Scott syndrome
| Scott syndrome | |
|---|---|
| Other names | Platelet factor X receptor deficiency |
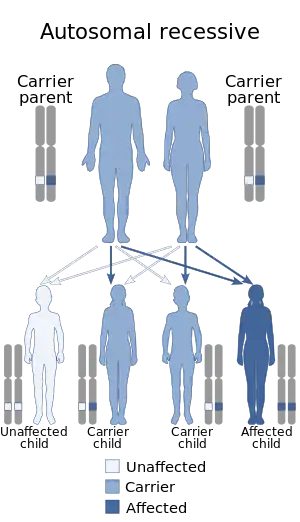 | |
| This condition is inherited in an autosomal recessive manner | |
Scott syndrome is a rare congenital bleeding disorder that is due to a defect in a platelet mechanism required for blood coagulation.[1]
Normally when a vascular injury occurs, platelets are activated and phosphatidylserine (PS) in the inner leaflet of the platelet membrane is transported to the outer leaflet of the platelet membrane, where it provides a binding site for plasma protein complexes that are involved in the conversion of prothrombin to thrombin, such as factor VIIIa-IXa (tenase) and factor Va-Xa (prothrombinase).[2]
In Scott syndrome, the mechanism for translocating PS to the platelet membrane is defective, resulting in impaired thrombin formation.[3][4][5] A similar defect in PS translocation has also been demonstrated in Scott syndrome red blood cells and Epstein-Barr virus transformed lymphocytes, suggesting that the defect in Scott syndrome reflects a mutation in a stem cell that affects multiple hematological lineages.
The basis for the defect in PS translocation is, at present, unknown. A candidate protein, scramblase,[6] that may be involved in this process appears to be normal in Scott syndrome platelets.[7] Other possible defects in PS translocation, reported in some patients, require further study.[8] The initially reported patient with Scott Syndrome has been found to have a mutation at a splice-acceptor site of the gene encoding anoctamin 6 (ANO6, transmembrane protein 16F, TMEM16F).[9] At present, the only treatment for episodes of bleeding is the transfusion of normal platelets.
References
- ↑ Weiss HJ. Scott syndrome: a disorder of platelet coagulant activity (PCA). Sem Hemat 1994; 31:312-319
- ↑ Zwaal FA, Comfurius P, Bevers EM. Scott syndrome, a bleeding disorder caused by defective scrambling of membrane phospholipids. Biochem Bioph Acta 2004; 1636:119-128
- ↑ Rosing J, Bevers EM, Comfurius P, Hemker HC, von Dieijen G, Weiss HJ, et al. Impaired factor X and prothrombin activation associated with decreased phospholipid exposure in platelets from a patient with a bleeding disorder. Blood 1985; 65:1557-1561.
- ↑ Toti F, Satta N, Fressinaud E, Meyer D, Freyssinet JM. Scott syndrome, characterized by impaired transmembrane migration of procoagulant phosphatidylserine and hemorrhagic complications, is an inherited disorder. Blood 1996; 87:1409-1415
- ↑ Elliott JI, Mumford AD, Albrecht C, Collins PW, Giddings JC, Higgins CF et al. Characterization of lymphocyte responses to Ca2+ in Scott syndrome. Thromb Haemost 2004; 91:412-415
- ↑ Sims PJ, Wiedmer T. Unraveling the mysteries of phospholipid scrambling. Thromb Haemost 2001; 86:266-275
- ↑ Zhou Q, Sims PJ, Wiedmer T. Expression of proteins controlling transbilayer movement of plasma membrane phospholipids in the B lymphocytes from a patient with Scott syndrome. Blood 1998; 92:1707-1712
- ↑ Weiss, HJ: Impaired platelet procoagulant mechanisms in patients with bleeding disorders. Sem. Thromb. Hemost. 35:233-241, 2009
- ↑ Suzuki J, Umeda M, Sims PJ, Nagata S. Calcium-dependent phospholipid scrambling by TMEM16F. Nature online, November 24, 2010
Further reading
- Heemskerk JWM, Bevers EM, Lindhout T. Platelet activation and blood coagulation, Thromb Haem 2002; 88:186-194
- Martinez MC, Martin S, Toti F, Fressinaud E, Dachary-Prigent J, Meyer D, et al. Significance of capacitative Ca2+ entry to the regulation of phoshatidylserine expression at the surface of stimulated cells. Biochemistry 1999; 38:10092-10098
- Munnix ICA, Harmsma M, Diddings JC, Collins PW, Feijge P, Comfurius JWM, et al. Store-mediated Ca2+ entry in the regulation of phoshatidylserine exposure in blood cells from Scott patients. Thromb Haemost 2003; 89:687-695
- Weiss HJ, Vicic WJ, Lages BA, Rogers J. Isolated deficiency of platelet procoagulant activity. Am J Med 1979; 67:206-213
- Miletich JP, Kane WH, Hofmann SL, Stanford N, Majerus PW. Deficiency of factor Xa-factor Va binding sites on the platelets of a patient with a bleeding disorder. Blood 1979; 54:1015-1022
- Bevers EM, Wiedmer T, Comfurius P, Shattil SJ, Weiss HJ, Zwaal RFA, et al. Defective Ca2+ induced microvesiculation and deficient expression of procoagulant activity in erythrocytes from a patient with a bleeding disorder: a study of the red blood cells of Scott syndrome. Blood 1992;79:380-388
- Kojima H, Newton-Nash D, Weiss HJ, Sims PJ, Zhao J, Wiedmer T. Production and characterization of transformed B-lymphocytes expressing the membrane defect of Scott Syndrome. J Clin Invest 1994; 94:2237-2244
- Stout JG, Basse F, Luhm RA, Weiss HJ, Wiedmer T, Sims PJ. Scott syndrome erythrocytes contain a membrane protein capable of mediating Ca2+-dependent transbilayer migration of membrane phospholipids. J Clin Invest 1997; 99:2232-2238
- Albrecht C, McVey JH, Elliott JI, Sardini A, Kasza I, Mumford AD, et al. A novel missense mutation in ABCA1 results in altered protein trafficking and reduced phosphatidylserine translocation in a patient with Scott syndrome. Blood 2005; 106:542-549
- Brooks MB, Catalfamo JL, Alex Brown H, Ivanova P, Lovaglio J. A hereditary bleeding disorder of dogs caused by a lack of platelet procoagulant activity. Blood 2002; 99:2434-2441