Drowning
| Drowning | |
|---|---|
 | |
| Vasily Perov: The Drowned, 1867 painting | |
| Specialty | Critical care medicine |
| Symptoms | Event: Often occurs silently with a person found unconscious[1][2] After rescue: Breathing problems, vomiting, confusion, unconscious[2][3] |
| Complications | Hypothermia, aspiration of vomit, acute respiratory distress syndrome[4] |
| Usual onset | Rapid[3] |
| Risk factors | Alcohol use, epilepsy, low socioeconomic status, access to water[5] |
| Diagnostic method | Based on symptoms[3] |
| Differential diagnosis | Suicide, seizure, hypoglycemia, heart arrhythmia[2] |
| Prevention | Fencing pools, teaching children to swim, safe boating practices[5][6] |
| Treatment | Rescue breathing, CPR, mechanical ventilation[7] |
| Medication | Oxygen therapy, intravenous fluids, vasopressors[7] |
| Frequency | 4.5 million (2015)[8] |
| Deaths | 324,000 (2015)[9] |
Drowning is defined as respiratory impairment as a result of being in or under a liquid.[7][10] Drowning typically occurs silently, with only a few people able to wave their hands or call for help.[1] Symptoms following rescue may include breathing problems, vomiting, confusion, or unconsciousness.[2][3] Occasionally symptoms may not appear until up to six hours afterwards.[3] Drowning may be complicated by low body temperature, aspiration of vomit, or acute respiratory distress syndrome.[4][11]
Drowning is more common when the weather is warm and among those with frequent access to water.[4][5] Risk factors include alcohol use, epilepsy, and low socioeconomic status.[5] Common locations of drowning include swimming pools, bathtubs, natural bodies of water, and buckets.[3][7] Initially the person holds their breath, which is followed by laryngospasm, and then low oxygen levels.[4] Significant amounts of water usually only enter the lungs later in the process.[4] It may be classified into three types: drowning with death, drowning with ongoing health problems, and drowning with no ongoing health problems.[10]
Efforts to prevent drowning include teaching children to swim, safe boating practices, and limiting or removing access to water such as by fencing pools.[5][6] Treatment of those who are not breathing should begin with opening the airway and providing five breaths.[7] In those whose heart is not beating and who have been underwater for less than an hour CPR is recommended.[7] Survival rates are better among those with a shorter time under the water.[7] Among children who survive, poor outcomes occur in about 7.5% of cases.[7]
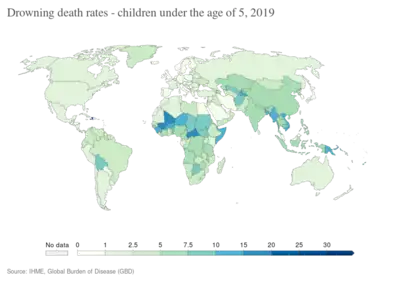
In 2015, there were an estimated 4.5 million cases of unintentional drowning worldwide.[8] That year, there were 324,000 drowning deaths, making it the third leading cause from unintentional injuries after falls and motor vehicle collisions.[9] Of these deaths, 56,000 occurred in children less than five years old.[9] Drowning accounts for 7% of all injury related deaths, with more than 90% of these deaths occurring in developing countries.[5][9] Drowning occurs more frequently in males and the young.[5]
Signs and symptoms
Drowning is most often quick and unspectacular. Its media depictions as a loud, violent struggle have much more in common with distressed non-swimmers, who may well drown but have not yet begun to do so. In particular, an asphyxiating person is seldom able to call for help.[12] The instinctive drowning response covers many signs or behaviors associated with drowning or near-drowning:
- Head low in the water, mouth at water level
- Head tilted back with mouth open
- Eyes glassy and empty, unable to focus
- Eyes open, with fear evident on the face
- Hyperventilating or gasping
- Trying to swim in a particular direction but not making headway
- Trying to roll over on the back to float
- Uncontrollable movement of arms and legs, rarely out of the water.
Drowning begins at the point a person is unable to keep their mouth above water; inhalation of water takes place at a later stage.[13] Most people demonstrating the instinctive drowning response do not show obvious prior evidence of distress.[13]
A person drowning is generally unable to call for help, or seek attention, as they cannot obtain enough air. The instinctive drowning response is the final set of autonomic reactions in the 20–60 seconds before sinking underwater, and to the untrained eye can look similar to calm safe behavior.[12][14] Lifeguards and other persons trained in rescue learn to recognize drowning people by watching for these movements.[12]
Cause
Drowning mainly happens due to the inability to swim in a circumstance: lack of skill, state of the waters, physical condition, loss of consciousness, and others. Anxiety can lead to exhaustion, precipitating the drowning.
Approximately 90% of drownings take place in freshwater (rivers, lakes and swimming pools) and 10% in seawater. Drownings in other fluids are rare, and often relate to industrial accidents. In New Zealand's early colonial history, so many settlers died while trying to cross rivers that drowning was known as "The New Zealand death".[15]
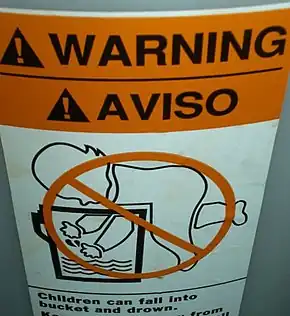
People have drowned in as little as 30 mm of water lying face down.[16] Children have drowned in baths, buckets and toilets; inebriates or those under the influence of drugs have died in puddles.
Drowning can also happen after the drowning incident itself, due to further complications. The inhaled fluid can act as an irritant inside the lungs. Physiological responses to even small quantities include the extrusion of liquid into the lungs (pulmonary edema) over the following hours, but this reduces the ability to exchange air and can lead to a person "drowning in their own body fluid". Certain poisonous vapors or gases (as for example in chemical warfare), or vomit can have a similar effect. The reaction can take place up to 72 hours after the drowning incident, and may lead to a serious condition or death.
Risk factors
Many factors, behavioral and physical, are related to drowning:[17][18]
- Worldwide, drowning is the most common cause of death for persons with seizure disorders, largely in the bathtub (by unintentional injury). People with epilepsy are more likely to die due to accidents such as drowning. However, this risk is especially elevated in low- and middle-income countries compared to high-income countries.[19]
- The use of alcohol increases the risk for drowning across developed and developing nations. Alcohol is involved in approximately 50% of fatal drownings, and 35% of non-fatal drownings.[20] Among adolescents and adults, alcohol use is involved in almost a quarter of emergency department visits for drowning.
- Inability to swim: Participation in formal swimming lessons can reduce the risk of drowning. The optimal age to start the lessons is childhood, between 1 and 4 years old.
- Feeling too tired reduces the swimming performance. This exhaustion can appear because of the anxious movements motivated by fear during drowning. Otherwise, a bad calculation of the own physical capabilities can leave oneself exhausted before reaching the shore.
- Free access to water: Effective barriers prevent young children from gaining access to the water.
- Ineffective supervision: Drowning can occur anywhere there is water, and even in the presence of lifeguards.
- Risk can vary with location depending on age. Children between 1 and 4 usually drown in home swimming pools. Drownings in natural water settings increase with age. More than half of drownings among those 15 years and older occurred in natural water environments.
- Failure to wear life jackets or personal flotation devices was implicated in 88% of the boating related drownings in the US during 2010.
Population groups at risk in the US are:[17]
- Children and young adults: Drowning rates are highest for children under 5 years of age and persons 15–24 years of age.
- Males: Nearly 80% of people who die from drowning are male.
- Minorities: The fatal unintentional drowning rate for African Americans between 2005 and 2009 was significantly higher than that of whites across all ages. The fatal drowning rate of African American children of ages from 5 to 14 is almost three times that of white children in the same age range, and 5.5 times higher in swimming pools. These disparities might be associated with lack of basic swimming skills in some minority populations.
Freediving
Some special causes of drowning can also happen during freediving activities:
- Ascent blackout, also called deep water blackout – caused by latent hypoxia during ascent from depth, where the partial pressure of oxygen in the lungs under pressure at the bottom of a deep freedive is adequate to support consciousness but drops below the blackout threshold as the water pressure decreases on the ascent. It usually strikes upon arriving near the surface as the pressure approaches normal atmospheric pressure.[21]
- Shallow water blackout – caused by hyperventilation prior to swimming or diving. The primary urge to breathe is triggered by rising carbon dioxide (CO2) levels in the bloodstream.[22] The body detects CO2 levels very accurately and relies on this to control breathing.[22] Hyperventilation reduces the carbon dioxide content of the blood but leaves the diver susceptible to sudden loss of consciousness without warning from hypoxia. There is no bodily sensation that warns a diver of an impending blackout, and people (often capable swimmers swimming under the surface in shallow water) become unconscious and drown quietly without alerting anyone to the fact that there is a problem; they are typically found on the bottom.
Pathophysiology
Drowning can be considered as going through four stages:[23]
- Breath-hold under voluntary control until the urge to breathe due to hypercapnia becomes overwhelming
- Fluid is aspirated into the airways and/or swallowed
- Cerebral anoxia stops breathing and aspiration
- Cerebral injury due to anoxia becomes irreversible
Generally, in the early stages of drowning a person holds their breath to prevent water from entering their lungs.[7] When this is no longer possible a small amount of water entering the trachea causes a muscular spasm that seals the airway and prevents further passage of water.[7] If the process is not interrupted, loss of consciousness due to hypoxia is followed rapidly by cardiac arrest.
Oxygen deprivation
A conscious person will hold his or her breath (see Apnea) and will try to access air, often resulting in panic, including rapid body movement. This uses up more oxygen in the blood stream and reduces the time to unconsciousness. The person can voluntarily hold his or her breath for some time, but the breathing reflex will increase until the person tries to breathe, even when submerged.[24]
The breathing reflex in the human body is weakly related to the amount of oxygen in the blood but strongly related to the amount of carbon dioxide (see Hypercapnia). During apnea, the oxygen in the body is used by the cells, and excreted as carbon dioxide. Thus, the level of oxygen in the blood decreases, and the level of carbon dioxide increases. Increasing carbon dioxide levels lead to a stronger and stronger breathing reflex, up to the breath-hold breakpoint, at which the person can no longer voluntarily hold his or her breath. This typically occurs at an arterial partial pressure of carbon dioxide of 55 mm Hg, but may differ significantly between people.
The breath-hold break point can be suppressed or delayed either intentionally or unintentionally. Hyperventilation before any dive, deep or shallow, flushes out carbon dioxide in the blood resulting in a dive commencing with an abnormally low carbon dioxide level; a potentially dangerous condition known as hypocapnia. The level of carbon dioxide in the blood after hyperventilation may then be insufficient to trigger the breathing reflex later in the dive and a blackout may occur without warning and before the diver feels any urgent need to breathe. This can occur at any depth and is common in distance breath-hold divers in swimming pools. Hyperventilation is often used by both deep and distance free-divers to flush out carbon dioxide from the lungs to suppress the breathing reflex for longer. It is important not to mistake this for an attempt to increase the body's oxygen store. The body at rest is fully oxygenated by normal breathing and cannot take on any more. Breath holding in water should always be supervised by a second person, as by hyperventilating, one increases the risk of shallow water blackout because insufficient carbon dioxide levels in the blood fail to trigger the breathing reflex.[25][26]
A continued lack of oxygen in the brain, hypoxia, will quickly render a person unconscious usually around a blood partial pressure of oxygen of 25–30 mmHg.[26] An unconscious person rescued with an airway still sealed from laryngospasm stands a good chance of a full recovery. Artificial respiration is also much more effective without water in the lungs. At this point the person stands a good chance of recovery if attended to within minutes. More than 10% of drownings may involve laryngospasm, but the evidence suggests that it is not usually effective at preventing water from entering the trachea. The lack of water found in lungs during autopsy does not necessarily mean there was no water at the time of drowning, as small amounts of freshwater are readily absorbed into the bloodstream. Hypercarbia and hypoxia both contribute to laryngeal relaxation, after which the airway is effectively open through the trachea. There is also bronchospasm and mucous production in the bronchi associated with laryngospasm, and these may prevent water entry at terminal relaxation.[27]
The hypoxemia and acidosis caused by asphyxia in drowning affect various organs. There can be central nervous system damage, cardiac arhythmias, pulmonary injury, reperfusion injury, and multiple-organ secondary injury with prolonged tissue hypoxia.[28]
A lack of oxygen or chemical changes in the lungs may cause the heart to stop beating. This cardiac arrest stops the flow of blood and thus stops the transport of oxygen to the brain. Cardiac arrest used to be the traditional point of death but at this point there is still a chance of recovery. The brain cannot survive long without oxygen and the continued lack of oxygen in the blood combined with the cardiac arrest will lead to the deterioration of brain cells causing first brain damage and eventually brain death from which recovery is generally considered impossible. The brain will die after approximately six minutes without oxygen at normal body temperature, but hypothermia of the central nervous system may prolong this.
The extent of central nervous system injury to a large extent determines the survival and long term consequences of drowning, In the case of children, most survivors are found within 2 minutes of immersion, and most fatalities are found after 10 minutes or more.[28]
Water aspiration
If water enters the airways of a conscious person, the person will try to cough up the water or swallow it, often inhaling more water involuntarily. When water enters the larynx or trachea, both conscious and unconscious persons experience laryngospasm, in which the vocal cords constrict, sealing the airway. This prevents water from entering the lungs. Because of this laryngospasm, in the initial phase of drowning, water generally enters the stomach and very little water enters the lungs. Though laryngospasm prevents water from entering the lungs, it also interferes with breathing. In most persons, the laryngospasm relaxes some time after unconsciousness and water can then enter the lungs causing a "wet drowning". However, about 7–10% of people maintain this seal until cardiac arrest.[24] This has been called "dry drowning", as no water enters the lungs. In forensic pathology, water in the lungs indicates that the person was still alive at the point of submersion. Absence of water in the lungs may be either a dry drowning or indicates a death before submersion.[29]
Aspirated water that reaches the alveoli destroys the pulmonary surfactant, which causes pulmonary oedema and decreased lung compliance which compromises oxygenation in affected parts of the lungs. This is associated with metabolic acidosis, and secondary fluid and electrolyte shifts. During alveolar fluid exchange, diatoms present in the water may pass through the alveolar wall into the capillaries to be carried to internal organs. Presence of these diatoms may be diagnostic of drowning.
Of people who have survived drowning, almost one third will experience complications such as acute lung injury (ALI) or acute respiratory distress syndrome (ARDS).[30] ALI/ARDS can be triggered by pneumonia, sepsis and water aspiration and are life-threatening disorders that can result in death if not treated promptly.[30] During drowning, aspirated water enters the lung tissues, causes a reduction in alveolar surfactant, obstructs ventilation and triggers a release of inflammatory mediators which ultimately results in hypoxia.[30] Specifically, upon reaching the alveoli, hypotonic liquid found in fresh water dilutes pulmonary surfactant, destroying the substance.[31] Comparatively, aspiration of hypertonic seawater draws liquid from the plasma into the alveoli and similarly causes damage to surfactant by disrupting the alveolar-capillary membrane.[31] Still, there is no clinical difference between salt and freshwater drowning. Once someone has reached definitive care, supportive care strategies such as mechanical ventilation can help to reduce the complications of ALI/ARDS.[30]
Whether a person drowns in fresh water versus salt water makes no difference in the respiratory management or the outcome of the person.[32] People who drown in fresh water may experience worse hypoxemia early in their treatment, however, this initial difference is short-lived and the management of both fresh water and salt water drowning is essentially the same.[32]
Cold water immersion
Submerging the face in water cooler than about 21 °C (70 °F) triggers the diving reflex, common to air-breathing vertebrates, especially marine mammals such as whales and seals. This reflex protects the body by putting it into energy saving mode to maximize the time it can stay under water. The strength of this reflex is greater in colder water and has three principal effects:
- Bradycardia, a slowing of the heart rate by up to 50% in humans.
- Peripheral vasoconstriction, the restriction of the blood flow to the extremities to increase the blood and oxygen supply to the vital organs, especially the brain.
- Blood Shift, the shifting of blood to the thoracic cavity, the region of the chest between the diaphragm and the neck, to avoid the collapse of the lungs under higher pressure during deeper dives.
The reflex action is automatic and allows both a conscious and an unconscious person to survive longer without oxygen under water than in a comparable situation on dry land. The exact mechanism for this effect has been debated and may be a result of brain cooling similar to the protective effects seen in people who are treated with deep hypothermia.[33][34]
The actual cause of death in cold or very cold water is usually lethal bodily reactions to increased heat loss and to freezing water, rather than any loss of core body temperature. Of those who die after plunging into freezing seas, around 20% die within 2 minutes from cold shock (uncontrolled rapid breathing and gasping causing water inhalation, massive increase in blood pressure and cardiac strain leading to cardiac arrest, and panic), another 50% die within 15 – 30 minutes from cold incapacitation (loss of use and control of limbs and hands for swimming or gripping, as the body 'protectively' shuts down the peripheral muscles of the limbs to protect its core),[35] and exhaustion and unconsciousness cause drowning, claiming the rest within a similar time.[36] A notable example of this occurred during the sinking of the Titanic, in which most people who entered the −2 °C (28 °F) water died within 15–30 minutes.[37]
[S]omething that almost no one in the maritime industry understands. That includes mariners [and] even many (most) rescue professionals: It is impossible to die from hypothermia in cold water unless you are wearing flotation, because without flotation – you won’t live long enough to become hypothermic.
— Mario Vittone, lecturer and author in water rescue and survival[35]
Submersion into cold water can induce cardiac arrhythmias (abnormal heart rates) in healthy people, sometimes causing strong swimmers to drown.[38] The physiological effects caused by the diving reflex conflict with the body's cold shock response, which includes a gasp and uncontrollable hyperventilation leading to aspiration of water.[39] While breath-holding triggers a slower heart rate, cold shock activates tachycardia, an increase in heart rate.[38] It is thought that this conflict of these nervous system responses may account for the arrhythmias of cold water submersion.[38]
Heat transfers very well into water, and body heat is therefore lost extremely quickly in water compared to air,[40] even in merely 'cool' swimming waters around 70F (~20C).[36] A water temperature of 10 °C (50 °F) can lead to death in as little as one hour, and water temperatures hovering at freezing can lead to death in as little as 15 minutes.[36] This is because cold water can have other lethal effects on the body, so hypothermia is not usually a reason for drowning or the clinical cause of death for those who drown in cold water.
Upon submersion into cold water, remaining calm and preventing loss of body heat is paramount.[41] While awaiting rescue, swimming or treading water should be limited to conserve energy and the person should attempt to remove as much of the body from the water as possible; attaching oneself to a buoyant object can improve the chance of survival should unconsciousness occur.[41]
Hypothermia (and also cardiac arrest) present a risk for survivors of immersion, as for survivors of exposure; in particular the risk increases if the survivor, feeling well again, tries to get up and move, not realizing their core body temperature is still very low and will take a long time to recover.
Most people who experience cold-water drowning do not develop hypothermia quickly enough to decrease cerebral metabolism before ischemia and irreversible hypoxia occur. The neuroprotective effects appear to require water temperatures below about 5 °C.[42]
Diagnosis
The World Health Organization in 2005 defined drowning as "the process of experiencing respiratory impairment from submersion/immersion in liquid".[10] This definition does not imply death, or even the necessity for medical treatment after removal of the cause, nor that any fluid enters the lungs. The WHO further recommended that outcomes should be classified as: death, morbidity, and no morbidity.[10] There was also consensus that the terms wet, dry, active, passive, silent, and secondary drowning should no longer be used.[10]
Experts differentiate between distress and drowning.
- Distress – people in trouble, but who still have the ability to keep afloat, signal for help and take actions.
- Drowning – people suffocating and in imminent danger of death within seconds.
Forensics
Forensic diagnosis of drowning is considered one of the most difficult in forensic medicine. External examination and autopsy findings are often non-specific, and the available laboratory tests are often inconclusive or controversial. The purpose of investigation is generally to distinguish whether the death was due to immersion, or whether the body was immersed post mortem. The mechanism in acute drowning is hypoxemia and irreversible cerebral anoxia due to submersion in liquid.
Drowning would be considered as a possible cause of death when the body was recovered from a body of water, or in close proximity to a fluid which could plausibly have caused drowning, or when found with the head immersed in a fluid. A medical diagnosis of death by drowning is generally made after other possible causes of death have been excluded by means of a complete autopsy and toxicology tests. Indications of drowning are seldom completely unambiguous, and may include bloody froth in the airway, water in the stomach, cerebral oedema and petrous or mastoid haemorrhage. Some evidence of immersion may be unrelated to the cause of death, and lacerations and abrasions may have occurred before or after immersion or death.[23]
Diatoms should normally never be present in human tissue unless water was aspirated, and their presence in tissues such as bone marrow suggests drowning, however, they are present in soil and the atmosphere and samples may easily be contaminated. An absence of diatoms does not rule out drowning, as they are not always present in water.[23] A match of diatom shells to those found in the water may provide supporting evidence of the place of death. Drowning in salt water can leave significantly different concentrations of sodium and chloride ions in the left and right chambers of the heart, but this will dissipate if the person survived for some time after the aspiration, or if CPR was attempted,[23] and have been described in other causes of death.
Most autopsy findings relate to asphyxia and are not specific to drowning. The signs of drowning are degraded by decomposition. Large amounts of froth will be present around the mouth and nostrils and in the upper and lower airways in freshly drowned bodies. The volume of froth is generally much greater in drowning than from other origins. Lung density may be higher than normal but normal weights are possible after cardiac arrest reflex or vaso-vagal reflex. The lungs may be over inflated and waterlogged, filling the thoracic cavity, and the surface may have a marbled appearance, with darker areas associated with collapsed alveoli interspersed with paler aerated areas. Fluid trapped in the lower airways may block the passive collapse that is normal after death. Haemorrhagic bullae of emphysema may be found. These are related to rupture of alveolar walls. These signs, while suggestive of drowning, are not conclusive.
Prevention

It is estimated that more than 85% of drownings could be prevented by supervision, training in water skills, normatives, technology, and public education.[43][44]
- Surveillance of the swimmers: Watching the swimmers is a basic task, especially in the case of children. More than 500 children die from drowning each day. Young children must be supervised, regardless of if they can already swim. The danger increases when they are alone. A baby can drown in the bathtub, in the toilet, and even in a small bucket filled with less than an inch of water. It only takes around 2 minutes underwater for an adult to lose consciousness, and only between 30 seconds and 2 minutes for a small child to die. Choosing supervised swimming places is safer. Many pools and bathing areas either have lifeguards or a pool safety camera system for local or remote monitoring. Some others have a computer-aided drowning detection. However, normal bystanders can also play an important role in drowning detection, and in performing an intervention or notification to lifeguards or any other authority by any method (phone, alarm, etc.) Lifeguards may be unaware of a drowning due to "the intrusion of non-lifeguard duties upon lifeguards' primary task: preventive lifeguarding" and because of "the distraction from surveillance duties".[45] For example, they could be diverted by using the mobile phone for leisure purposes upon the watching operations. About the alarms in pools, evidence shows that they are poor for any utility.[46] The World Health Organization recommends to analyze what are the most crowded hours in the swimming zones, to increase the number of lifeguards at those moments (the more people is swimming, the more work is distributed to each lifeguard.)
- Learning to swim: Being able to swim is one of the best defenses against drowning. The studies recommend that children learn to swim when they are between 1 and 4 years old, but in a safe environment and being supervised. Learning to swim is also possible in adults, equally taking the classes in a safe environment and under supervision. After being able to swim, it's still possible to drown (because of the state of the water and other circumstances), so it is recommended to choose swimming places that are safe and kept under surveillance.
- Additional education: The WHO recommends to train the general public in first-aid for the drowned, cardiopulmonar resuscitation (CPR), and to behave in a safe manner when being in the water. In addition, it is convenient to give some advices to the minors so they avoid drowning. If they can not swim, it is recommended to teach them to keep themselves away from deep waters.
- Fencing the pools: Every swimming pool, private or public, should be fenced and enclosed, on every side, so no child nor any other person can access inside.[47] The "Raffarin law", applied in France in 2003, that forced to fence any pool, reduced the drowning of children by 75%. It is also convenient to check that there are no objects left on the surface of the pools, so children don't approach attracted by them.
.jpg.webp)
- Absorbed by pool drains: Swimming pools usually have drainage systems to absorb and beam the water. If they work badly, they can drain to the swimmers themselves, causing injuries or even trapping their hair or any extremity, which could lead to immobilize and drown them. To avoid it, drainage holes and sumps are covered with grates and lids (according to the case), and, besides, they must suction with not too much strength. This require to make a good installation of the pool, and to check it, and to review it periodically. It is also recommended that the pool has many drainage holes, small and spaced, instead of only a big one, but the most important factor is that the system work well.
- Caution in problematic diseases: Some illnesses require prudence when water is near. Epilepsy and all seizure disorders are problematic to swim, dive and bathe because of the possibility of drowning during a convulsion. Moreover, drowning is the most common cause of unintentional death for the people which suffers from that sort of diseases. For the epileptics, it is recommended to take showers rather than using a bath tub for bathing.
- Alcohol or drugs: Alcohol and drugs increase the probability of drowning. This danger is greater in the bars located near the water, in the parties of boat-clubs, etc.
.jpg.webp)
- Use of lifejacket: The children that can not swim, the disabled, and other people in risk of drowning, would have to wear a fastened lifejacket when they are in the water, and even near the water. There exist some other floating devices (inflatable inner tubes, arm floaties -water wings-, foam tubes, etc.) which can be more or less useful (depending of how is each one of them); however they are not considered safety instruments by the institutions, but "toys".[48] The instrument that is considered safe to float on water is the lifejacket, when it is homologated and well fastened around the body. Besides, there are some other flotation instruments that are considered safe: the professional circle-shaped lifebuoy (hoop-buoy, ring-buoy, life-ring, life-donut, lifesaver or lifepreserver), which is mainly designed to be thrown, and some other professional variants that are designed to be used by lifeguards in their rescues.
- Keeping calm in water: This is to avoid getting tired, because it difficults swimming. Exhaustion can appear because of the anxious movements motivated by fear during drowning. In other sense, a bad calculation of the own physical capabilities can leave oneself exhausted before reaching the water's edge. Lowering the rhythm helps to reduce exhaustion. In case of suffering a tug, cramp or contracture (muscle spasm), it is useful to keep calm and swimming towards the shore, asking for help if necessary. If oneself is stung by a jellyfish, it is possible to get out of the water without major problems even with some itching or pain. When a problem makes swimming more difficult, it is possible to float by laying on the own back (in a completely horizontal position face up), because that position allows to float without effort.
- Not to jump into water before knowing the depth: It is convenient to know if there are, or could be, rocks that stand out too much. Headfirst jumps cause more than 70% of all spinal injuries related to sports and recreational activities. A fall from a great height on shallow water (in a swimming pool or in the sea) can cause a serious impact against the bottom. This could kill the person immediately, or later, in case of suffering a brain or body injury followed by drowning. If the person does not die, the injury could cause a permanent paralysis.
- Avoid dangerous waters: Avoid swimming in turbulent waters, with very large waves, with dangerous animals, and in those that are too cold. Also avoid dragging currents. These currents may have any characteristic that allows to recognize them, such as being more turbulent, more foamy, dragging things or debris, etc. In case of being caught by one of these currents, swim out from it (it is possible to move out gradually, in a diagonal direction until arriving to the shore).
- Navigating safely: Many people who die by drowning die in navigation accidents. A safe navigation includes being informed of the state of the sea, and equipping the boat with regulatory instruments to keep people afloat. These instruments are lifejackets (see above) and professional lifebuoys with the shape of a circle (ring-buoy, hoop-buoy, life-ring, life-donut, lifesaver or lifepreserver).
- Use the "buddy system": It consists in not to swim alone, but near a buddy, who can help in case of any problem.
- Paying heed to rules: Most people who drown did not follow the safety normatives. It is important to pay attention to the banners, the flags that indicate if swimming is possible and the indications of the authorities (lifeguards, coastguards, etc.).
Water safety
The concept of water safety involves the procedures and policies that are directed to prevent people from drowning or injuring in water.[49]
Management
Rescue
.jpg.webp)
Many people who are drowning manage to save themselves, or are assisted by bystanders or professional rescuers. Less than 6% of people rescued by lifeguards need medical attention, and only 0.5% need CPR. The statistics are not as good for rescue by bystanders, but even there, a minority require CPR.
When a drowning occurs, or a swimmer becomes missing, bystanders should immediately call for help. A lifeguard should be called, if present. If not, emergency medical services and paramedics should be contacted as soon as possible. Rescue, and where necessary, resuscitation, should be started as early as possible. So the person should be taken out of the water as soon as possible.
Rescuers should avoid endangering themselves unnecessarily and, when possible, should assist from a safe position[50] (such as a boat or the shore). This assistance usually consists in throwing with precision a flotation instrument (as a hoop-shaped lifebuoy). In other cases, the manner to help could be by holding out an object (as a rope or pole, even the own arm. etc.) towards the person, but, doing this, the rescuer's body should be laying down, well secured to the ground, to avoid falling to the water too.
In a direct swimming rescue, the initial grasp is important and must be well managed by the rescuer. If something goes wrong, it could happen that an anxious drowning person clings to the rescuer to stand out of the water, submerging the rescuer in the process. To avoid this, it is recommended that the rescuer approaches to the panicking person with a buoyant object, or offering one hand, or even from behind and bending the person's arm against the back to restrict movement. Anyway, if the person pushes the rescuer towards below the water, the rescuer can usually escape diving downwards (because people who are unable to swim tend to move up, searching the water surface). After escaping in that manner, it is possible to come back and try a new approach to the drowning person. When the rescuer accomplishes a successful approach, the negatively buoyant objects (used in diving, such the weight belt) should be removed. Next, the priority is to transport the person to the water's edge using a tow maneuver. The rescuer usually approaches to the drowning person from behind, and then the person's body is turned face up, and grasped with a secure grip. There are many grips that can be used, but it is common that they grasp the person around the jaw area. The person's mouth and nose must be kept above the water surface. If the person is cooperative, the towing may be in a similar fashion held at the armpits. Unconscious people may be pulled in another similar fashion held at the chin and cheeks, and ensuring that the mouth and nose are well kept above the water. Special care has to be taken for people with suspected spinal injuries, they can require a more specific grip, and a back board (spinal board) may be needed for their rescue.[51]
In unconscious people, an in-water resuscitation could increase the chances of survival by a factor of about three, but this procedure require both medical and swimming skills, and only the breaths of the rescue ventilation are practicable in the water. Chest compressions require a suitable platform, so in-water assessment of circulation is pointless. If the person does not respond after a few breaths, cardiac arrest may be assumed, and getting them out of the water becomes the priority.[50]
First aid

The checks for responsiveness and breathing are carried out with the person horizontally supine. If unconscious but breathing, the recovery position is appropriate.
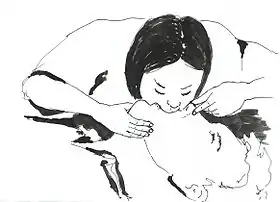
If not breathing, rescue ventilation is necessary. Drowning can produce a gasping pattern of apnea while the heart is still beating, and ventilation alone may be sufficient. The airway-breathing-circulation (ABC) sequence should be followed, rather than starting with compressions as is typical in cardiac arrest,[52] because the basic problem is lack of oxygen.
Five initial breaths are recommended, as the initial ventilation may be difficult because of water in the airways which can interfere with effective alveolar inflation. Thereafter a continual sequence of 2 breaths and 30 chest compressions is recommended. This alternance is repeated until vital signs are re-established, the rescuers are unable to continue, or advanced life support is available.[50] For babies, the procedure is slightly modified. In the rescue breaths, the rescuer's mouth covers the baby's mouth and nose at the same time. Besides, the chest compressions are applied pressing with only with two fingers on the chest bone (approximately on the lower part).
Attempts to actively expel water from the airway by abdominal thrusts, Heimlich maneuver or positioning head downwards should be avoided as there is no obstruction by solids, and they delay the start of ventilation and increase the risk of vomiting, with an increased risk of death, as aspiration of stomach contents is a common complication of resuscitation efforts.[50][53]
Treatment for hypothermia may also be necessary. Because of the diving reflex, people submerged in cold water and apparently drowned may revive after a relatively long period of immersion.[54] Rescuers retrieving a child from water significantly below body temperature should attempt resuscitation even after protracted immersion.[54]
Medical care
People with a near-drowning experience who have normal oxygen levels and no respiratory symptoms should be observed in a hospital for a period of time to ensure there are no delayed complications.[55] The target of ventilation is to achieve 92% to 96% arterial saturation and adequate chest rise. Positive end-expiratory pressure will generally improve oxygenation. Drug administration via peripheral veins is preferred over endotracheal administration. Hypotension remaining after oxygenation may be treated by rapid crystalloid infusion.[50] Cardiac arrest in drowning usually presents as asystole or pulseless electrical activity. Ventricular fibrillation is more likely to be associated with complications of pre-existing coronary artery disease, severe hypothermia, or the use of epinephrine or norepinephrine.[50]
While surfactant may be used, no high quality evidence exist that looks at this practice.[3] Extracorporeal membrane oxygenation may be used in those who cannot be oxygenated otherwise.[3] Steroids are not recommended.[3]
Prognosis
| Duration of submersion | Risk of death or poor outcomes[50] |
|---|---|
| 0–5 min | 10% |
| 6–10 min | 56% |
| 11–25 min | 88% |
| >25 min | nearly 100% |
| Signs of brain-stem injury predict death or severe neurological consequences | |

People who have drowned who arrive at a hospital with spontaneous circulation and breathing usually recover with good outcomes.[54] Early provision of basic and advanced life support improve probability of positive outcome.[50]
Longer duration of submersion is associated with lower probability of survival and higher probability of permanent neurological damage.[54]
Contaminants in the water can cause bronchospasm and impaired gas exchange, and can cause secondary infection with delayed severe respiratory compromise.[54]
Low water temperature can cause ventricular fibrillation, but hypothermia during immersion can also slow the metabolism, allowing a longer hypoxia before severe damage occurs.[54] Hypothermia which reduces brain temperature significantly can improve outcome. A reduction of brain temperature by 10 °C decreases ATP consumption by approximately 50%, which can double the time that the brain can survive.[50]
The younger the person, the better the chances of survival.[54] In one case, a child submerged in cold (37 °F (3 °C)) water for 66 minutes was resuscitated without apparent neurological damage.[54] However, over the long term significant deficits were noted, including a range of cognitive difficulties, particularly general memory impairment, although recent magnetic resonance imaging (MRI) and magnetoencephalography (MEG) were within normal range.[57]
Children
Drowning is a major worldwide cause of death and injury in children. Long term neurological outcomes of drowning cannot be predicted accurately during the early stages of treatment and although survival after long submersion times, mostly by young children, has been reported, many survivors will remain severely and permanently neurologically compromised after much shorter submersion times. Factors affecting probability of long term recovery with mild deficits or full function in young children include the duration of submersion, whether advanced life support was needed at the accident site, the duration of cardiopulmonary resuscitation, and whether spontaneous breathing and circulation are present on arrival at the emergency room.[58]
Data on long-term outcome are scarce and unreliable. Neurological examination at the time of discharge from hospital does not accurately predict long term outcomes. Some people with severe brain injury and were transferred to other institutions died months or years after the drowning and are recorded as survivors. Non-fatal drownings have been estimated as two to four times more frequent than fatal drownings.[58]
Epidemiology
In 2013, drowning was estimated to have resulted in 368,000 deaths, down from 545,000 deaths in 1990.[59] There are more than 20 times that many non-fatal incidents.[60] It is the third leading cause of death from unintentional trauma after traffic injuries and falls.[61]
In many countries, drowning is one of the main causes of preventable death for children under 12 years old. In the United States in 2006, 1100 people under 20 years of age died from drowning.[62] The United Kingdom has 450 drownings per year, or 1 per 150,000, whereas in the United States, there are about 6,500 drownings yearly, around 1 per 50,000. In Asia suffocation and drowning were the leading causes of preventable death for children under five years of age;[63][64] a 2008 report by the organization found that in Bangladesh, for instance, 46 children drown each day.[65]
Males, due to a generally increased likelihood for risk taking, are 4 times more likely to have submersion injuries.[60]
In the fishing industry, the largest group of drownings is associated with vessel disasters in bad weather, followed by man-overboard incidents and boarding accidents at night; either in foreign ports, or under the influence of alcohol.[60] Scuba diving deaths are estimated at 700 to 800 per year, associated with inadequate training and experience, exhaustion, panic, carelessness and barotrauma.[60]
United States
In the United States, drowning is the second leading cause of death (after motor vehicle accidents) in children 12 and younger.[66]
People who drown are more likely to be male, young, or adolescent.[66] Surveys indicate that 10% of children under 5 have experienced a situation with a high risk of drowning. Worldwide, about 175,000 children die through drowning every year.[67] The causes of drowning cases in the US from 1999 to 2006 were as follows:[68]
| 31.0% | Drowning and submersion while in natural water |
| 27.9% | Unspecified drowning and submersion |
| 14.5% | Drowning and submersion while in swimming pool |
| 9.4% | Drowning and submersion while in bathtub |
| 7.2% | Drowning and submersion following fall into natural water |
| 6.3% | Other specified drowning and submersion |
| 2.9% | Drowning and submersion following fall into swimming pool |
| 0.9% | Drowning and submersion following fall into bathtub |
According to the US National Safety Council, 353 people ages 5 to 24 drowned in 2017.[69]
Society and culture
Old terminology
The word "drowning"—like "electrocution"—was previously used to describe fatal events only, and occasionally that usage is still insisted upon, though the consensus of the medical community supports the definition used in this article. Several terms related to drowning which have been used in the past are also no longer recommended.[7] These include:
Active drowning: People, such as non-swimmers and the exhausted or hypothermic at the surface, who are unable to hold their mouth above water and are suffocating due to lack of air. Instinctively, people in such cases perform well-known behaviors in the last 20–60 seconds before being submerged, representing the body's last efforts to obtain air.[10][50] Notably, such people are unable to call for help, talk, reach for rescue equipment, or alert swimmers even feet away, and they may drown quickly and silently close to other swimmers or safety.[12]
- Passive drowning: People who suddenly sink or have sunk due to a change in their circumstances. Examples include people who drown in an accident, or due to sudden loss of consciousness or sudden medical condition.[50]
- Secondary drowning: Physiological response to foreign matter in the lungs due to drowning causing extrusion of liquid into the lungs (pulmonary edema) which adversely affects breathing.[10][50]
Dry drowning
Dry drowning is a term that has never had an accepted definition, and is currently medically discredited.[71][72] Following the 2002 World Congress on Drowning in Amsterdam, a consensus definition of drowning was established. Based on this definition, drowning is the "process of experiencing respiratory impairment from submersion/immersion in liquid."[73] This definition resulted in only three legitimate drowning subsets: fatal drowning, non-fatal drowning with illness/injury, and non-fatal drowning without illness/injury.[74] In response, major medical consensus organizations have adopted this definition worldwide and have officially discouraged any medical or publication use of the term "dry drowning".[71] Such organizations include the International Liaison Committee on Resuscitation,[75] the Wilderness Medical Society,[41] the American Heart Association,[76] the Utstein Style system,[75] the International Lifesaving Federation,[77] the International Conference on Drowning,[73] Starfish Aquatics Institute,[78] the American Red Cross,[79] the Centers for Disease Control and Prevention (CDC),[80][81][82] the World Health Organization [83] and the American College of Emergency Physicians.[84]
Drowning experts have recognized that the end result pathophysiology of hypoxemia, acidemia, and eventual death is the same whether water entered the lung or not. As this distinction does not change management or prognosis, but causes significant confusion due to alternate definitions and misunderstandings, it is generally established that pathophysiological discussions of "dry" versus "wet" drowning are not relevant to drowning care.[85]
"Dry drowning" is frequently cited in the news with a wide variety of definitions.[86] and is often confused with the equally inappropriate and discredited term "secondary drowning" or "delayed drowning".[87] Various conditions including spontaneous pneumothorax, chemical pneumonitis, bacterial or viral pneumonia, head injury, asthma, heart attack, and chest trauma have been misattributed to the erroneous terms "delayed drowning", "secondary drowning", and "dry drowning". Currently, there has never been a case identified in the medical literature where a person was observed to be without symptoms and who died hours or days later as a direct result of drowning alone.[71]
Capital punishment
In Europe, drowning was used as capital punishment. During the Middle Ages, a sentence of death was read using the words "cum fossa et furca", or "with pit and gallows".[88]
Drowning survived as a method of execution in Europe until the 17th and 18th centuries.[89] England had abolished the practice by 1623, Scotland by 1685, Switzerland in 1652, Austria in 1776, Iceland in 1777, and Russia by the beginning of the 1800s. France revived the practice during the French Revolution (1789–1799) and it was carried out by Jean-Baptiste Carrier at Nantes.[90]
References
- 1 2 "Drowning". CDC. 15 September 2017. Archived from the original on 3 February 2017. Retrieved 9 August 2018.
- 1 2 3 4 Ferri, Fred F. (2017). Ferri's Clinical Advisor 2018 E-Book: 5 Books in 1. Elsevier Health Sciences. p. 404. ISBN 9780323529570. Archived from the original on 30 July 2020. Retrieved 4 August 2020.
- 1 2 3 4 5 6 7 8 9 "Drowning - Injuries; Poisoning - Merck Manuals Professional Edition". Merck Manuals Professional Edition. September 2017. Archived from the original on 9 August 2018. Retrieved 9 August 2018.
- 1 2 3 4 5 Handley, AJ (16 April 2014). "Drowning". BMJ (Clinical Research Ed.). 348: g1734. doi:10.1136/bmj.g1734. PMID 24740929.
- 1 2 3 4 5 6 7 "Drowning". World Health Organization. 15 January 2018. Archived from the original on 23 August 2018. Retrieved 9 August 2018.
- 1 2 Preventing drowning: an implementation guide (PDF). WHO. 2015. p. 2. ISBN 978-92-4-151193-3. Archived (PDF) from the original on 28 July 2018. Retrieved 9 August 2018.
- 1 2 3 4 5 6 7 8 9 10 11 Mott, TF; Latimer, KM (1 April 2016). "Prevention and Treatment of Drowning". American Family Physician. 93 (7): 576–82. PMID 27035042.
- 1 2 GBD 2015 Disease and Injury Incidence and Prevalence, Collaborators. (8 October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- 1 2 3 4 GBD 2015 Mortality and Causes of Death, Collaborators. (8 October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- 1 2 3 4 5 6 7 8 9 10 11 van Beeck, EF; Branche, CM; Szpilman, D; Modell, JH; Bierens, JJ (November 2005). "A new definition of drowning: towards documentation and prevention of a global public health problem". Bulletin of the World Health Organization. 83 (11): 853–6. PMC 2626470. PMID 16302042.
- ↑ Wall, Ron (2017). Rosen's Emergency Medicine: Concepts and Clinical Practice (9 ed.). Elsevier. p. 1802. ISBN 978-0323354790.
- 1 2 3 4 Vittone, Mario; Pia, Francesco (Fall 2006). "'It Doesn't Look Like They're Drowning': How To Recognize the Instinctive Drowning Response" (PDF). On Scene: The Journal of U.S. Coast Guard Search and Rescue: 14. Archived (PDF) from the original on 3 January 2011. Retrieved 29 December 2010.
- 1 2 Pia, Frank (1999). "Chapter 14: Reflections on Lifeguard surveillance programs". In Fletemeyer, John R.; Freas, Samuel J. (eds.). Drowning: New Perspectives on Intervention and Prevention. p. 234. ISBN 978-1-57444-223-6.
- ↑ O'Connell, Claire (3 August 2010). "What stops people shouting and waving when drowning?". Irish Times. Archived from the original on 22 October 2012. Retrieved 29 December 2010.
- ↑ Young, David (13 July 2012). "Rivers - The impact of European settlement". Te Ara: The Encyclopedia of New Zealand. Archived from the original on 2 June 2015. Retrieved 7 January 2015.
- ↑ Gulli, Benjamin; Ciatolla, Joseph A.; Barnes, Leaugeay (2011). Emergency Care and Transportation of the Sick and Injured. Sudbury, Massachusetts: Jones and Bartlett. p. 1157. ISBN 9780763778286. Archived from the original on 25 November 2017.
- 1 2 Staff (23 September 2014). "Drowning". CDC Tip sheets. Atlanta. Georgia: Centers for Disease Control and Prevention. Archived from the original on 3 February 2017. Retrieved 2 February 2017.
- ↑ Staff (28 April 2016). "Unintentional Drowning: Get the Facts". Home and Recreational Safety. Atlanta, Georgia: Centers for Disease Control and Prevention. Archived from the original on 2 February 2017. Retrieved 2 February 2017.
- ↑ Watila, Musa M.; Balarabe, Salisu A.; Ojo, Olubamiwo; Keezer, Mark R.; Sander, Josemir W. (October 2018). "Overall and cause-specific premature mortality in epilepsy: A systematic review" (PDF). Epilepsy & Behavior. 87: 213–225. doi:10.1016/j.yebeh.2018.07.017. ISSN 1525-5050. PMID 30154056.
- ↑ Hamilton, Kyra; Keech, Jacob J.; Peden, Amy E.; Hagger, Martin S. (2018-06-03). "Alcohol use, aquatic injury, and unintentional drowning: A systematic literature review". Drug and Alcohol Review. 37 (6): 752–773. doi:10.1111/dar.12817. ISSN 0959-5236. PMID 29862582. Archived from the original on 14 March 2021. Retrieved 4 August 2020.
- ↑ Campbell, Ernest (1996). "Free Diving and Shallow Water Blackout". Diving Medicine Online. scuba-doc.com. Archived from the original on 18 September 2016. Retrieved 24 January 2017.
- 1 2 Lindholm, P; Lundgren, C. E. (2006). "Alveolar gas composition before and after maximal breath-holds in competitive divers". Undersea & Hyperbaric Medicine. 33 (6): 463–7. PMID 17274316. Archived from the original on 24 March 2011. Retrieved 30 December 2010.
- 1 2 3 4 Harle, Lindsey (August 2012). "Drowning". Forensic pathology: Types of injuries. PathologyOutlines.com. Archived from the original on 7 February 2017. Retrieved 3 February 2017.
- 1 2 Gorman, Mark (2008). Jose Biller (ed.). Interface of Neurology and Internal Medicine. Lippincott Williams & Wilkins. pp. 702–706. ISBN 978-0-7817-7906-7. Archived from the original on 19 June 2013. Retrieved 9 May 2013.
- ↑ Lane, Jordan D. (2017). "Drowning Deaths From Unsupervised Breath Holding: Separating Necessary Training From Unwarranted Risk". Military Medicine. 182 (January/February): 1471–1473. doi:10.7205/MILMED-D-16-00246. PMID 28051962.
- 1 2 Lindholm, Peter (2006). Lindholm, P.; Pollock, N. W.; Lundgren, C. E. G. (eds.). Physiological mechanisms involved in the risk of loss of consciousness during breath-hold diving (PDF). Breath-hold diving. Proceedings of the Undersea and Hyperbaric Medical Society/Divers Alert Network 2006 June 20–21 Workshop. Durham, NC: Divers Alert Network. p. 26. ISBN 978-1-930536-36-4. Archived (PDF) from the original on 19 May 2016. Retrieved 24 January 2017.
- ↑ North, Robert (December 2002). "The pathophysiology of drowning" (PDF). South Pacific Underwater Medicine Society Journal. 32 (4). Archived from the original (PDF) on 11 February 2017. Retrieved 9 February 2017.
- 1 2 Cantwell, G Patricia (5 July 2016). "Drowning: Pathophysiology". Drugs & Diseases - Emergency Medicine. Medscape. Archived from the original on 4 February 2017. Retrieved 3 February 2017.
- ↑ DiMaio, Dominick; DiMaio, Vincent J.M. (28 June 2001). Forensic Pathology (2nd ed.). Taylor & Francis. pp. 405–. ISBN 978-0-8493-0072-1. Archived from the original on 19 June 2013. Retrieved 9 May 2013.
- 1 2 3 4 Jin, Faguang; Li, Congcong (2017-04-05). "Seawater-drowning-induced acute lung injury: From molecular mechanisms to potential treatments". Experimental and Therapeutic Medicine. 13 (6): 2591–2598. doi:10.3892/etm.2017.4302. ISSN 1792-0981. PMC 5450642. PMID 28587319.
- 1 2 Bierens JJ, Lunetta P, Tipton M, Warner DS. Physiology Of Drowning: A Review. Physiology (Bethesda). 2016 Mar;31(2):147-66.
- 1 2 Michelet, Pierre; Dusart, Marion; Boiron, Laurence; Marmin, Julien; Mokni, Tarak; Loundou, Anderson; Coulange, Mathieu; Markarian, Thibaut (2018-08-03). "Drowning in fresh or salt water". European Journal of Emergency Medicine. Publish Ahead of Print (5): 340–344. doi:10.1097/mej.0000000000000564. ISSN 0969-9546. PMID 30080702.
- ↑ Lundgren, Claus E. G.; Ferrigno, Massimo, eds. (1985). Physiology of Breath-hold Diving. 31st Undersea and Hyperbaric Medical Society Workshop. Vol. UHMS Publication Number 72(WS-BH)4-15-87. Undersea and Hyperbaric Medical Society. Archived from the original on 2 June 2009. Retrieved 24 April 2009.
- ↑ Mackensen, G. B.; McDonagh, D. L.; Warner, D. S. (March 2009). "Perioperative hypothermia: use and therapeutic implications". J. Neurotrauma. 26 (3): 342–58. doi:10.1089/neu.2008.0596. PMID 19231924.
- 1 2 Vittone, Mario (21 October 2010). "The Truth About Cold Water". Survival. Mario Vittone. Archived from the original on 14 January 2017. Retrieved 24 January 2017.
- 1 2 3 "Hypothermia safety". United States Power Squadrons. 23 January 2007. Archived from the original on 8 December 2008. Retrieved 19 February 2008.
- ↑ Butler, Daniel Allen (1998). Unsinkable: The Full Story of RMS Titanic. Mechanicsburg, PA: Stackpole Books. ISBN 978-0-8117-1814-1.
- 1 2 3 Shattock, Michael J.; Tipton, Michael J. (2012-06-14). "'Autonomic conflict': a different way to die during cold water immersion?". The Journal of Physiology. 590 (14): 3219–3230. doi:10.1113/jphysiol.2012.229864. ISSN 0022-3751. PMC 3459038. PMID 22547634.
- ↑ Tipton, M. J.; Collier, N.; Massey, H.; Corbett, J.; Harper, M. (2017-09-21). "Cold water immersion: kill or cure?". Experimental Physiology. 102 (11): 1335–1355. doi:10.1113/ep086283. ISSN 0958-0670. PMID 28833689. Archived from the original on 30 July 2020. Retrieved 4 August 2020.
- ↑ Sterba, J. A. (1990). "Field Management of Accidental Hypothermia during Diving". US Navy Experimental Diving Unit Technical Report. NEDU-1-90. Archived from the original on 27 July 2011. Retrieved 11 June 2008.
- 1 2 3 Schmidt, AC; Sempsrott JR; Hawkins SC (2016). "Wilderness Medical Society Practice Guidelines for the Prevention and Treatment of Drowning". Wilderness & Environmental Medicine. 27 (2): 236–51. doi:10.1016/j.wem.2015.12.019. PMID 27061040. Retrieved August 25, 2017.
- ↑ Cantwell, G Patricia (5 July 2016). "Drowning: Prognosis". Drugs & Diseases - Emergency Medicine. Medscape. Archived from the original on 4 February 2017. Retrieved 3 February 2017.
- ↑ Centers for Disease Control and Prevention. "Water-Related Injuries". Archived from the original on 14 February 2020.
- ↑ Szpilman, David; Bierens, Joost J.L.M.; Handley, Anthony J.; Orlowski, James P. (4 October 2012). "Drowning". The New England Journal of Medicine. 366 (22): 2102–2110. doi:10.1056/NEJMra1013317. PMID 22646632.
- ↑ Pia, Frank (June 1984). "The RID factor as a cause of drowning". Parks & Recreation. Archived from the original on 5 March 2016. Retrieved 1 October 2012 – via pia-enterprises.com.
- ↑ Mott, TF; Latimer, KM (1 April 2016). "Prevention and Treatment of Drowning". American Family Physician. 93 (7): 576–82. PMID 27035042.
- ↑ Thompson, D. C.; Rivara, F. P. (2000). "Pool fencing for preventing drowning in children". The Cochrane Database of Systematic Reviews (2): CD001047. doi:10.1002/14651858.CD001047. ISSN 1469-493X. PMID 10796742.
- ↑ Centers for Disease Control and Prevention. "Water-Related Injuries". Archived from the original on 14 February 2020.
- ↑ "Water safety - RoSPA". rospa.com. Archived from the original on 21 December 2019. Retrieved 2020-02-14.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Szpilman, David; Bierens, Joost J.L.M.; Handley, Anthony J.; Orlowski, James P. (4 October 2012). "Drowning". The New England Journal of Medicine. 366 (22): 2102–2110. doi:10.1056/NEJMra1013317. PMID 22646632.
- ↑ "2005 ILCOR resuscitation guidelines" (PDF). Circulation. 112 (22 supplement). 29 November 2005. doi:10.1161/CIRCULATIONAHA.105.166480 (inactive 25 January 2020). Archived (PDF) from the original on 27 February 2008. Retrieved 17 February 2008.
There is insufficient evidence to recommend for or against the use of oxygen by the first aid provider.
{{cite journal}}: CS1 maint: DOI inactive as of January 2020 (link) - ↑ Hazinski, Mary Fran, ed. (2010). Guidelines for CPR and ECC (PDF). Highlights of the 2010 American Heart Association (Report). American Heart Association. p. 2. Archived (PDF) from the original on 6 January 2017. Retrieved 2 January 2017.
- ↑ MedlinePlus Encyclopedia: Near drowning
- 1 2 3 4 5 6 7 8 McKenna, Kim D. (2011). Mosby's paramedic textbook. Jones & Bartlett Publishers. pp. 1262–1266. ISBN 978-0-323-07275-5. Archived from the original on 19 June 2013. Retrieved 9 May 2013.
- ↑ "Drowning - Symptoms, diagnosis and treatment". BMJ Best Practice. Archived from the original on 3 December 2018. Retrieved 2018-12-03.
- ↑ "WHO Disease and injury country estimates". World Health Organization. 2009. Archived from the original on 11 November 2009. Retrieved 11 November 2009.
- ↑ Hughes, S. K.; Nilsson, D. E.; Boyer, R. S.; Bolte, R. G.; Hoffman, R. O.; Lewine, J. D.; Bigler, E. D. (2002). "Neurodevelopmental outcome for extended cold water drowning: A longitudinal case study". Journal of the International Neuropsychological Society. 8 (4): 588–596. doi:10.1017/s1355617702814370. PMID 12030312.
- 1 2 Suominen, Pertti K.; Vähätalo, Raisa (15 August 2012). "Neurologic long term outcome after drowning in children". Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine. 20 (55): 55. doi:10.1186/1757-7241-20-55. ISSN 1757-7241. PMC 3493332. PMID 22894549.
- ↑ GBD 2013 Mortality and Causes of Death, Collaborators (17 December 2014). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- 1 2 3 4 Cantwell, G Patricia (5 July 2016). "Drowning: Epidemiology". Drugs & Diseases - Emergency Medicine. Medscape. Archived from the original on 4 February 2017. Retrieved 3 February 2017.
- ↑ Lozano, R; Naghavi, M.; Foreman, K.; Lim, S.; Shibuya, K.; Aboyans, V.; Abraham, J.; Adair, T.; Aggarwal, R.; Ahn, S. Y.; Alvarado, M.; Anderson, H. R.; Anderson, L. M.; Andrews, K. G.; Atkinson, C.; Baddour, L. M.; Barker-Collo, S.; Bartels, D. H.; Bell, M. L.; Benjamin, E. J.; Bennett, D.; Bhalla, K.; Bikbov, B.; Bin Abdulhak, A.; Birbeck, G.; Blyth, F.; Bolliger, I.; Boufous, S.; Bucello, C.; et al. (15 Dec 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–128. doi:10.1016/S0140-6736(12)61728-0. hdl:10536/DRO/DU:30050819. PMID 23245604.
- ↑ Committee on injury, violence, and poison prevention (2010). "Policy Statement—Prevention of Drowning". Pediatrics. 126 (1): 178–185. doi:10.1542/peds.2010-1264. PMID 20498166. Archived from the original on 9 June 2010.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ "Drowning, Homicide and Suicide Leading Killers for Children in Asia". The Salem News. 11 March 2008. Archived from the original on 11 September 2011. Retrieved 5 October 2010.
- ↑ "UNICEF Says Injuries A Fatal Problem For Asian Children". All Headline News. 13 March 2008. Archived from the original on 18 January 2012. Retrieved 5 October 2010.
- ↑ "Children Drowning, Drowning Children" (PDF). The Alliance for Safe Children. Archived from the original (PDF) on 28 July 2011. Retrieved 6 October 2010.
- 1 2 "Drowning". Centers for Disease Control and Prevention. 23 September 2014. Archived from the original on 10 May 2016. Retrieved 26 June 2016.
- ↑ "Traffic Accidents Top Cause Of Fatal Child Injuries". Science. National Public Radio. 10 December 2008. Archived from the original on 12 December 2016. Retrieved 2 February 2017.
- ↑ "Archived copy". Archived from the original on 27 September 2017. Retrieved 9 September 2017.
{{cite web}}: CS1 maint: archived copy as title (link) - ↑ "Drowning: It Can Happen in an Instant". US National Safety Council. 2019. Archived from the original on 14 June 2019. Retrieved 2019-05-31.
- ↑ Breining, Greg (29 May 2015). "Silent Drowning: How to Spot the Signs and Save a Life". Outdoors. Safe Bee. Archived from the original on 3 February 2017. Retrieved 2 February 2017.
- 1 2 3 Hawkins, SC; Sempsrott, J.; Schmidt, A. (16 June 2017). "Drowning in a Sea of Misinformation: Dry Drowning and Secondary Drowning". Emergency Medicine News. Archived from the original on 7 August 2017.
- ↑ Szpilman, D; Bierens JL; Handley A; Orlowski JP (2012). "Drowning". New England Journal of Medicine. 10 (2): 2102–2110. doi:10.1056/nejmra1013317. PMID 22646632.
- 1 2 van Beeck, EF (2006). "Definition of Drowning". In Handbook on Drowning: Prevention, Rescue, Treatment. Berlin: Springer.
- ↑ Van Beeck, EF; Branche, CM (2005). "A new definition of drowning: towards documentation and prevention of a global public health program". Bull World Health Organ. 83: 853–856.
- 1 2 Idris, AH (2003). "Recommended Guidelines for Uniform Reporting of Data from Drowning". Circulation. 108 (20): 2565–2574. doi:10.1161/01.cir.0000099581.70012.68. PMID 14623794.
- ↑ "2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 112 (24): IV–133–IV–135. 2005. doi:10.1161/CIRCULATIONAHA.105.166565. Archived from the original on 26 August 2017. Retrieved 25 August 2017.
- ↑ "Lifesaving Position Statement LPS 17: Definition of Drowning". International Life Saving Federation. 9 March 2016. Archived from the original on 1 July 2017. Retrieved 25 August 2017.
- ↑ "Defining Drowning". www.starfishaquaticsinstitute.blogspot.com. Starfish Aquatics Institute. 7 April 2015. Archived from the original on 25 August 2017. Retrieved 25 August 2017.
- ↑ Tobin, JM; Rossano JW; Wernicki PG (2017). "Dry Drowning: A Distinction without a Difference". Resuscitation. 118: e5–e6. doi:10.1016/j.resuscitation.2017.06.023. PMID 28655623. Retrieved August 25, 2017.
- ↑ Gilchrist, A (2004). "Nonfatal and Fatal Drownings in Recreational Water Settings-United States 2001-2002". Morbidity and Mortality Weekly Report. 53: 447–452.
- ↑ "Dry Drowning". Snopes. June 8, 2017. Retrieved August 25, 2017.
- ↑ "Water-Related Injuries". US Centers for Disease Control and Prevention. Jun 12, 2008. Archived from the original on July 19, 2008. Retrieved August 25, 2017.
{{cite web}}: CS1 maint: bot: original URL status unknown (link) - ↑ van Beek, EF (2005). "A new definition of drowning: towards documentation and prevention of a global public health problem". Bulletin of the World Health Organization. 83: 801–880.
- ↑ American College of Emergency Physicians Press Release (11 July 2017). "Death After Swimming Is Extremely Rare and is NOT Dry Drowning". www.acep.org. American College of Emergency Physicians. Archived from the original on 7 August 2017. Retrieved 25 August 2017.
- ↑ Sempsrott, J; Schmidt, AC; Hawkins, SC (2017). "Drowning and Submersion Injuries". In Auerbach's Wilderness Medicine 7th edition. Philadelphia: Elsevier.
- ↑ "Death After Swimming is Extremely Rare – And is NOT "Dry Drowning"". American College of Emergency Physicians. Archived from the original on 21 October 2017. Retrieved 20 October 2017.
- ↑ Sempsrott, J. "Wet and Wild: Drowning & Water Injuries: Dry Drowning and Secondary Drowning". Wilderness Medicine Magazine. Archived from the original on 7 August 2017.
- ↑ Halkerston, Peter (1829). A Translation and Explanation of the principal technical Terms and Phrases used in Mr. Erskine's Institute of the Law of Scotland ... With an index materiarum and the Latin maxims in law and equity most in use (2nd ed.). Edinborough: Peter Halkerston. p. 29. Archived from the original on 25 November 2017. Retrieved 2 February 2017.
- ↑ Norton, Rictor (17 November 2011). "Newspaper Reports: The Dutch Purge of Homosexuals, 1730". Homosexuality in Eighteenth-Century England: A Sourcebook. Archived from the original on 18 May 2012.
- ↑ . Encyclopædia Britannica. Vol. 08 (11th ed.). 1911.
External links
- Canadian Red Cross: Drowning Research: Drownings in Canada, 10 Years of Research Module 2 – Ice & Cold Water Immersion
| Classification | |
|---|---|
| External resources |
