Pancreatic cyst
| Pancreatic cyst | |
|---|---|
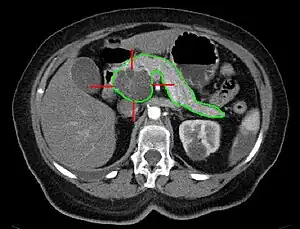 | |
| MRI - cancerous pancreatic cyst | |
| Specialty | Gastroenterology |
A pancreatic cyst is a fluid filled sac within the pancreas.[1] There are several types, some with the potential to become cancerous, and they are commonly found when investigating another problem.[2]
Diagnosis is by medical imaging.[2]
Up to one in five MRIs and 3% of CTs in older people may show a pancreatic cyst.[2] The most common pancreatic cysts are the serous cystadenoma, mucinous cystic neoplasm (MCN), and intraductal papillary mucinous neoplasm (IPMN).[2]
Types
Cystic lesions are found in 20.6% of all pancreatectomy specimens. Among this heterogeneous group, benign neoplasms predominate, particularly those with mucinous lining. Age at presentation, gender, location and tumor size are highly variable, with the exception of solid pseudopapillary tumor.
- Pancreatic intraductal papillary mucinous tumors (most common diagnosis - 52.6%)
- Pancreatic serous cystic tumors (20.6%)
- Pancreatic serous cystadenoma
- Pancreatic serous cystadenocarcinoma
- Pancreatic mucinous cystic tumors (13.4%)
- Pancreatic mucinous cystadenoma
- Pancreatic mucinous cystadenocarcinoma
Cause
Causes range from benign to malignant. Pancreatic cysts can occur in the setting of pancreatitis, though they are only reliably diagnosed 6 weeks after the episode of acute pancreatitis.
Benign tumors such as serous cystadenomas can occur. Main branch intraductal papillary mucinous neoplasms (IPMNs) are associated with dilatation of the main pancreatic duct, while side branch IPMNs are typically benign, and not associated with dilatation. MRCP can help distinguish the position of the cysts relative to the pancreatic duct, and direct appropriate treatment and follow-up. The most common malignancy that can present as a pancreatic cyst is a mucinous cystic neoplasm.
Follow up guidelines
Cysts from 1–5 mm on CT or ultrasound are typically too small to characterize and considered benign. No further imaging follow-up is recommended for these lesions. Cysts from 6–9 mm require a single follow-up in 2–3 years, preferably with magnetic resonance cholangiopancreatography (MRCP) to better evaluate the pancreatic duct. If stable at follow-up, no further imaging follow-up is recommended. For cysts from 1–1.9 cm follow-up is suggested with MRCP or multiphasic CT in 1–2 years. If stable at follow-up, the interval of imaging follow-up is increased to 2–3 years. Cysts from 2–2.9 cm have more malignant potential, and a baseline endoscopic ultrasound is suggested, followed by MRCP or multiphasic CT in 6–12 months. If patients are young, surgery may be considered to avoid the need for prolonged surveillance. If these cysts are stable at follow-up, interval imaging follow-up can be done in 1–2 years.[3]
References
- ↑ Shipley, LC; Ahmed, AM (2022). "New and emerging technology in the diagnosis and treatment of pancreatic cysts". Translational gastroenterology and hepatology. 7: 15. doi:10.21037/tgh-2020-09. PMID 35548473. Archived from the original on 2022-07-05. Retrieved 2022-07-02.
- 1 2 3 4 Lee, LS (14 September 2021). "Updates in diagnosis and management of pancreatic cysts". World journal of gastroenterology. 27 (34): 5700–5714. doi:10.3748/wjg.v27.i34.5700. PMID 34629795. Archived from the original on 5 July 2022. Retrieved 2 July 2022.
- ↑ Campbell, NM; Katz, SS; Escalon, JG; Do, RK (March 2015). "Imaging patterns of intraductal papillary mucinous neoplasms of the pancreas: an illustrated discussion of the International Consensus Guidelines for the Management of IPMN". Abdominal Imaging. 40 (3): 663–77. doi:10.1007/s00261-014-0236-4. PMID 25219664.
External links
| Classification |
|---|