Maternal death
| Maternal death | |
|---|---|
| Other names: Maternal mortality | |
 | |
| A mother dies and is taken by angels as her new-born child is taken away, A grave from 1863 in Striesener Friedhof in Dresden. | |
Maternal death, also known as maternal mortality, is defined in slightly different ways by different health organizations. The World Health Organization (WHO) defines maternal death as the death of a pregnant woman due to complications related to pregnancy, underlying conditions worsened by the pregnancy or management of these conditions. This can occur either while she is pregnant or within six weeks of resolution of the pregnancy.[1] The CDC definition of pregnancy-related deaths extends the period of consideration to include one year from the resolution of the pregnancy.[2][3] Pregnancy associated death, as defined by the American College of Obstetricians and Gynecologists (ACOG), are all deaths occurring within one year of a pregnancy resolution.[4] Identification of pregnancy associated deaths is important for deciding whether or not the pregnancy was a direct or indirect contributing cause of the death.
There are two main measures used when talking about the rates of maternal mortality in a community or country. These are the maternal mortality ratio and maternal mortality rate, both abbreviated as "MMR".[5] By 2017, the world maternal mortality rate had declined 44% since 1990; however, everyday 808 women die from pregnancy or childbirth related causes.[6] According to the United Nations Population Fund (UNFPA) 2017 report, about every 2 minutes a woman dies because of complications due to child birth or pregnancy. For every woman who dies, there are about 20 to 30 women who experience injury, infection, or other birth or pregnancy related complication.[6]
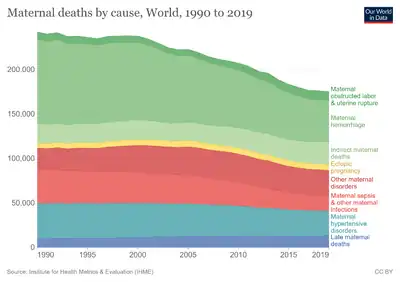
UNFPA estimated that 303,000 women died of pregnancy or childbirth related causes in 2015.[6][7] The WHO divides causes of maternal deaths into two categories: direct obstetric deaths and indirect obstetric deaths. Direct obstetric deaths are causes of death due to complications of pregnancy, birth or termination. For example, these could range from severe bleeding to obstructed labor, for which there are highly effective interventions.[8][1] Indirect obstetric deaths are caused by pregnancy interfering or worsening an existing condition, like a heart problem.[1]
As women have gained access to family planning and skilled birth attendant with backup emergency obstetric care, the global maternal mortality ratio has fallen from 385 maternal deaths per 100,000 live births in 1990 to 216 deaths per 100,000 live births in 2015.[6][7] Many countries halved their maternal death rates in the last 10 years.[6] Although attempts have been made to reduce maternal mortality, there is much room for improvement, particularly in low-resource regions. Over 85% of maternal deaths are in low-resource communities in Africa and Asia.[6] In higher resource regions, there are still significant areas with room for growth, particularly as they relate to racial and ethnic disparities and inequities in maternal mortality and morbidity rates.[4][7]
Overall, maternal mortality is an important marker of the overall health of the country and reflects on its health infrastructure.[4] Lowering the amount of maternal death is an important goal of many health organizations world-wide.
Causes
Direct obstetric deaths
Direct obstetric deaths are due to complications of pregnancy, birth, termination or complications arising from their management.[1]
The causes of maternal death vary by region and level of access. According to a study published in the Lancet which covered the period from 1990 to 2013, the most common causes of maternal death world-wide are postpartum bleeding (15%), complications from unsafe abortion (15%), hypertensive disorders of pregnancy (10%), postpartum infections (8%), and obstructed labor (6%).[9] Other causes include blood clots (3%) and pre-existing conditions (28%).[10]
Descriptions by condition
Postpartum bleeding happens when there is uncontrollable bleeding from the uterus, cervix or vaginal wall after bleeding. This can happen when the uterus does not contract correctly after birth, there is left over placenta in the uterus, or there are cuts in the cervix or vagina from birth.[11]
Hypertensive disorders of pregnancy happen when the body does not regulate blood pressure correctly. In pregnancy, this is due to changes at the level of the blood vessels, likely because of the placenta.[12] This includes medical conditions like gestational hypertension and pre-eclampsia.
Postpartum infections are infections of the uterus or other parts of the reproductive tract after the resolution of a pregnancy. They are usually bacterial and cause fever, increased pain, and foul-smelling discharge.[13]
Obstructed labor happens when the baby does not properly move into the pelvis and out of the body during labor. The most common cause of obstructed labor is when the baby's head is too big or angled at a way that does not allow it to pass through the pelvis and birth canal.[14]
Blood clots can occur in different vessels in the body, including vessels in the arms, legs, and lungs. They can cause problems in the lung, as well as travel to the heart or brain, leading to complications.[15]
Unsafe abortion
When abortion is legal and accessible, it is widely regarded as safer than carrying a pregnancy to term and delivery. In fact, a study published in the journal Obstetrics & Gynecology reported that in the United States, carrying a pregnancy to term and delivering a baby comes with 14 times increased risk of death as compared to a legal abortion.[16] However, in many regions of the world, abortion is not legal and can be unsafe.[16][17][18] Maternal deaths caused by improperly performed procedures are preventable and contribute 13% to the maternal mortality rate worldwide. This number is increased to 25% in countries where other causes of maternal mortality are low, such as in Eastern European and South American countries. This makes unsafe abortion practices the leading cause of maternal death worldwide.[19]
Unsafe abortion is another major cause of maternal death worldwide. In regions where abortion is legal and accessible, abortion is safe and does not contribute greatly to overall rates of maternal death.[7][17][16] However, in regions where abortions are not legal, available, or regulated, unsafe abortion practices can cause significant rates of maternal death.[20] According to the World Health Organization in 2009, every eight minutes a woman died from complications arising from unsafe abortions.[21]
Unsafe abortion practices are defined by the WHO as procedures that are performed by someone without the appropriate training and/or ones that are performed in an environment that is not considered safe or clean.[19][22] Using this definition, the WHO estimates that out of the 45 million abortions that are performed each year globally, 19 million of these are considered unsafe, and 97% of these unsafe abortions occur in developing countries.[19][23] Complications include hemorrhage, infection, sepsis and genital trauma.[24]
Rates

One proposal for measuring trends and variations in risks to maternal death associated with maternal death is to measure the percentage of induced abortions that are defined unsafe (by the WHO) and by the ratio of deaths per 100,000 procedures, which would be defined as the abortion mortality ratio.[23]
There are four primary types of data sources that are used to collect abortion-related maternal mortality rates: confidential enquiries, registration data, verbal autopsy, and facility-based data sources. A verbal autopsy is a systematic tool that is used to collect information on the cause of death from laypeople and not medical professionals.[25]
Confidential enquires for maternal deaths do not occur very often on a national level in most countries. Registration systems are usually considered the "gold-standard" method for mortality measurements. However, they have been shown to miss anywhere between 30 and 50% of all maternal deaths.[25] Another concern for registration systems is that 75% of all global births occur in countries where vital registration systems do not exist, meaning that many maternal deaths occurring during these pregnancies and deliveries may not be properly record through these methods. There are also issues with using verbal autopsies and other forms of survey in recording maternal death rates. For example, the family's willingness to participate after the loss of a loved one, misclassification of the cause of death, and under-reporting all present obstacles to the proper reporting of maternal mortality causes. Finally, an potential issue with facility-based data collection on maternal mortality is the likelihood that women who experience abortion-related complications to seek care in medical facilities. This is due to fear of social repercussions or legal activity in countries where unsafe abortion is common since it is more likely to be legally restrictive and/or more highly stigmatizing.[25] Another concern for issues related to errors in proper reporting for accurate understanding of maternal mortality is the fact that global estimates of maternal deaths related to a specific cause present those related to abortion as a proportion of the total mortality rate. Therefore, any change, whether positive or negative, in the abortion-related mortality rate is only compared relative to other causes, and this does not allow for proper implications of whether abortions are becoming more safe or less safe with respect to the overall mortality of women.[25]
Prevention

The prevention and reduction of maternity death is one of the United Nation's Sustainable Development Goals, specifically Goal 3, "Good health and well being". Promoting effective contraceptive use and information distributed to a wider population, with access to high-quality care, can make steps towards reducing the number of unsafe abortions. For nations that allow contraceptives, programs should be instituted to allow the easier accessibility of these medications.[24] However, this alone will not eliminate the demand for safe services, awareness on safe abortion services, health education on prenatal check ups and proper implementation of diets during pregnancy and lactation also contributes to its prevention.[26]
Indirect obstetric deaths
Indirect obstetric deaths are caused by preexisting health problem worsened by pregnancy or newly developed health problem unrelated to pregnancy .[27][1] Fatalities during but unrelated to a pregnancy are termed accidental, incidental, or non-obstetrical maternal deaths.
Indirect causes include malaria, anemia,[28] HIV/AIDS, and cardiovascular disease, all of which may complicate pregnancy or be aggravated by it.[29] Risk factors associated with increased maternal death include the age of the mother, obesity before becoming pregnant, other pre-existing chronic medical conditions, and cesarean delivery.[30][31]
Risk factors
According to a 2004 WHO publication, sociodemographic factors such as age, access to resources and income level are significant indicators of maternal outcomes. Young mothers face higher risks of complications and death during pregnancy than older mothers,[32] especially adolescents aged 15 years or younger.[33] Adolescents have higher risks for postpartum hemorrhage,endometritis, operative vaginal delivery, episiotomy, low birth weight, preterm delivery, and small-for-gestational-age infants, all of which can lead to maternal death.[33] The leading cause of death for girls at the age of 15 in developing countries is complication through pregnancy and childbirth. They have more pregnancies, on average, than women in developed countries, and it has been shown that 1 in 180 15-year-old girls in developing countries who become pregnant will die due to complications during pregnancy or childbirth. This is compared to women in developed countries, where the likelihood is 1 in 4900 live births.[32] However, in the United States, as many women of older age continue to have children, the maternal mortality rate has risen in some states, especially among women over 40 years old.[30]
Structural support and family support influences maternal outcomes.[34] Furthermore, social disadvantage and social isolation adversely affects maternal health which can lead to increases in maternal death.[35] Additionally, lack of access to skilled medical care during childbirth, the travel distance to the nearest clinic to receive proper care, number of prior births, barriers to accessing prenatal medical care and poor infrastructure all increase maternal deaths.[32]
Causes
Pregnancy-related deaths between 2011 and 2014 in the United States have been shown to have major contributions from non-communicable diseases and conditions, and the following are some of the more common causes related to maternal death:[2] cardiovascular diseases (15.2%.), non-cardiovascular diseases (14.7%), infection or sepsis (12.8%), hemorrhage (11.5%), cardiomyopathy (10.3%), pulmonary embolism (9.1%), cerebrovascular accidents (7.4%), hypertensive disorders of pregnancy (6.8%), amniotic fluid embolism (5.5%), and anesthesia complications (0.3%).
Three delays model
The three delays model addresses three critical factors that inhibit women from receiving appropriate maternal health care.[36] These factors include:
- Delay in seeking care
- Delay in reaching care
- Delay in receiving adequate and appropriate care[37]
Delays in seeking care are due to the decisions made by the women who are pregnant and/or other decision-making individuals. Decision-making individuals can include a spouse and family members.[37] Examples of reasons for delays in seeking care include lack of knowledge about when to seek care, inability to afford health care, and women needing permission from family members.[36][37]
Delays in reaching care include factors such as limitations in transportation to a medical facility, lack of adequate medical facilities in the area, and lack in confidence in medicine.[38]
Delays in receiving adequate and appropriate care may result from an inadequate number of trained providers, lack of appropriate supplies, and the lack of urgency or understanding of an emergency.[36][37]
The three delays model illustrates that there are a multitude of complex factors, both socioeconomic and cultural, that can result in maternal death.[36]
Measurement
The four measures of maternal death are the maternal mortality ratio (MMR), maternal mortality rate, lifetime risk of maternal death and proportion of maternal deaths among deaths of women of reproductive years (PM).
Maternal mortality ratio (MMR) is the ratio of the number of maternal deaths during a given time period per 100,000 live births during the same time-period.[39] The MMR is used as a measure of the quality of a health care system.
Maternal mortality rate (MMRate) is the number of maternal deaths in a population divided by the number of women of reproductive age, usually expressed per 1,000 women.[39]
Lifetime risk of maternal death is a calculated prediction of a woman's risk of death after each consecutive pregnancy.[40] The calculation pertains to women during their reproductive years.[40] The adult lifetime risk of maternal mortality can be derived using either the maternal mortality ratio (MMR), or the maternal mortality rate (MMRate).[39]
Proportion of maternal deaths among deaths of women of reproductive age (PM) is the number of maternal deaths in a given time period divided by the total deaths among women aged 15–49 years.[41]
Approaches to measuring maternal mortality include civil registration system, household surveys, census, reproductive age mortality studies (RAMOS) and verbal autopsies.[41] The most common household survey method, recommended by the WHO as time- and cost-effective, is the sisterhood method.[42]
Trends
The United Nations Population Fund (UNFPA; formerly known as the United Nations Fund for Population Activities) have established programs that support efforts in reducing maternal death. These efforts include education and training for midwives, supporting access to emergency services in obstetric and newborn care networks, and providing essential drugs and family planning services to pregnant women or those planning to become pregnant.[6] They also support efforts for review and response systems regarding maternal deaths.
According to the 2010 United Nations Population Fund report, low-resource nations account for ninety-nine percent of maternal deaths with the majority of those deaths occurring in Sub-Saharan Africa and Southern Asia.[41] Globally, high and middle income countries experience lower maternal deaths than low income countries. The Human Development Index (HDI) accounts for between 82 and 85 percent of the maternal mortality rates among countries.[43] In most cases, high rates of maternal deaths occur in the same countries that have high rates of infant mortality. These trends are a reflection that higher income countries have stronger healthcare infrastructure, more doctors, use more advanced medical technologies and have fewer barriers to accessing care than low income countries. In low income countries, the most common cause of maternal death is obstetrical hemorrhage, followed by hypertensive disorders of pregnancy. This is contrast to high income countries, for which the most common cause is thromboembolism.[44]
Between 1990 and 2015, the maternal mortality ratio has decreased from 385 deaths per 100,000 live births to 216 maternal deaths per 100,000 live births.[6][45] Some factors that have been attributed to the decreased maternal deaths seen between this period are in part to the access that women have gained to family planning services and skilled birth attendance, meaning a midwife, doctor, or trained nurse), with back-up obstetric care for emergency situations that may occur during the process of labor.[6] This can be examined further by looking at statistics in some areas of the world where inequities in access to health care services reflect an increased number of maternal deaths. The high maternal death rates also reflect disparate access to health services between resource communities and those that are high-resource or affluent.[32]
Prevention
According to UNFPA, there are four essential elements for prevention of maternal death.[6] These include, prenatal care, assistance with birth, access to emergency obstetric care and adequate postnatal care. It is recommended that expectant mothers receive at least four antenatal visits to check and monitor the health of mother and fetus. Second, skilled birth attendance with emergency backup such as doctors, nurses and midwives who have the skills to manage normal deliveries and recognize the onset of complications. Third, emergency obstetric care to address the major causes of maternal death which are hemorrhage, sepsis, unsafe abortion, hypertensive disorders and obstructed labor. Lastly, postnatal care which is the six weeks following delivery. During this time, bleeding, sepsis and hypertensive disorders can occur, and newborns are extremely vulnerable in the immediate aftermath of birth. Therefore, follow-up visits by a health worker to assess the health of both mother and child in the postnatal period is strongly recommended.
Additionally, reliable access to information, compassionate counseling and quality services for the management of any issues that arise from abortions (whether safe or unsafe) can be beneficial in reducing the number of maternal deaths.[19] In regions where abortion is legal, abortion practices need to be safe in order to effectively reduce the number of maternal deaths related to abortion.
Maternal Death Surveillance and Response is another strategy that has been used to prevent maternal death. This is one of the interventions proposed to reduce maternal mortality where maternal deaths are continuously reviewed to learn the causes and factors that led to the death. The information from the reviews is used to make recommendations for action to prevent future similar deaths.[46] Maternal and perinatal death reviews have been in practice for a long time worldwide, and the World Health Organization (WHO) introduced the Maternal and Perinatal Death Surveillance and Response (MPDSR) with a guideline in 2013. Studies have shown that acting on recommendations from MPDSR can reduce maternal and perinatal mortality by improving quality of care in the community and health facilities.
Prenatal care
It was estimated that in 2015, a total of 303,000 women died due to causes related to pregnancy or childbirth.[6] The majority of these were due to severe bleeding, sepsis or infections, eclampsia, obstructed labor, and consequences from unsafe abortions. Most of these causes are either preventable or have highly effective interventions.[6] An important factor that contributes to the maternal mortality rate is access and opportunity to receive prenatal care. Women who do not receive prenatal care are between three and four times more likely to die from complications resulting from pregnancy or delivery than those who receive prenatal care. Even in high-resource countries, many women do not receive the appropriate preventative or prenatal care. For example, 25% of women in the United States do not receive the recommended number of prenatal visits. This number increases for women among traditionally marginalized populations—32% of African American women and 41% for American Indian and Alaska Native women do not receive the recommended preventative health services prior to delivery.[47]
Medical technologies
The decline in maternal deaths has been due largely to improved aseptic techniques, better fluid management and quicker access to blood transfusions, and better prenatal care.
Technologies have been designed for resource poor settings that have been effective in reducing maternal deaths as well. The non-pneumatic anti-shock garment is a low-technology pressure device that decreases blood loss, restores vital signs and helps buy time in delay of women receiving adequate emergency care during obstetric hemorrhage.[48] It has proven to be a valuable resource. Condoms used as uterine tamponades have also been effective in stopping post-partum hemorrhage.[49]
Management
Some maternal deaths can be prevented through medication use. Injectable oxytocin can be used to prevent death due to postpartum bleeding.[10] Additionally, postpartum infections can be treated using antibiotics. In fact, the use of broad-spectrum antibiotics both for the prevention and treatment of maternal infection is common in low-income countries.[50] Maternal death due to eclampsia can also be prevented through the use of medications such as magnesium sulfate.[10]
Many complications can be managed with procedures and/or surgery if there is access to a qualified surgeon and appropriate facilities and supplies. For example, the contents of the uterus can be cleaned if there is concern for remaining pregnancy tissue or infection. If there is concern for excess bleeding, special ties, stitches or tools (Bakri Balloon) can be placed if there is concern for excess bleeding.[51]
Public health
.jpg.webp)
A public health approach to addressing maternal mortality includes gathering information on the scope of the problem, identifying key causes, and implementing interventions, both prior to pregnancy and during pregnancy, to combat those causes and prevent maternal mortality.[52]
Public health has a role to play in the analysis of maternal death. One important aspect in the review of maternal death and its causes are Maternal Mortality Review Committees or Boards. The goal of these review committees are to analyze each maternal death and determine its cause. After this analysis, the information can be combined in order to determine specific interventions that could lead to preventing future maternal deaths. These review boards are generally comprehensive in their analysis of maternal deaths, examining details that include mental health factors, public transportation, chronic illnesses, and substance use disorders. All of this information can be combined to give a detailed picture of what is causing maternal mortality and help to determine recommendations to reduce their impact.[53]
Many states within the US are taking Maternal Mortality Review Committees a step further and are collaborating with various professional organizations to improve quality of perinatal care. These teams of organizations form a "perinatal quality collaborative" (PQC) and include state health departments, the state hospital association and clinical professionals such as doctors and nurses. These PQCs can also involve community health organizations, Medicaid representatives, Maternal Mortality Review Committees and patient advocacy groups. By involving all of these major players within maternal health, the goal is to collaborate and determine opportunities to improve quality of care. Through this collaborative effort, PQCs can aim to make impacts on quality both at the direct patient care level and through larger system devices like policy. It is thought that the institution of PQCs in California was the main contributor to the maternal mortality rate decreasing by 50% in the years following. The PQC developed review guides and quality improvement initiatives aimed at the most preventable and prevalent maternal deaths: those due to bleeding and high blood pressure. Success has also been observed with PQCs in Illinois and Florida.[54]
Several interventions prior to pregnancy have been recommended in efforts to reduce maternal mortality. Increasing access to reproductive healthcare services, such as family planning services and safe abortion practices, is recommended in order to prevent unintended pregnancies.[52] Several countries, including India, Brazil, and Mexico, have seen some success in efforts to promote the use of reproductive healthcare services.[55] Other interventions include high quality sex education, which includes pregnancy prevention and sexually transmitted infection (STI) prevention and treatment. By addressing STIs, this not only reduces perinatal infections, but can also help reduce ectopic pregnancy caused by STIs.[56] Adolescents are between two and five times more likely to suffer from maternal mortality than a female twenty years or older. Access to reproductive services and sex education could make a large impact, specifically on adolescents, who are generally uneducated in regards to carrying a healthy pregnancy. Education level is a strong predictor of maternal health as it gives women the knowledge to seek care when it is needed.[52] Public health efforts can also intervene during pregnancy to improve maternal outcomes. Areas for intervention have been identified in access to care, public knowledge, awareness about signs and symptoms of pregnancy complications, and improving relationships between healthcare professionals and expecting mothers.[56]
Access to care during pregnancy is a significant issue in the face of maternal mortality. "Access" encompasses a wide range of potential difficulties including costs, location of healthcare services, availability of appointments, availability of trained health care workers, transportation services, and cultural or language barriers that could inhibit a woman from receiving proper care.[56] For women carrying a pregnancy to term, access to necessary antenatal (prior to delivery) healthcare visits is crucial to ensuring healthy outcomes. These antenatal visits allow for early recognition and treatment of complications, treatment of infections and the opportunity to educate the expecting mother on how to manage her current pregnancy and the health advantages of spacing pregnancies apart.[52]
Access to birth at a facility with a skilled healthcare provider present has been associated with safer deliveries and better outcomes.[52] The two areas bearing the largest burden of maternal mortality, Sub-Saharan Africa and South Asia, also had the lowest percentage of births attended by a skilled provider, at just 45% and 41% respectively.[57] Emergency obstetric care is also crucial in preventing maternal mortality by offering services like emergency cesarean sections, blood transfusions, antibiotics for infections and assisted vaginal delivery with forceps or vacuum.[52] In addition to physical barriers that restrict access to healthcare, financial barriers also exist. Close to one out of seven women of child-bearing age have no health insurance. This lack of insurance impacts access to pregnancy prevention, treatment of complications, as well as perinatal care visits contributing to maternal mortality.[58]
By increasing public knowledge and awareness through health education programs about pregnancy, including signs of complications that need addressed by a healthcare provider, this will increase the likelihood of an expecting mother to seek help when it is necessary.[56] Higher levels of education have been associated with increased use of contraception and family planning services as well as antenatal care.[59] Addressing complications at the earliest sign of a problem can improve outcomes for expecting mothers, which makes it extremely important for a pregnant woman to be knowledgeable enough to seek healthcare for potential complications.[52] Improving the relationships between patients and the healthcare system as a whole will make it easier for a pregnant woman to feel comfortable seeking help. Good communication between patients and providers, as well as cultural competence of the providers, could also assist in increasing compliance with recommended treatments.[56]
Another important preventive measure being implemented is specialized education for mothers. Doctors and medical professionals providing simple information to women, especially women in lower socioeconomic areas will decrease the miscommunication that often occurs between doctors and patients.[60] Training health care professionals will be another important aspect in decreasing the rate of maternal death,[61] "The study found that white medical students and residents often believed incorrect and sometimes 'fantastical' biological fallacies about racial differences in patients. For these assumptions, researchers blamed not individual prejudice but deeply ingrained unconscious stereotypes about people of color, as well as physicians’ difficulty in empathizing with patients whose experiences differ from their own."[62]
Policy
The biggest global policy initiative for maternal health came from the United Nations' Millennium Declaration which created the Millennium Development Goals. In 2012, this evolved at the United Nations Conference on Sustainable Development to become the Sustainable Development Goals (SDGs) with a target year of 2030. The SDGs are 17 goals that call for global collaboration to tackle a wide variety of recognized problems. Goal 3 is focused on ensuring health and well-being for people of all ages.[63] A specific target is to achieve a global maternal mortality ratio of less than 70 per 100,000 live births. So far, specific progress has been made in births attended by a skilled provider, now at 80% of births worldwide compared with 62% in 2005.[64]
Countries and local governments have taken political steps in reducing maternal deaths. Researchers at the Overseas Development Institute studied maternal health systems in four apparently similar countries: Rwanda, Malawi, Niger, and Uganda.[65] In comparison to the other three countries, Rwanda has an excellent recent record of improving maternal death rates. Based on their investigation of these varying country case studies, the researchers conclude that improving maternal health depends on three key factors:
- reviewing all maternal health-related policies frequently to ensure that they are internally coherent;
- enforcing standards on providers of maternal health services;
- any local solutions to problems discovered should be promoted, not discouraged.
In terms of aid policy, proportionally, aid given to improve maternal mortality rates has shrunken as other public health issues, such as HIV/AIDS and malaria have become major international concerns.[66] Maternal health aid contributions tend to be lumped together with newborn and child health, so it is difficult to assess how much aid is given directly to maternal health to help lower the rates of maternal mortality. Regardless, there has been progress in reducing maternal mortality rates internationally.[67]
In countries where abortion practices are not considered legal, it is necessary to look at the access that women have to high-quality family planning services, since some of the restrictive policies around abortion could impede access to these services. These policies may also affect the proper collection of information for monitoring maternal health around the world.[19]
Epidemiology
%252C_OWID.svg.png.webp)
Maternal deaths and disabilities are leading contributors in women's disease burden with an estimated 303,000 women killed each year in childbirth and pregnancy worldwide.[69] The global rate in 2017 is 211 maternal deaths per 100,000 live births and 45% of postpartum deaths occur within 24 hours.[70] Ninety-nine percent of maternal deaths occur in low-resource countries.[10]
At a country level, India (19% or 56,000) and Nigeria (14% or 40,000) accounted for roughly one third of the maternal deaths in 2010.[71] Democratic Republic of the Congo, Pakistan, Sudan, Indonesia, Ethiopia, United Republic of Tanzania, Bangladesh and Afghanistan accounted for between 3 and 5 percent of maternal deaths each.[41] These ten countries combined accounted for 60% of all the maternal deaths in 2010 according to the United Nations Population Fund report. Countries with the lowest maternal deaths were Greece, Iceland, Poland, and Finland.[72]
As of 2017, countries in Southeast Asia and Sub-Saharan Africa account for approximately 86% of all maternal death in the world. Sub-Saharan African countries accounted for about two-thirds of the global maternal deaths and Southeast Asian countries accounted for approximately one-fifth. Since 2000, Southeast Asian countries have seen a significant decrease in maternal mortality with an overall decrease in maternal mortality of almost 60%.[73] Sub-Saharan Africa also saw an almost 40% decrease in maternal mortality between 2000 and 2017. As of 2017, the countries with the highest maternal mortality rates included South Sudan, Somalia, Central African Republic, Yemen, Syria, South Sudan, and the Democratic Republic of the Congo. The numbers for maternal mortality in these countries are likely affect by the political and civil unrest that these countries are facing.[73]
Significant progress has been made since the United Nations made the reduction of maternal mortality part of the Millennium Development Goals (MDGs) in 2000.[74]: 1066 Bangladesh, for example, cut the number of deaths per live births by almost two-thirds from 1990 to 2015. A further reduction of maternal mortality is now part of the Agenda 2030 for sustainable development. The United Nations has more recently developed a list of goals termed the Sustainable Development Goals. The target of the third Sustainable Development Goal (SDG) is to reduce the global maternal mortality rate (MMR) to less than 70 per 100,000 live births by 2030.[75] Some of the specific aims of the Sustainable Development Goals are to prevent unintended pregnancies by ensuring more women have access to contraceptives, as well as providing women who become pregnant with a safe environment for delivery with respectful and skilled care. This initiative also included access to emergency services for women who developed complications during delivery.[6]
The WHO has developed a global goal to end preventable death related to maternal mortality.[32] A major goal of this strategy is to identify and address the causes of maternal and reproductive morbidities and mortalities, as well as disabilities related to maternal health outcomes. Their strategy aims to address inequalities in access to reproductive, maternal, and newborn services, as well as the quality of care with universal health coverage. The WHO strategy also aims to ensure quality data collection in order to better respond to the needs of women and girls while improving the equity and quality of care provided to women.
Variation within countries
There are significant maternal mortality intra country variations, especially in nations with large equality gaps in income and education and high healthcare disparities. Women living in rural areas experience higher maternal mortality than women living in urban and sub-urban centers because[76] those living in wealthier households, having higher education, or living in urban areas, have higher use of healthcare services than their poorer, less-educated, or rural counterparts.[77] There are also racial and ethnic disparities in maternal health outcomes which increases maternal mortality in marginalized groups.[78]
By country
| Country | Maternal Mortality Ratio (2017) by Country All data is from the World Bank.[79][80] |
|---|---|
| Italy | 2 |
| Spain | 4 |
| Sweden | 4 |
| Japan | 5 |
| Australia | 6 |
| Germany | 7 |
| UK | 7 |
| France | 8 |
| New Zealand | 9 |
| Canada | 10 |
| South Korea | 11 |
| Russia | 17 |
| US | 19 |
| Mexico | 33 |
| China | 29 |
| South Africa | 119 |
| India | 145 |
| Ghana | 308 |
In the year 2017, 810 women died from preventable causes related to pregnancy and birth per day which totaled to approximately 295,000 maternal deaths that year alone. It was also estimated that 94% of maternal deaths occurred in low-resource countries in the same year.[81]
In a retrospective study done across several countries in 2007, the cause of death and causal relationship to the mode of delivery in pregnant women was examined from the years 2000 to 2006. It was discovered that the excess maternal death rate of women who experienced a pulmonary embolism was casually related to undergoing a cesarean delivery. There was also an association found between neuraxial anesthesia, more commonly known as an epidural, and an increased risk for an epidural hematoma. Both of these risks could be reduced by the institution of graduated compression, whether by compression stockings or a compression device. There is also speculation that eliminating the concept of elective cesarean sections in the United States would significantly lower the maternal death rate.
Related terms
Severe maternal morbidity
Severe maternal morbidity (SMM) is an unanticipated acute or chronic health outcome after labor and delivery that detrimentally affects a woman's health. Severe Maternal Morbidity (SMM) includes any unexpected outcomes from labor or delivery that cause both short and long-term consequences to the mother's overall health.[82] There are nineteen total indicators used by the CDC to help identify SMM, with the most prevalent indicator being a blood transfusion.[83] Other indicators include an acute myocardial infarction ("heart attack"), aneurysm, and kidney failure. All of this identification is done by using ICD-10 codes, which are disease identification codes found in hospital discharge data.[84] Using these definitions that rely on these codes should be used with careful consideration since some may miss some cases, have a low predictive value, or may be difficult for different facilities to operationalize.[31] There are certain screening criteria that may be helpful and are recommended through the American College of Obstetricians and Gynecologists as well as the Society for Maternal-Fetal Medicine (SMFM). These screening criteria for SMM are for transfusions of four or more units of blood and admission of a pregnant woman or a postpartum woman to an ICU facility or unit.[31]
The greatest proportion of women with SMM are those who require a blood transfusion during delivery, mostly due to excessive bleeding. Blood transfusions given during delivery due to excessive bleeding has increased the rate of mothers with SMM.[82] The rate of SMM has increased almost 200% between 1993 (49.5 per 100,000 live births) and 2014 (144.0 per 100,000 live births). This can be seen with the increased rate of blood transfusions given during delivery, which increased from 1993 (24.5 per 100,000 live births) to 2014 (122.3 per 100,000 live births).[82]
In the United States, severe maternal morbidity has increased over the last several years, impacting greater than 50,000 women in 2014 alone. There is no conclusive reason for this dramatic increase. It is thought that the overall state of health for pregnant women is impacting these rates. For example, complications can derive from underlying chronic medical conditions like diabetes, obesity, HIV/AIDS, and high blood pressure. These underlying conditions are also thought to lead to increased risk of maternal mortality.[85]
The increased rate for SMM can also be indicative of potentially increased rates for maternal mortality, since without identification and treatment of SMM, these conditions would lead to increased maternal death rates. Therefore, diagnosis of SMM can be considered a "near miss" for maternal mortality.[31] With this consideration, several different expert groups have urged obstetric hospitals to review SMM cases for opportunities that can lead to improved care, which in turn would lead to improvements with maternal health and a decrease in the number of maternal deaths.
See also
- Child health
- Confidential Enquiry into Maternal Deaths in the UK
- Infant mortality
- List of women who died in childbirth
- Maternal mortality in fiction
- Maternal near miss
- Obstetric transition
- Perinatal mortality
- Black maternal mortality in the United States
References
- 1 2 3 4 5 "Indicator Metadata Registry Details". www.who.int. Archived from the original on 2021-11-08. Retrieved 2021-11-08.
- 1 2 "Pregnancy Mortality Surveillance System - Pregnancy - Reproductive Health". CDC. 25 November 2020. Archived from the original on 25 May 2019. Retrieved 22 March 2022.
- ↑ "Pregnancy-Related Deaths | CDC". www.cdc.gov. 2019-02-26. Archived from the original on 2021-11-12. Retrieved 2021-11-08.
- 1 2 3 Atrash, H. K.; Rowley, D.; Hogue, C. J. (February 1992). "Maternal and perinatal mortality". Current Opinion in Obstetrics & Gynecology. 4 (1): 61–71. doi:10.1097/00001703-199202000-00009. ISSN 1040-872X. PMID 1543832. S2CID 32268911. Archived from the original on 2021-11-07. Retrieved 2022-03-22.
- ↑ Maternal Mortality Ratio vs Maternal Mortality Rate Archived 2017-02-02 at the Wayback Machine on Population Research Institute website
- 1 2 3 4 5 6 7 8 9 10 11 12 13 "Maternal health". United Nations Population Fund. Archived from the original on 2020-11-29. Retrieved 2017-01-29.
- 1 2 3 4 Ozimek, John A.; Kilpatrick, Sarah J. (2018-06-01). "Maternal Mortality in the Twenty-First Century". Obstetrics and Gynecology Clinics. 45 (2): 175–186. doi:10.1016/j.ogc.2018.01.004. ISSN 0889-8545. PMID 29747724. S2CID 13683555. Archived from the original on 2022-03-23. Retrieved 2022-03-22.
- ↑ GBD 2013 Mortality Causes of Death Collaborators (January 2015). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- ↑ GBD 2013 Mortality Causes of Death Collaborators (January 2015). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- 1 2 3 4 "Maternal mortality: Fact sheet N°348". World Health Organization. WHO. Archived from the original on 30 September 2015. Retrieved 20 June 2014.
- ↑ "UpToDate". www.uptodate.com. Archived from the original on 2022-03-23. Retrieved 2021-11-12.
- ↑ Eiland, Elosha; Nzerue, Chike; Faulkner, Marquetta (2012). "Preeclampsia 2012". Journal of Pregnancy. 2012: 586578. doi:10.1155/2012/586578. ISSN 2090-2727. PMC 3403177. PMID 22848831.
- ↑ "CDC Reports Infection as a Major Cause of Maternal Death". Sepsis Alliance. Archived from the original on 2021-11-13. Retrieved 2021-11-13.
- ↑ Philpott, R. H. (December 1982). "Obstructed labour". Clinics in Obstetrics and Gynaecology. 9 (3): 625–640. doi:10.1016/S0306-3356(21)00535-5. ISSN 0306-3356. PMID 7172577. Archived from the original on 2021-11-17. Retrieved 2022-03-22.
- ↑ "Blood Clots: Risks, Symptoms, Treatments, Prevention". Cleveland Clinic. Archived from the original on 2021-11-13. Retrieved 2021-11-13.
- 1 2 3 Raymond, Elizabeth G.; Grimes, David A. (February 2012). "The Comparative Safety of Legal Induced Abortion and Childbirth in the United States". Obstetrics & Gynecology. 119 (2 Part 1): 215–219. doi:10.1097/AOG.0b013e31823fe923. ISSN 0029-7844. PMID 22270271. S2CID 25534071. Archived from the original on 2021-11-13. Retrieved 2022-03-22.
- 1 2 Berer, Marge (June 2017). "Abortion Law and Policy Around the World". Health and Human Rights. 19 (1): 13–27. ISSN 1079-0969. PMC 5473035. PMID 28630538.
- ↑ "Legality and Safety". Guttmacher Institute. Archived from the original on 2021-11-13. Retrieved 2021-11-13.
- 1 2 3 4 5 Dixon-Mueller R, Germain A (January 2007). "Fertility regulation and reproductive health in the Millennium Development Goals: the search for a perfect indicator". American Journal of Public Health. 97 (1): 45–51. doi:10.2105/AJPH.2005.068056. PMC 1716248. PMID 16571693.
- ↑ "Preventing unsafe abortion". www.who.int. Archived from the original on 2019-08-23. Retrieved 2021-11-13.
- ↑ "WHO | Unsafe abortion: global and regional estimates of incidence of unsafe abortion and associated mortality in 2003". WHO. Archived from the original on 2018-04-07. Retrieved 2021-11-13.
- ↑ World Health Organization, Unsafe Abortion: Global and Regional Estimates of the Incidence of Unsafe Abortion and Associated Mortality in 2000, 4th ed.
- 1 2 Souto SL, Ferreira JD, Ramalho NM, de Lima CL, Ferreira TM, Maciel GM, et al. (2017-07-04). "Nursing Care For Women In Situation Of Unsafe Abortion". International Archives of Medicine. 10. doi:10.3823/2484.
- 1 2 Haddad LB, Nour NM (2009). "Unsafe abortion: unnecessary maternal mortality". Reviews in Obstetrics & Gynecology. 2 (2): 122–6. PMC 2709326. PMID 19609407.
- 1 2 3 4 Gerdts C, Tunçalp O, Johnston H, Ganatra B (September 2015). "Measuring abortion-related mortality: challenges and opportunities". Reproductive Health. 12 (1): 87. doi:10.1186/s12978-015-0064-1. PMC 4572614. PMID 26377189.
- ↑ Bongaarts J, Westoff CF (September 2000). "The potential role of contraception in reducing abortion". Studies in Family Planning. 31 (3): 193–202. doi:10.1111/j.1728-4465.2000.00193.x. PMID 11020931. S2CID 14424881. Archived from the original on 2022-03-23. Retrieved 2022-03-22.
- ↑ Khlat M, Ronsmans C (February 2000). "Deaths attributable to childbearing in Matlab, Bangladesh: indirect causes of maternal mortality questioned". American Journal of Epidemiology. 151 (3): 300–6. doi:10.1093/oxfordjournals.aje.a010206. PMID 10670555.
- ↑ The most common causes of anemia/anaemia are poor nutrition, iron, and other micronutrient deficiencies, which are in addition to malaria, hookworm, and schistosomiasis (2005 WHO report p45).
- ↑ Nair, Manisha; Nelson-Piercy, Catherine; Knight, Marian (March 2017). "Indirect maternal deaths: UK and global perspectives". Obstetric Medicine. 10 (1): 10–15. doi:10.1177/1753495X16689444. ISSN 1753-495X. PMC 5405948. PMID 28491125.
- 1 2 Molina RL, Pace LE (November 2017). "A Renewed Focus on Maternal Health in the United States". The New England Journal of Medicine. 377 (18): 1705–1707. doi:10.1056/NEJMp1709473. PMID 29091560.
- 1 2 3 4 Kilpatrick SK, Ecker JL (September 2016). "Severe maternal morbidity: screening and review". American Journal of Obstetrics and Gynecology. 215 (3): B17–22. doi:10.1016/j.ajog.2016.07.050. PMID 27560600. Cited in CDC 2017 report.
- 1 2 3 4 5 "Maternal mortality". World Health Organisation. Archived from the original on 2015-09-30. Retrieved 2022-03-22.
- 1 2 Conde-Agudelo A, Belizán JM, Lammers C (February 2005). "Maternal-perinatal morbidity and mortality associated with adolescent pregnancy in Latin America: Cross-sectional study". American Journal of Obstetrics and Gynecology. 192 (2): 342–9. doi:10.1016/j.ajog.2004.10.593. PMID 15695970.
- ↑ Upadhyay, Priti; Liabsuetrakul, Tippawan; Shrestha, Amir Babu; Pradhan, Neelam (December 2014). "Influence of family members on utilization of maternal health care services among teen and adult pregnant women in Kathmandu, Nepal: a cross sectional study". Reproductive Health. 11 (1): 92. doi:10.1186/1742-4755-11-92. ISSN 1742-4755. PMC 4290463. PMID 25539759.
- ↑ Morgan KJ, Eastwood JG (January 2014). "Social determinants of maternal self-rated health in South Western Sydney, Australia". BMC Research Notes. 7 (1): 51. doi:10.1186/1756-0500-7-51. PMC 3899616. PMID 24447371.
- 1 2 3 4 "WHO | Applying the lessons of maternal mortality reduction to global emergency health". WHO. Archived from the original on June 6, 2015. Retrieved 2019-08-02.
- 1 2 3 4 Thaddeus, Sereen; Maine, Deborah (1994-04-01). "Too far to walk: Maternal mortality in context". Social Science & Medicine. 38 (8): 1091–1110. doi:10.1016/0277-9536(94)90226-7. ISSN 0277-9536. PMID 8042057.
- ↑ Barnes-Josiah, Debora; Myntti, Cynthia; Augustin, Antoine (1998-04-15). "The "three delays" as a framework for examining maternal mortality in Haiti". Social Science & Medicine. 46 (8): 981–993. doi:10.1016/S0277-9536(97)10018-1. ISSN 0277-9536. PMID 9579750.
- 1 2 3 "MME Info". maternalmortalitydata.org. Archived from the original on October 14, 2013.
- 1 2 "WHO | The lifetime risk of maternal mortality: concept and measurement". WHO. Archived from the original on August 5, 2011. Retrieved 2019-08-01.
- 1 2 3 4 [UNICEF, W. (2012). UNFPA, World Bank (2012) Trends in maternal mortality: 1990 to 2010 Archived 2018-02-05 at the Wayback Machine. WHO, UNICEF.]
- ↑ "The Sisterhood Method for Estimating Maternal Mortality: Guidance notes for potential users" (PDF). Who.org. World Health Organization. Archived (PDF) from the original on 2 April 2015. Retrieved 13 March 2015.
- ↑ Lee KS, Park SC, Khoshnood B, Hsieh HL, Mittendorf R (September 1997). "Human development index as a predictor of infant and maternal mortality rates". The Journal of Pediatrics. 131 (3): 430–3. doi:10.1016/S0022-3476(97)80070-4. PMID 9329421.
- ↑ Venös tromboembolism (VTE) - Guidelines for treatment in C counties. Bengt Wahlström, Emergency department, Uppsala Academic Hospital. January 2008
- ↑ "Maternal Morality Comparison: USA vs. Israel vs. Europe". Juravin. 19 January 2019. Retrieved 2 July 2019.
{{cite web}}: CS1 maint: url-status (link) - ↑ World Health Organization and partner organizations (2013). Maternal death surveillance and response: technical guidance. Information for action to prevent maternal death. World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland: WHO press. p. 128. ISBN 978-92-4-150608-3. Archived from the original on October 13, 2014. Retrieved 4 October 2017.
{{cite book}}: CS1 maint: location (link) - ↑ "Maternal Health in the United States". Maternal Health Task Force. 2015-08-14. Archived from the original on 2018-11-01. Retrieved 2018-11-09.
- ↑ Miller S, Turan JM, Dau K, Fathalla M, Mourad M, Sutherland T, et al. (2007). "Use of the non-pneumatic anti-shock garment (NASG) to reduce blood loss and time to recovery from shock for women with obstetric haemorrhage in Egypt". Global Public Health. 2 (2): 110–24. doi:10.1080/17441690601012536. PMID 19280394. S2CID 11392183. Archived from the original on 2022-03-23. Retrieved 2022-03-22. (NASG)
- ↑ Akhter S, Begum MR, Kabir Z, Rashid M, Laila TR, Zabeen F (September 2003). "Use of a condom to control massive postpartum hemorrhage" (PDF). MedGenMed. 5 (3): 38. PMID 14600674. Archived (PDF) from the original on 2016-10-08. Retrieved 2022-03-22.
- ↑ Information, National Center for Biotechnology; Pike, U. S. National Library of Medicine 8600 Rockville; MD, Bethesda; Usa, 20894 (2015). Background. World Health Organization. Archived from the original on 2022-03-23. Retrieved 2022-03-22.
{{cite book}}: CS1 maint: numeric names: authors list (link) - ↑ Shah, Monjri; Wright, Jason D. (April 2009). "Surgical intervention in the management of postpartum hemorrhage". Seminars in Perinatology. 33 (2): 109–115. doi:10.1053/j.semperi.2008.12.006. ISSN 1558-075X. PMID 19324240. Archived from the original on 2021-11-13. Retrieved 2022-03-22.
- 1 2 3 4 5 6 7 Rai SK, Anand K, Misra P, Kant S, Upadhyay RP (2012). "Public health approach to address maternal mortality". Indian Journal of Public Health. 56 (3): 196–203. doi:10.4103/0019-557x.104231. PMID 23229211.
- ↑ "Review to Action". reviewtoaction.org. Archived from the original on 2018-11-21. Retrieved 2018-11-20.
- ↑ Main EK (June 2018). "Reducing Maternal Mortality and Severe Maternal Morbidity Through State-based Quality Improvement Initiatives". Clinical Obstetrics and Gynecology. 61 (2): 319–331. doi:10.1097/grf.0000000000000361. PMID 29505420. S2CID 3673030.
- ↑ GBD 2015 Maternal Mortality Collaborators (October 2016). "Global, regional, and national levels of maternal mortality, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1775–1812. doi:10.1016/S0140-6736(16)31470-2. PMC 5224694. PMID 27733286.
- 1 2 3 4 5 Berg C, Danel I, Atrash H, Zane S, Bartlett L, eds. (2001). Strategies to reduce pregnancy-related deaths: from identification and review to action (PDF). Atlanta: Centers for Disease Control and Prevention. Archived (PDF) from the original on 2021-07-01. Retrieved 2022-03-22.
- ↑ "The State of the World's Children 2009: Maternal and newborn health" (PDF). United Nations Children's Fund (UNICEF). December 2008. Archived (PDF) from the original on 2021-06-11. Retrieved 2022-03-22.
- ↑ Lu MC (September 2018). "Reducing Maternal Mortality in the United States". JAMA. 320 (12): 1237–1238. doi:10.1001/jama.2018.11652. PMID 30208484. S2CID 205095772.
- ↑ Weitzman A (May 2017). "The effects of women's education on maternal health: Evidence from Peru". Social Science & Medicine. 180: 1–9. doi:10.1016/j.socscimed.2017.03.004. PMC 5423409. PMID 28301806.
- ↑ Vilda, Dovile; Wallace, Maeve; Dyer, Lauren; Harville, Emily; Theall, Katherine (2019-12-01). "Income inequality and racial disparities in pregnancy-related mortality in the US". SSM - Population Health. 9: 100477. doi:10.1016/j.ssmph.2019.100477. ISSN 2352-8273. PMC 6734101. PMID 31517017.
- ↑ Roth, Louise Marie; Henley, Megan M. (2012). "Unequal Motherhood: Racial-Ethnic and Socioeconomic Disparities in Cesarean Sections in the United States". Social Problems. 59 (2): 207–227. doi:10.1525/sp.2012.59.2.207. ISSN 0037-7791. JSTOR 10.1525/sp.2012.59.2.207.
- ↑ Villarosa, Linda (April 2018). "Why America's Black Mothers and Babies Are in a Life-or-Death Crisis" (PDF). The New York Times Magazine. Archived (PDF) from the original on 2021-07-01. Retrieved 2022-03-22.
- ↑ "Sustainable Development Goals .:. Sustainable Development Knowledge Platform". sustainabledevelopment.un.org. Archived from the original on 2020-07-23. Retrieved 2018-11-25.
- ↑ "Goal 3 .:. Sustainable Development Knowledge Platform". sustainabledevelopment.un.org. Archived from the original on 2018-11-27. Retrieved 2018-11-25.
- ↑ Chambers V, Booth D (2012). "Delivering maternal health: why is Rwanda doing better than Malawi, Niger and Uganda?" (Briefing Paper). Overseas Development Institute.
{{cite web}}: CS1 maint: url-status (link) - ↑ "Development assistance for health by health focus area (Global), 1990-2009, interactive treemap". Institute for Health Metrics and Evaluation. Archived from the original on 2014-03-17.
- ↑ "Progress in maternal and child mortality by country, age, and year (Global), 1990-2011". Archived from the original on 2014-03-17.
- ↑ "Maternal mortality ratio". Our World in Data. Archived from the original on 26 September 2019. Retrieved 16 February 2020.
- ↑ "Trends in maternal mortality: 1990 to 2015". World Health Organization. November 2015. p. 16. Archived from the original on 2022-03-21. Retrieved 2022-03-22.
- ↑ Nour NM (2008). "An introduction to maternal mortality". Reviews in Obstetrics & Gynecology. 1 (2): 77–81. PMC 2505173. PMID 18769668.
- ↑ "WHO | Facility-based maternal death review in Nigeria". WHO. Archived from the original on May 23, 2017. Retrieved 2020-09-24.
- ↑ "Comparison: Maternal Mortality Rate". The World Factbook. Central Intelligence Agency. Archived from the original on 2019-04-30. Retrieved 2022-03-22.
- 1 2 "Maternal mortality". www.who.int. Archived from the original on 2021-04-10. Retrieved 2021-04-12.
- ↑ Khan KS, Wojdyla D, Say L, Gülmezoglu AM, Van Look PF (April 2006). "WHO analysis of causes of maternal death: a systematic review" (PDF). Lancet. 367 (9516): 1066–1074. doi:10.1016/S0140-6736(06)68397-9. PMID 16581405. S2CID 2190885. Archived from the original (PDF) on 2017-10-31. Retrieved 2022-03-22.
- ↑ "Health - United Nations Sustainable Development". United Nations. Archived from the original on 2019-09-20. Retrieved 2022-03-22.
- ↑ "WHO Maternal Health". WHO. Archived from the original on 2015-09-30. Retrieved 2022-03-22.
- ↑ Wang W, Alva S, Wang S, Fort A (2011). "Levels and trends in the use of maternal health services in developing countries" (PDF). Calverton, MD: ICF Macro. p. 85. (DHS Comparative Reports 26). Archived (PDF) from the original on 2018-05-15. Retrieved 2022-03-22.
- ↑ Lu MC, Halfon N (March 2003). "Racial and ethnic disparities in birth outcomes: a life-course perspective". Maternal and Child Health Journal. 7 (1): 13–30. doi:10.1023/A:1022537516969. PMID 12710797. S2CID 19973932.
- ↑ "Maternal mortality ratio (modeled estimate, per 100,000 live births) | Data". Archived from the original on 2018-10-14. Retrieved 2018-06-27.
- ↑ What’s killing America’s new mothers? Archived 2022-03-03 at the Wayback Machine By Annalisa Merelli. October 29, 2017. Quartz. "The dire state of US data collection on maternal health and mortality is also distressing. Until the early 1990s, death certificates did not note if a woman was pregnant or had recently given birth when she died. It took until 2017 for all US states to add that check box to their death certificates."
- ↑ Clark, Steven (July 2008). "Maternal death in the 21st century: causes, prevention, and relationship to cesarean delivery". American Journal of Obstetrics and Gynecology. 199 (1): 36.1–36.5. doi:10.1016/j.ajog.2008.03.007. PMID 18455140. Retrieved November 12, 2020.
- 1 2 3 "Severe Maternal Morbidity in the United States". CDC. 2017-11-27. Archived from the original on 2018-11-15. Retrieved 2022-03-22.
- ↑ "Severe Maternal Morbidity in the United States | Pregnancy | Reproductive Health |CDC". www.cdc.gov. 2017-11-27. Archived from the original on 2018-11-15. Retrieved 2018-11-20.
- ↑ "Severe Maternal Morbidity Indicators and Corresponding ICD Codes during Delivery Hospitalizations". www.cdc.gov. 2018-08-21. Archived from the original on 2018-11-20. Retrieved 2018-11-20.
- ↑ Campbell KH, Savitz D, Werner EF, Pettker CM, Goffman D, Chazotte C, Lipkind HS (September 2013). "Maternal morbidity and risk of death at delivery hospitalization". Obstetrics and Gynecology. 122 (3): 627–33. doi:10.1097/aog.0b013e3182a06f4e. PMID 23921870. S2CID 25347341.
Bibliography
- World Health Organization (2014). Trends in maternal mortality: 1990 to 2013 (PDF). WHO. ISBN 978-92-4-150722-6. Archived (PDF) from the original on 15 January 2020. Retrieved 2 August 2016.
External links
| Classification |
|---|
- The World Health Report 2005 – Make Every Mother and Child Count Archived 2022-03-20 at the Wayback Machine