Posterior vitreous detachment
| Posterior vitreous detachment | |
|---|---|
| Other names: Vitreous detachment | |
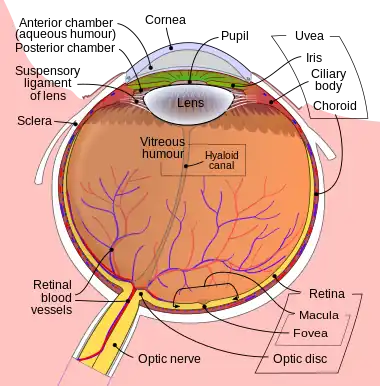 | |
| Schematic diagram of the human eye. | |
| Specialty | Opthalmology |
| Symptoms | Floaters, flashes of light[1] |
| Complications | Retinal tear, retinal detachment, macular hole, macular pucker[1] |
| Usual onset | >50 yr old[1] |
| Risk factors | Nearsightedness[1] |
| Diagnostic method | Dilated eye exam[1] |
| Differential diagnosis | Migraine aura, uveitis, retinitis pigmentosa[2] |
| Treatment | None, surgery[1] |
| Prognosis | Usually good[2] |
| Frequency | Common[1] |
Posterior vitreous detachment (PVD) is a condition of the eye in which the vitreous separates from the retina.[3][4] Symptoms include floaters and flashes of light in the peripheral vision.[1] Pain does not occur.[3] This generally resolves over a few months.[1] Complications may include retinal tear, retinal detachment, macular hole, macular pucker, and vitreous bleed.[1][2]
Risk factors include being nearsighted.[1] Episodes may be triggered by cataract surgery, trauma, uveitis, and laser capsulotomy.[2] The underlying mechanism involves age related softening of the vitreous.[3] Diagnosis is by dilated eye exam.[1] Other measures used may include ultrasound and optical coherence tomography.[2]
In most cases no specific treatment is required.[1] Follow up may be recommended in 2 to 4 weeks to rule out complications.[2] Outcomes are usually good.[2] If the condition causes significant problems surgery, known as a vitrectomy, may be tried.[1]
Posterior vitreous detachment becomes common as people age.[1] About half of people over the age of 50 are affected.[2] Women are more commonly affected at a younger age.[2] It was first described in 1856 by Muller and 1875 by Briere.[2]
Signs and symptoms
When this occurs there is a characteristic pattern of symptoms:
- Flashes of light (photopsia)
- A sudden increase in the number of floaters
- A ring of floaters or hairs just to the temporal side of the central vision
As a posterior vitreous detachment proceeds, adherent vitreous membrane may pull on the retina. While there are no pain fibers in the retina, vitreous traction may stimulate the retina, with resultant flashes that can look like a perfect circle.
If a retinal vessel is torn, the leakage of blood into the vitreous cavity is often perceived as a "shower" of floaters. Retinal vessels may tear in association with a retinal tear, or occasionally without the retina being torn.
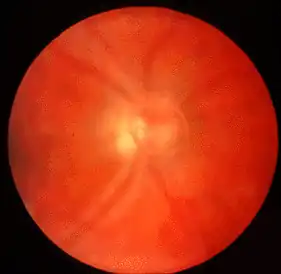
A Weiss ring can sometimes be seen with ophthalmoscopy as very strong indicator that vitreous detachment has occurred. This ring can remain free-floating for years after detachment.
Complications
The risk of retinal detachment is the greatest in the first 6 weeks following a vitreous detachment, but can occur over 3 months after the event.
The risk of retinal tears and detachment associated with vitreous detachment is higher in patients with myopic retinal degeneration, lattice degeneration, and a familial or personal history of previous retinal tears/detachment.
Causes
The vitreous (Latin for "glassy") humor is a gel which fills the eye behind the lens. Between it and the retina is the vitreous membrane. With age the vitreous humor changes, shrinking and developing pockets of liquefaction, similar to the way a gelatin dessert shrinks and detaches from the edge of a pan. At some stage the vitreous membrane may peel away from the retina. This is usually a sudden event, but it may also occur slowly over months.
Age and refractive error play a role in determining the onset of PVD in a healthy person. PVD is rare in emmetropic people under the age of 40 years, and increases with age to 86% in the 90s. Several studies have found a broad range of incidence of PVD, from 20% of autopsy cases to 57% in a more elderly population of patients (average age was 83.4 years).[5]
People with myopia (nearsightedness) greater than 6 diopters are at higher risk of PVD at all ages. Posterior vitreous detachment does not directly threaten vision. Even so, it is of increasing interest because the interaction between the vitreous body and the retina might play a decisive role in the development of major pathologic vitreoretinal conditions, such as epiretinal membrane.
PVD may also occur in cases of cataract surgery, within weeks or months of the surgery.[6]
The vitreous membrane is more firmly attached to the retina anteriorly, at a structure called the vitreous base. The membrane does not normally detach from the vitreous base, although it can be detached with extreme trauma. However, the vitreous base may have an irregular posterior edge. When the edge is irregular, the forces of the vitreous membrane peeling off the retina can become concentrated at small posterior extensions of the vitreous base. Similarly, in some people with retinal lesions such as lattice retinal degeneration or chorio-retinal scars, the vitreous membrane may be abnormally adherent to the retina. If enough traction occurs the retina may tear at these points. If there are only small point tears, these can allow glial cells to enter the vitreous humor and proliferate to create a thin epiretinal membrane that distorts vision. In more severe cases, vitreous fluid may seep under the tear, separating the retina from the back of the eye, creating a retinal detachment. Trauma can be any form from a blunt force trauma to the face such as a boxer's punch or even in some cases has been known to be from extremely vigorous coughing or blowing of the nose.
Diagnosis
Posterior Vitreous Detachment is diagnosed via dilated eye examination. For some patients the vitreous gel is extremely clear and so it can be hard to see the PVD. In these cases, additional imaging such as Optical Coherence Tomography (OCT) or ocular ultrasound are used.[7]
Treatment
Therapy is not required or indicated in posterior vitreous detachment, unless there are associated retinal tears, which need to be repaired.[8] In absence of retinal tears, the usual progress is that the vitreous humor will continue to age and liquefy and floaters will usually become less and less noticeable, and eventually most symptoms will completely disappear.[8] Prompt examination of patients experiencing vitreous humor floaters combined with expeditious treatment of any retinal tears has been suggested as the most effective means of preventing certain types of retinal detachments.[9]
See also
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 "Vitreous Detachment | National Eye Institute". www.nei.nih.gov. Archived from the original on 10 February 2022. Retrieved 11 February 2022.
- 1 2 3 4 5 6 7 8 9 10 Ahmed, Faryal; Tripathy, Koushik (2022). "Posterior Vitreous Detachment". StatPearls. StatPearls Publishing. Archived from the original on 22 January 2022. Retrieved 11 February 2022.
- 1 2 3 Gauger E; Chin EK; Sohn EH (17 November 2014). "Vitreous Syneresis: An Impending Posterior Vitreous Detachment (PVD)". University of Iowa Health Care: Ophthalmology and Visual Sciences. Archived from the original on 5 July 2020. Retrieved 7 June 2021; See "Discussion" following "Clinical Course".
{{cite web}}: CS1 maint: postscript (link) - ↑ "Posterior vitreous detachment". RNIB - See differently. 19 February 2014. Archived from the original on 29 June 2021. Retrieved 11 February 2022.
- ↑ Acta Ophthalmol. 2012 May;90(3):e179-84. doi: 10.1111/j.1755-3768.2011.02310.x. Epub 2011 Nov 22.Prevalence of early and late stages of physiologic PVD in emmetropic elderly population. Schwab C, Ivastinovic D, Borkenstein A, Lackner EM, Wedrich A, Velikay-Parel M.
- ↑ Hilford D; Hilford M; Mathew A; Polkinghorne PJ (2009). "Posterior vitreous detachment following cataract surgery". Eye. 23 (6): 1388–1392. doi:10.1038/eye.2008.273. PMID 18776863.
- ↑ Thompson, John. "Posterior Vitreous Detachment". American Society of Retinal Specialists. ASRS. Archived from the original on July 21, 2017. Retrieved July 11, 2017.
- 1 2 "Posterior Vitreous Detachment". Cleveland Clinic. Archived from the original on 2009-12-13. Retrieved 2008-12-24.
- ↑ Byer, NE (September 1994). "Natural history of posterior vitreous detachment with early management as the premier line of defense against retinal detachment". Ophthalmology. 101 (9): 1503–13, discussion 1513–4. doi:10.1016/s0161-6420(94)31141-9. PMID 8090453.
External links
| Classification |
|---|