services. In parallel the number of mHealth applications grew significantly in the last years.
Doctors, nurses and clinicians use mobile devices to access patient information and other databases and resources.
Technology and market
Basic SMS functions and real-time voice communication serve as the backbone and the current most common use of mobile phone technology. The broad range of potential benefits to the health sector that the simple functions of mobile phones can provide should not be understated.[47]
The appeal of mobile communication technologies is that they enable communication in motion, allowing individuals to contact each other irrespective of time and place.[48][49] This is particularly beneficial for work in remote areas where the mobile phone, and now increasingly wireless infrastructure, is able to reach more people, faster. As a result of such technological advances, the capacity for improved access to information and two-way communication becomes more available at the point of need.
Mobile phones
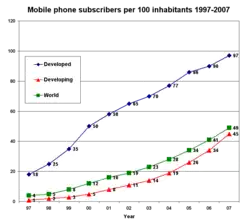
With the global mobile phone penetration rate drastically increasing over the last decade, mobile phones have made a recent and rapid entrance into many parts of the low- and middle-income world. Improvements in telecommunications technology infrastructure, reduced costs of mobile handsets, and a general increase in non-food expenditure have influenced this trend. Low- and middle-income countries are utilizing mobile phones as "leapfrog technology" (see leapfrogging). That is, mobile phones have allowed many developing countries, even those with relatively poor infrastructure, to bypass 20th century fixed-line technology and jump to modern mobile technology.[50]
The number of global mobile phone subscribers in 2007 was estimated at 3.1 billion of an estimated global population of 6.6 billion (47%).[51] These figures are expected to grow to 4.5 billion by 2012, or a 64.7% mobile penetration rate. The greatest growth is expected in Asia, the Middle East, and Africa. In many countries, the number of mobile phone subscribers has bypassed the number of fixed-line telephones; this is particularly true in developing countries.[52] Globally, there were 4.1 billion mobile phones in use in December 2008. See List of countries by number of mobile phones in use.
While mobile phone penetration rates are on the rise, globally, the growth within countries is not generally evenly distributed. In India, for example, while mobile penetration rates have increased markedly, by far the greatest growth rates are found in urban areas. Mobile penetration, in September 2008, was 66% in urban areas, while only 9.4% in rural areas. The all India average was 28.2% at the same time.[53] So, while mobile phones may have the potential to provide greater healthcare access to a larger portion of a population, there are certainly within-country equity issues to consider.
Mobile phones are spreading because the cost of mobile technology deployment is dropping and people are, on average, getting wealthier in low- and middle-income nations.[54] Vendors, such as Nokia, are developing cheaper infrastructure technologies (CDMA) and cheaper phones (sub $50–100, such as Sun's Java phone). Non-food consumption expenditure is increasing in many parts of the developing world, as disposable income rises, causing a rapid increase in spending on new technology, such as mobile phones. In India, for example, consumers have become and continue to become wealthier. Consumers are shifting their expenditure from necessity to discretionary. For example, on average, 56% of Indian consumers' consumption went towards food in 1995, compared to 42% in 2005. The number is expected to drop to 34% by 2015. That being said, although total share of consumption has declined, total consumption of food and beverages increased 82% from 1985 to 2005, while per-capita consumption of food and beverages increased 24%. Indian consumers are getting wealthier and they are spending more and more, with a greater ability to spend on new technologies.[55]
Smartphones
More advanced mobile phone technologies are enabling the potential for further healthcare delivery. Smartphone technologies are now in the hands of a large number of physicians and other healthcare workers in low- and middle-income countries. Although far from ubiquitous, the spread of smartphone technologies opens up doors for mHealth projects such as technology-based diagnosis support, remote diagnostics and telemedicine, preprogrammed daily self-assessment prompts, video or audio clips,[56] web browsing, GPS navigation, access to web-based patient information, post-visit patient surveillance, and decentralized health management information systems (HMIS).
While uptake of smartphone technology by the medical field has grown in low- and middle-income countries, it is worth noting that the capabilities of mobile phones in low- and middle-income countries has not reached the sophistication of those in high-income countries. The infrastructure that enables web browsing, GPS navigation, and email through smartphones is not as well developed in much of the low- and middle-income countries.[47] Increased availability and efficiency in both voice and data-transfer systems in addition to rapid deployment of wireless infrastructure will likely accelerate the deployment of mobile-enabled health systems and services throughout the world.[57]
Other technologies
Beyond mobile phones, wireless-enabled laptops and specialized health-related software applications are currently being developed, tested, and marketed for use in the mHealth field. Many of these technologies, while having some application to low- and middle-income nations, are developing primarily in high-income countries. However, with broad advocacy campaigns for free and open source software (FOSS), applications are beginning to be tailored for and make inroads in low- and middle-income countries.[6]
Some other mHealth technologies include:[1]
- Patient monitoring devices
- Mobile telemedicine/telecare devices
- Microcomputers
- Data collection software
- Mobile Operating System Technology
- Mobile applications (e.g., gamified/social wellness solutions)
- Chatterbots
Mobile device operating system technology
Technologies relate to the operating systems that orchestrate mobile device hardware while maintaining confidentiality, integrity and availability are required to build trust. This may foster greater adoption of mHealth technologies and services, by exploiting lower cost multi purpose mobile devices such as tablets, PCs, and smartphones. Operating systems that control these emerging classes of devices include Google's Android, Apple's iPhone OS, Microsoft's Windows Mobile, and RIM's BlackBerry OS.
Operating systems must be agile and evolve to effectively balance and deliver the desired level of service to an application and end user, while managing display real estate, power consumption and security posture. As advances in capabilities such as integrating voice, video and Web 2.0 collaboration tools into mobile devices, significant benefits can be achieved in the delivery of health care services. New sensor technologies[58] such as HD video and audio capabilities, accelerometers, GPS, ambient light detectors, barometers and gyroscopes[59] can enhance the methods of describing and studying cases, close to the patient or consumer of the health care service. This could include diagnosis, education, treatment and monitoring.
Air quality sensing technologies
Environmental conditions have a significant impact on public health. Per the World Health Organization, outdoor air pollution accounts for about 1.4% of total mortality.[60] Utilizing Participatory sensing technologies in mobile telephone, public health research can exploit the wide penetration of mobile devices to collect air measurements,[59] which can be utilized to assess the impact of pollution. Projects such as the Urban Atmospheres are utilizing embedded technologies in mobile phones to acquire real time conditions from millions of user mobile phones. By aggregating this data, public health policy shall be able to craft initiatives to mitigate risk associated with outdoor air pollution.
Data
Data has become an especially important aspect of mHealth. Data collection requires both the collection device (mobile phones, computer, or portable device) and the software that houses the information. Data is primarily focused on visualizing static text but can also extend to interactive decision support algorithms, other visual image information, and also communication capabilities through the integration of e-mail and SMS features. Integrating use of GIS and GPS with mobile technologies adds a geographical mapping component that is able to "tag" voice and data communication to a particular location or series of locations. These combined capabilities have been used for emergency health services as well as for disease surveillance, health facilities and services mapping, and other health-related data collection.
History
The motivation behind the development of the mHealth field arises from two factors. The first factor concerns the myriad constraints felt by healthcare systems of developing nations. These constraints include high population growth, a high burden of disease prevalence,[42] low health care workforce, large numbers of rural inhabitants, and limited financial resources to support healthcare infrastructure and health information systems. The second factor is the recent rapid rise in mobile phone penetration in developing countries to large segments of the healthcare workforce, as well as the population of a country as a whole.[51] With greater access to mobile phones to all segments of a country, including rural areas, the potential of lowering information and transaction costs in order to deliver healthcare improves.
The combination of these two factors has motivated much discussion of how greater access to mobile phone technology can be leveraged to mitigate the numerous pressures faced by developing countries' healthcare systems.
Research
Emerging trends and areas of interest:
- Emergency response systems (e.g., road traffic accidents, emergency obstetric care).
- Human resources coordination, management, and supervision.
- Mobile synchronous (voice) and asynchronous (SMS) telemedicine diagnostic and decision support to remote clinicians.[61]
- Clinician-focused, evidence-based formulary, database and decision support information available at the point of care.[61]
- Pharmaceutical supply chain integrity and patient safety systems (e.g. Sproxil and mPedigree).[62]
- Clinical care and remote patient monitoring.
- Health extension services.
- Inpatient monitoring.[63]
- Health services monitoring and reporting.
- Health-related mLearning for the general public.
- Mental health promotion[64][21] and illness prevention [65]
- Training and continuing professional development for health care workers.[66]
- Health promotion and community mobilization.
- Support of long-term conditions, for example medication reminders and diabetes self-management.[67][68]
- Peer-to-peer personal health management for telemedicine.[69]
- Social mobilization for infectious disease prevention.[70]
- Surgical follow-up, such as for major joint arthroplasty patients.[71]
- Mobile social media for global health personnel;[4] for example, the capacity to facilitate professional connectedness, and to empower health workforce.[72]
According to the Vodafone Group Foundation on February 13, 2008, a partnership for emergency communications was created between the group and United Nations Foundation. Such partnership will increase the effectiveness of the information and communications technology response to major emergencies and disasters around the world.
See also
- Health informatics
- Health 2.0
- Open source software packages for mHealth
- Telehealth
- Healthcare workforce information systems
- Telemedicine service providers
References
- 1 2 Adibi, Sasan, ed. (February 19, 2015). Mobile Health: A Technology Road Map. Springer Series in Bio-/Neuroinformatics. Vol. 5. Springer. p. 1. doi:10.1007/978-3-319-12817-7. ISBN 978-3-319-12817-7.
- 1 2 Cipresso, P.; Serino S.; Villani D.; Repetto C.; Selitti L.; Albani G.; Mauro A.; Gaggioli A.; Riva G. (2012). "Is your phone so smart to affect your states? An exploratory study based on psychophysiological measures". Neurocomputing. 84: 23–30. doi:10.1016/j.neucom.2011.12.027.
- 1 2 3 4 5 6 7 8 9 10 11 Vital Wave Consulting (February 2009). mHealth for Development: The Opportunity of Mobile Technology for Healthcare in the Developing World (PDF). United Nations Foundation, Vodafone Foundation. p. 9. Archived from the original (PDF) on 2012-12-03.
- 1 2 Pimmer, Christoph; Tulenko, Kate (2016). "The convergence of mobile and social media: Affordances and constraints of mobile networked communication for health workers in low- and middle-income countries". Mobile Media & Communication. 4 (2): 252–269. doi:10.1177/2050157915622657. S2CID 167748382.
- ↑ Germanakos P, Mourlas C, Samaras G. "A Mobile Agent Approach for Ubiquitous and Personalized eHealth Information Systems" (PDF). Proceedings of the Workshop on 'Personalization for e-Health' of the 10th International Conference on User Modeling (UM'05). Edinburgh, July 29, 2005. pp. 67–70.
- 1 2 3 Adibi, Sasan, ed. (November 24, 2014). mHealth Multidisciplinary Verticals. CRC Press (Taylor & Francis Group). p. 259. ISBN 978-1-482-21480-2.
- 1 2 Masson, M (December 2014). "Benefits of TED Talks". Canadian Family Physician. 60 (12): 1080. PMC 4264800. PMID 25500595.
- ↑ Istepanian, Robert S.H.; Laxminarayan, Swamy; Pattichis, Constantinos S., eds. (2006). M-Health: Emerging Mobile Health Systems. Topics in Biomedical Engineering. Boston, MA: Springer. Bibcode:2006mhem.book.....I. doi:10.1007/b137697. ISBN 978-0-387-26558-2. OCLC 836533004.
- 1 2 Torgan, Carol (November 6, 2009). "The mHealth Summit: Local & Global Converge". caroltorgan.com. Retrieved July 29, 2011.
- ↑ "mHealth: a new vision for healthcare" (PDF).
- ↑ Rowland SP, Fitzgerald JE, Holme T, Powell J, McGregor A (2020). "What is the clinical value of mHealth for patients?". NPJ Digital Medicine. 3: 4. doi:10.1038/s41746-019-0206-x. PMC 6957674. PMID 31970289.
- 1 2 3 4 5 6 7 8 Odendaal, Willem A.; Anstey Watkins, Jocelyn; Leon, Natalie; Goudge, Jane; Griffiths, Frances; Tomlinson, Mark; Daniels, Karen (March 2020). "Health workers' perceptions and experiences of using mHealth technologies to deliver primary healthcare services: a qualitative evidence synthesis". The Cochrane Database of Systematic Reviews. 3: CD011942. doi:10.1002/14651858.CD011942.pub2. ISSN 1469-493X. PMC 7098082. PMID 32216074.
- ↑ Pimmer, C, Brühlmann, F, Odetola TD, Dipeolu O, Oluwasola, DO, Ajuwon, AJ (2008). "Facilitating Professional Mobile Learning Communities with Instant Messaging". Computers & Education. 128: 102–11. doi:10.1016/j.compedu.2018.09.005. S2CID 53744443.
- 1 2 Devi, Balla Rama; Syed-Abdul, Shabbir; Kumar, Arun; Iqbal, Usman; Nguyen, Phung-Anh; Li, Yu-Chuan Jack; Jian, Wen-Shan (2015-11-01). "mHealth: An updated systematic review with a focus on HIV/AIDS and tuberculosis long term management using mobile phones". Computer Methods and Programs in Biomedicine. 122 (2): 257–265. doi:10.1016/j.cmpb.2015.08.003. ISSN 1872-7565. PMID 26304621.
- ↑ Murray, Melanie Caroline Margaret; Lester, Richard T.; Money, Deborah M.; Kestler, Mary H.; Alimenti, Ariane; Pick, Neora; Albert, Arianne YK; Maan, Evelyn J.; Qiu, Annie Q. (2017). "Mobile Text Messaging to Improve Medication Adherence and Viral Load in a Vulnerable Canadian Population Living With Human Immunodeficiency Virus: A Repeated Measures Study". Journal of Medical Internet Research. 19 (6): e190. doi:10.2196/jmir.6631. PMC 5472843. PMID 28572079.
- ↑ Maddison, Ralph; Rolleston, Anna; Stewart, Ralph; Jiang, Yannan; Whittaker, Robyn; Dale, Leila Pfaeffli (2015). "Text Message and Internet Support for Coronary Heart Disease Self-Management: Results From the Text4Heart Randomized Controlled Trial". Journal of Medical Internet Research. 17 (10): e237. doi:10.2196/jmir.4944. PMC 4642389. PMID 26490012.
- 1 2 Hamine, Saee; Gerth-Guyette, Emily; Faulx, Dunia; Green, Beverly B.; Ginsburg, Amy Sarah (2015-02-24). "Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review". Journal of Medical Internet Research. 17 (2): e52. doi:10.2196/jmir.3951. ISSN 1438-8871. PMC 4376208. PMID 25803266.
- ↑ Belt, Tom H. van de; Gelder, Marleen MHJ van; Massari, Daniele De; Zimmerman, Lisa; Hendriks, Sandra; Engelen, Lucien JLPG; Heeren, Barend; Lancee, Gerardus J.; Tack, Cornelis J. (2018). "Glucose Control, Disease Burden, and Educational Gaps in People With Type 1 Diabetes: Exploratory Study of an Integrated Mobile Diabetes App". JMIR Diabetes. 3 (4): e17. doi:10.2196/diabetes.9531. PMC 6286423. PMID 30470680.
- ↑ Chomutare, Taridzo; Fernandez-Luque, Luis; Årsand, Eirik; Hartvigsen, Gunnar (2011-01-01). "Features of Mobile Diabetes Applications: Review of the Literature and Analysis of Current Applications Compared Against Evidence-Based Guidelines". Journal of Medical Internet Research. 13 (3): e65. doi:10.2196/jmir.1874. PMC 3222161. PMID 21979293.
- ↑ Nair, Uthara; Armfield, Nigel R.; Chatfield, Mark D.; Edirippulige, Sisira (December 2018). "The effectiveness of telemedicine interventions to address maternal depression: A systematic review and meta-analysis". Journal of Telemedicine and Telecare. 24 (10): 639–650. doi:10.1177/1357633X18794332. ISSN 1758-1109. PMID 30343660.
- 1 2 Farb, Norman AS; Saab, Bechara J.; Walsh, Kathleen Marie (2019). "Effects of a Mindfulness Meditation App on Subjective Well-Being: Active Randomized Controlled Trial and Experience Sampling Study". JMIR Mental Health. 6 (1): e10844. doi:10.2196/10844. PMC 6329416. PMID 30622094.
- ↑ Furberg RD, Uhrig JD, Bann CM, Lewis MA, Harris JL, Williams P, Coomes C, Martin N, Kuhns L (2012). "Technical Implementation of a Multi-Component, Text Message–Based Intervention for Persons Living with HIV". JMIR Res Protoc. 1 (2): e17. doi:10.2196/resprot.2017. PMC 3626151. PMID 23612237.
- ↑ "mHealth. New horizons for health through mobile technologies" (PDF). World Health Organization. Retrieved May 22, 2014.
- ↑ Baum, Peter (September 18–21, 2012). "A new track for technology: Can ICT take care for healthier lifestyles?". hdl:10419/52185.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Mahmud, N; Rodriguez, Nesbit (2010). "A text message-based intervention to bridge the healthcare communication gap in the rural developing world". Technol Health Care. 18 (2): 137–144. doi:10.3233/THC-2010-0576. PMID 20495253.
- ↑ Bloomfield, Gerald S; Vedanthan, Rajesh; Vasudevan, Lavanya; Kithei, Anne; Were, Martin; Velazquez, Eric J (2014). "Mobile health for non-communicable diseases in Sub-Saharan Africa: a systematic review of the literature and strategic framework for research". Globalization and Health. 10 (1): 49. doi:10.1186/1744-8603-10-49. ISSN 1744-8603. PMC 4064106. PMID 24927745.
- ↑ Republic of Uganda. (2012). Coordination and harmonisation of eHealth initiatives [circular ADM 45/273/01]. Kampala: Uganda Ministry of Health.
- ↑ Helsper, Ellen J; Reisdorf, Bianca C (2017). "The emergence of a "digital underclass" in Great Britain and Sweden: Changing reasons for digital exclusion". New Media & Society. 19 (8): 1253–1270. doi:10.1177/1461444816634676. ISSN 1461-4448. S2CID 30116698.
- ↑ Hampshire, Kate; Porter, Gina; Owusu, Samuel Asiedu; Mariwah, Simon; Abane, Albert; Robson, Elsbeth; Munthali, Alister; DeLannoy, Ariane; Bango, Andisiwe (2015). "Informal m-health: How are young people using mobile phones to bridge healthcare gaps in Sub-Saharan Africa?". Social Science & Medicine. 142: 90–99. doi:10.1016/j.socscimed.2015.07.033. PMID 26298645.
- ↑ Haenssgen, Marco J. (2018). "The struggle for digital inclusion: Phones, healthcare, and marginalisation in rural India" (PDF). World Development. 104: 358–374. doi:10.1016/j.worlddev.2017.12.023.
- ↑ Lupton, Deborah (2013). "Quantifying the body: monitoring and measuring health in the age of mHealth technologies". Critical Public Health. 23 (4): 393–403. doi:10.1080/09581596.2013.794931. ISSN 0958-1596. S2CID 53492891.
- 1 2 Lupton, Deborah (2014). "Critical Perspectives on Digital Health Technologies: Digital Health Technologies". Sociology Compass. 8 (12): 1344–1359. doi:10.1111/soc4.12226.
- ↑ Haas, Sebastian; Wohlgemuth, Sven; Echizen, Isao; Sonehara, Noboru; Müller, Günter (2011). "Aspects of privacy for electronic health records". International Journal of Medical Informatics. 80 (2): e26–e31. doi:10.1016/j.ijmedinf.2010.10.001. PMID 21041113.
- ↑ "WHO Disease and injury country estimates". World Health Organization. 2009. Retrieved Nov 11, 2009.
- ↑ Larsson, Emma; Mawkin, Mala; Taylor-Robinson, Simon D; Harrington, Peter; Gondwe, Hastings; Watson, Chris; Gallagher, Joseph; Ledwidge, Mark; Chirambo, Griphin Baxter; O'Donoghue, John (December 2020). "Implementing Innovative Approaches to Healthcare in a Lower-Middle Income Country: Perspectives from Malawi". International Journal of General Medicine. 13: 1723–1730. doi:10.2147/IJGM.S285130. ISSN 1178-7074. PMC 7783193. PMID 33414644.
- ↑ Peters, David H.; Garg, Anu; Bloom, Gerry; Walker, Damian G.; Brieger, William R.; Hafizur Rahman, M. (2008). "Poverty and Access to Health Care in Developing Countries". Annals of the New York Academy of Sciences. 1136 (1): 161–171. Bibcode:2008NYASA1136..161P. doi:10.1196/annals.1425.011. PMID 17954679. S2CID 24649523.
- ↑ mHealth: New horizons for health through mobile technologies. Global Observatory for eHealth series. Vol. 3. World Health Organization. 7 June 2011. ISBN 978-92-4-156425-0. Archived from the original on January 29, 2013.
- ↑ "Center for Global Health and Economic Development". Archived from the original on 27 February 2009.
- ↑ World Health Organization (2006). The World Health Report 2006: Working Together for Health (Report). Geneva: WHO. Archived from the original on April 10, 2006.
- ↑ Kinfu, Y.; Dal Poz, M.; Mercer, H.; Evans, D.B. (March 2009). "Table 3. Current density of physicians, nurses and midwives and required rate of workforce growth according to population growth rates in 12 African countries". Bulletin of the World Health Organization. 87 (3): 225–230. doi:10.2471/blt.08.051599. PMC 2654639. PMID 19377719. Archived from the original on October 12, 2009.
- ↑ UNData. "Statistics Physicians density (per 10 000 population)". WHO Data. Archived from the original on 15 February 2009.
- 1 2 The Global Burden of Disease: 2004 Update (Report). World Health Organization. 2008. Archived from the original on March 24, 2009.
- 1 2 Kinfu, Y.; Dal Poz, M.; Mercer, H.; Evans, D.B. (March 2009). "The health worker shortage in Africa: are enough physicians and nurses being trained?". Bulletin of the World Health Organization. 87 (3): 225–230. doi:10.2471/blt.08.051599. PMC 2654639. PMID 19377719. Archived from the original on March 16, 2009.
- ↑ "The power of mobile money". The Economist. September 24, 2009.
- ↑ United Nations General Assembly Session 55 Resolution 55/2. United Nations Millennium Declaration A/res/55/2 18 September 2000.
- ↑ United Nations (2006). The Millennium Development Goals Report (PDF) (Report). New York: United Nations. Archived from the original (PDF) on 2007-06-14. Retrieved 2017-10-26.
- 1 2 Mechael, Patricia N. (December 2006). Exploring Health-related Uses of Mobile Phones: An Egyptian Case Study (PDF) (PhD). London: London School of Hygiene and Tropical Medicine. p. 264 – via iHRIS Wiki.
- ↑ Agar, J. (2003). Constant Touch: A Global History of the Mobile Phone Cambridge: Icon Books Ltd.
- ↑ Ling, R. (2004). The mobile connection: The cell phone's impact on society London: Morgan Kaufmann
- ↑ "Leaders: The limits of leapfrogging; Technology and development". The Economist. February 7, 2008.
- 1 2 "Global Mobile Phone Subscribers to Reach 4.5 Billion by 2012". Cellular News. March 9, 2008. Retrieved 2010-04-01.
- ↑ ITU (2003). "Mobile overtakes fixed: Implications for policy and regulation" (PDF). Geneva: International Telecommunications Union.
- ↑ Kathuria, R, Uppal M., Mamta (2009). An econometric analysis of the impact of mobile. Case paper in India: The impact of mobile phones. Vodafone Group Plc. The Policy Paper Series. November 2009
- ↑ "Global Economic Prospects 2007: Managing the Next Wave of Globalization". World Bank report. Archived from the original on 2006-12-21.
- ↑ Jonathan Ablett; Aadarsh Baijal; Eric Beinhocker; Anupam Bose; Diana Farrell; Ulrich Gersch; Ezra Greenberg; Shishir Gupta; Sumit Gupta (May 2007), The 'bird of gold': the rise of India's consumer market, McKinsey Global Institute
- ↑ Ben-Zeev, Dror; Brian, Rachel M.; Jonathan, Geneva; Razzano, Lisa; Pashka, Nicole; Carpenter-Song, Elizabeth; Drake, Robert E.; Scherer, Emily A. (2018). "Mobile Health (mHealth) Versus Clinic-Based Group Intervention for People With Serious Mental Illness: A Randomized Controlled Trial". Psychiatric Services. 69 (9): 978–985. doi:10.1176/appi.ps.201800063. ISSN 1075-2730. PMID 29793397.
- ↑ Istepanian, R.S.H.; Jovanov, E.; Zhang, Y.T. (December 2004). "Introduction to the Special Section on M-Health: Beyond Seamless Mobility and Global Wireless Health-care Connectivity" (PDF). IEEE Transactions on Information Technology in Biomedicine. 8 (4): 405–414. doi:10.1109/titb.2004.840019. PMID 15615031. S2CID 71150.
- ↑ New sensor technologies. 2008. CiteSeerX 10.1.1.141.6348.
- 1 2 Lane, Nicholas; Miluzzo, Emiliano; Lu, Hong; Peebles, Daniel; Choudhury, Tanzeem; Campbell, Andrew (2010). "A survey of mobile phone sensing". IEEE Communications Magazine. 48 (9): 140–150. CiteSeerX 10.1.1.186.9844. doi:10.1109/MCOM.2010.5560598. S2CID 356450.
- ↑ Ostro, Bart (2004). Outdoor air pollution : assessing the environmental burden of disease at national and local levels (null ed.). Geneva: World Health Organization, Protection of the Human Environment. ISBN 978-92-4-159146-1.
- 1 2 Mechael, P. (August 2007). WHO mHealth Review: Towards the Development of an mHealth Strategy (Report).
- ↑ Bennett, Simeon (14 May 2010). "Ghana News: West African Innovation Hits Global Stage". Joy Online. Modified for length by Richard Akuoko. Bloomberg. Archived from the original on 2010-05-16. Retrieved 2010-08-14.
- ↑ Dobkin, Bruce H.; Dorsch, Andrew (2011). "The Promise of mHealth: Daily Activity Monitoring and Outcome Assessments by Wearable Sensors". Neurorehabilitation and Neural Repair. 25 (9): 788–798. doi:10.1177/1545968311425908. ISSN 1545-9683. PMC 4098920. PMID 21989632.
- ↑ Adkins, Elizabeth C.; O'Loughlin, Kristen; Neary, Martha; Schueller, Stephen M. (2018). "Discovery of and Interest in Health Apps Among Those With Mental Health Needs: Survey and Focus Group Study". Journal of Medical Internet Research. 20 (6): e10141. doi:10.2196/10141. PMC 6018235. PMID 29891468.
- ↑ Deady, Mark; GLozier, N.; Calvo, R.A.; Johnston, D M. (2020). "Preventing depression using a smartphone app: a randomized controlled trial". Psychological Medicine. 2020. doi:10.1017/S003329172000208 (inactive 31 October 2021).
{{cite journal}}: CS1 maint: DOI inactive as of October 2021 (link) - ↑ Martin, Nick (22 July 2013). "Charting the Future of Capacity Building for mHealth". TechChange. Retrieved August 4, 2013.
- ↑ Elliott, Jane (16 January 2010). "Text reminder to take epilepsy tablets". BBC News.
- ↑ Chomutare T, Fernandez-Luque L, Arsand E, Hartvigsen G (22 September 2011). "Features of mobile diabetes applications". Journal of Medical Internet Research. 13 (3): e65. doi:10.2196/jmir.1874. PMC 3222161. PMID 21979293.
- ↑ Bailey, Eric (August 15, 2013). "Deborah Jeffries, MD, talks about collaborative video and emerging telemedicine trends". mHealthNews. HIMSS Media. Archived from the original on 2013-08-25.
- ↑ Abbott, Patricia; Barbosa, Sayonara (2015). "Using Information Technology and Social Mobilization to Combat Disease" (PDF). Acta Paulista de Enfermagem. 28 (1). ISSN 0103-2100. Retrieved 5 April 2015.
- ↑ Koutras C, Bitsaki M, Koutras G, Nikolaou C, Heep H (17 August 2015). "Socioeconomic impact of e-Health services in major joint replacement: A scoping review". Technol Health Care. 23 (6): 809–17. doi:10.3233/THC-151036. PMID 26409523.
- ↑ Abdul SS, Lin CW, Scholl J, Fernandez-Luque L, Jian WS, Hsu MH, Li YC (2011). "Facebook use leads to health-care reform in Taiwan". The Lancet. 377 (9783): 2083–2084. doi:10.1016/S0140-6736(11)60919-7. PMID 21684378. S2CID 32789692.
Further reading
- Asangansi, Ime; Braa, Kristin (2010). Safran, C.; Reti, S.; Marin, H.F. (eds.). The emergence of mobile-supported national health information systems in developing countries. MEDINFO 2010. Studies in health technology and informatics. Vol. 160. IOS Press. pp. 540–544. doi:10.3233/978-1-60750-588-4-540. ISBN 978-1-60750-588-4. PMID 20841745.

- Brown, David (30 November 2007). "Globally, Deaths From Measles Drop Sharply". World. The Washington Post. Retrieved 2010-08-14. Describes role of EpiSurveyor mobile data collection software in contributing to the highly successful fight against measles mortality.
- "The doctor in your pocket". The Economist. 15 September 2005.
- Giuffrida, Antonio; El-Wahab, Shireen; Anta, Rafael (February 2009). Mobile Health: The potential of mobile telephony to bring health care to the majority (Report). Inter-American Development Bank.
- Huang, Anpeng; Chen, Chao; Bian, Kaigui; et al. (March 2014). "WE-CARE: An Intelligent Mobile Telecardiology System to Enable mHealth Applications". IEEE Journal of Biomedical and Health Informatics. 18 (2): 693–702. doi:10.1109/jbhi.2013.2279136. PMID 24608067. S2CID 14856105.
- Huang, Anpeng. "Worldwide Gallery for Mobile Health". Archived from the original on 2014-10-20.
- "JMIR mHealth and uHealth". JMIR mHealth and uHealth. JMIR Publications. ISSN 2291-5222.
 Peer-reviewed journal on mHealth and uHealth (ubiquitous health)
Peer-reviewed journal on mHealth and uHealth (ubiquitous health) - Kaplan, Warren A. (23 May 2006). "Can the ubiquitous power of mobile phones be used to improve health outcomes in developing countries?". Globalization and Health. 2: 9. doi:10.1186/1744-8603-2-9. PMC 1524730. PMID 16719925.

- Mechael, Patricia N. (Winter 2009). "The Case for mHealth in Developing Countries". Innovations: Technology, Governance, Globalization. 4 (1): 103–118. doi:10.1162/itgg.2009.4.1.103.
- Mechael, Patricia N.; Sloninsky, Daniela (August 2008). Towards the Development of an mHealth Strategy: A Literature Review (PDF) (Working Document). New York: Earth Institute at Columbia University.
- "Mobile Medical Applications". U.S. Food and Drug Administration. Archived from the original on 2 May 2013.
- Olmeda, Christopher J. (2000). Information Technology in Systems of Care. Delfin Press. ISBN 978-0-9821442-0-6.
- Saran, Cliff (3 April 2008). "Technology plays crucial role in vaccination distribution". Computer Weekly. TechTarget. Retrieved 2010-08-14. Discusses use of handheld electronic data collection in managing public health data and activities.
- Shackleton, Sally-Jean (May 2007). Rapid Assessment of Cell Phones for Development (Report). Implemented by Women'sNet. UNICEF South Africa.
- Tal, Amir; Torous, John, eds. (September 2017). Special Issue: Digital and Mobile Mental Health. Psychiatric Rehabilitation Journal. Vol. 40. ISBN 978-1-4338-9119-9.
- United Nations Department of Economic and Social Affairs, Division for Public Administration and Development Management (2007). Mobile Applications on Health and Learning (PDF) (Report). Compendium of ICT Applications on Electronic Government. Vol. 1. United Nations. ST/ESA/PAD/SER.E/113.
- "A world of witnesses". The Economist. 10 April 2008. Retrieved 2017-10-26. Discusses use of EpiSurveyor software in public health monitoring in Africa.