Supervised injection site

Supervised injection sites (SIS)[1] are medically supervised facilities designed to provide a hygienic environment in which people are able to consume illicit recreational drugs intravenously.[2] The legality of such a facility is dependent by location and political jurisdiction. Supervised injection sites are part of a harm reduction approach towards drug problems. The facilities provide sterile injection equipment, information about drugs and basic health care, treatment referrals, access to medical staff, and, at some facilities, counseling. Most programs prohibit the sale or purchase of recreational drugs at the facility.
Terminology
They are also known as overdose prevention centers (OPC),[3] supervised injection facilities,[4] safe consumption rooms,[5] safe injection sites,[1] safe injection rooms,[6] fix rooms,[7] fixing rooms,[8] safer injection facilities (SIF), drug consumption facilities (DCF),[2] drug consumption rooms (DCRs),[9] and harm reduction centers.[10]
Facilities
Australia
"Shooting galleries" (the term "shooting" is slang for injecting drugs) have existed for a long time; there were illicit for-profit facilities in Sydney, Australia during the 1990s. Authors differentiated the legally sanctioned sites in Australia from those examples in the care they provide. While the operators of the shooting galleries exemplified in Sydney had little regard for the health of their clients, modern supervised injection facilities are a professionally staffed health and welfare service.[11] The same journal describes the same facility in Australian context as "in general" may be defined as "legally sanctioned and supervised facilities designed to reduce the health and public order problems associated with illegal injection drug use"[11]
The legality of supervised injection is handled on a state-by state basis. New South Wales trialed a supervised injection site in Sydney in 2001, which was made permanent in 2010.[12] Victoria also opened a supervised injection site in Melbourne in 2018 on a trial basis; in 2020 the trial was extended for a further three years and a second site approved.[13]
Europe
The first professionally staffed service where drug injection was accepted emerged in the Netherlands during the early 1970s as part of the "alternative youth service" provided by the St. Paul's church in Rotterdam. At its peak it had two centers that combined an informal meeting place with a drop-in center providing basic health care, food and a laundering service. One of the centers was also a pioneer in providing needle-exchange. Its purpose was to improve the psychosocial function and health of its clients. The centers received some support from law enforcement and local government officials, although they were not officially sanctioned until 1996.[11]
The first modern supervised consumption site was opened in Berne, Switzerland in June, 1986.[14] Part of a project combatting HIV, the general concept of the café was a place where simple meals and beverages would be served, and information on safe sex, safe drug use, condoms and clean needles provided. Social workers providing counselling and referrals were also present. An injection room was not originally conceived, however, drug users began to use the facility for this purpose, and this soon became the most attractive aspect of the café. After discussions with the police and legislature, the café was turned into the first legally sanctioned drug consumption facility provided that no one under the age of 18 was admitted.[15]
During the 1990s additional legal facilities emerged in other cities in Switzerland, Germany and the Netherlands.[2][11] In the first decade of 2000, facilities opened in Spain, Luxembourg, and Norway.[2]
Whereas injection facilities in Europe often evolved from something else, such as different social and medical outreaches or perhaps a homeless shelter, the degree and quality of actual supervision varies. The history of the European centers also mean that there have been no or little systematic collection of data needed to do a proper evaluation of effectiveness of the scheme.[2]
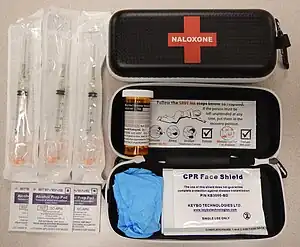
At the beginning of 2009 there were 92 facilities operating in 61 cities, including 30 cities in the Netherlands, 16 cities in Germany and 8 cities in Switzerland.[2] Denmark passed a law allowing municipalities to run "fix rooms" in 2012, and by the end of 2013 there were three open.[7] However, some of the very rationale for the projects in Sydney and Vancouver are specifically to gather data, as they are created as scientific pilot projects. The approach at the centers is also more clinical in nature, as they provide supervision by staff equipped and trained to administer oxygen or naloxone in the case of a heroin or other opioid overdose.[16]
Canada
There are 39 government authorized SCS in Canada as of July 2019. 19 in Ontario, 9 in British Columbia, 7 in Alberta and 4 in Quebec[17] An exemption to controlled substances law under Canadian Criminal Code is granted inside the facilities, but drug possession remains illegal outside the facility and there is no buffer zone around the facility.[17] Canada's first SCS, Insite in Downtown Eastside of Vancouver, commenced operation in 2003.[16] In August 2020, the largest SCS in North America ARCHES Lethbridge located in Lethbridge, Alberta closed shortly after province revoked their grant for misuse of grant funds.[18] It had been open since February 2018[19] and after it opened, it started causing calls for police service and opioid related EMS calls to the immediate vicinity.[20] Three weeks after its closure, the city already noticed a 36% decline in opioid related requests for emergency medical service.[21]
Expenditure
The average per-capita operating cost of government sanctioned sites are reported to be CAD$600 per unique-client; with the exception of the ARCHES Lethbridge which had a disproportionately high cost of CAD $3,200 per unique client.[20]
Unauthorized site in Alberta
In September 2020, a group in Lethbridge, Alberta led by an ARCHES employee started hosting an unauthorized SCS in public places in a tent.[22][23] The group did not have authorizations to operate an SCS or a permit to pitch a tent in the park. The organizer was issued citations for the tent; and the Lethbridge Police Service advised that users utilizing the unauthorized SCS would be arrested for drug possession, because exemptions do not apply to unauthorized sites.[24][25][26] This opening of this illegal drug consumption tent was controversial and became a subject of discussion at the City Council meeting.[27][28]
United States
The first government-authorized supervised injection site began operating in New York City on November 30, 2021. Though legal under city and state law, the site is arguably illegal under federal law, and relies on lack of enforcement by federal officials to keep operating.[29]
Clandestine injection sites have existed for years. There were illicit for-profit facilities in New York City during the 1980s. New England Journal of Medicine from July 2020 reports that an illegal SCS has been operating at an "undisclosed" city in the U.S. since 2014 where over 10,000 doses of illegal drugs have been injected over a five-year period.[30]
The organization Safehouse (formed in 2018) attempted to open a supervised injection site in Philadelphia February 2020 with the support of the city. Under pressure from neighbors, the owner of the first proposed location withdraw a lease offer.[31][32] United States District Attorney William McSwain sued to stop the Safehouse project, losing in district court in October 2019, but winning an injunction in January 2021 from a 3-judge panel of the United States Court of Appeals for the Third Circuit.[33]
In November, 2018, Denver city council approved a pilot program for a safe injection site with a 12-to-1 vote. The Drug Enforcement Administration's Denver field office and the United States Attorney's office for the District of Colorado issued a statement together on the proposed site[34] stating that "the operation of such sites is illegal under federal law. 21 U.S.C. Sec. 856 prohibits the maintaining of any premises for the purpose of using any controlled substance".
A safe injection site in the United States was projected to open in Philadelphia February 2020 but received strong opposition from its immediate neighbors.[35] In its counterarguments, the nonprofit Safehouse said its proposed operation was "a legitimate medical intervention, not illicit drug dens" and claimed protection under the Free Exercise Clause because "religious beliefs compel them to save lives at the heart of one of the most devastating overdose crises in the country".[36]
Jesse Harvey attempted to claim similar religious freedom protection by forming the Church of Safe Injection in Maine. After his death from a drug overdose, the organization obtained a relaxation in regulations from the governor of Maine and approval from the Maine CDC to operate as an authorized needle exchange in several cities (but not a supervised injection site).[37]
Local governments in San Francisco, Seattle, Boston, Vermont, Delaware, and Portland, Oregon have considered opening safe injection sites as well.[38][39] Plans to open an injection site in Somerville, Massachusetts in 2020 were delayed by the COVID-19 pandemic.[40]
Evaluations
In the late 1990s there were a number of studies available on consumption rooms in Germany, Switzerland and the Netherlands. “The reviews concluded that the rooms contributed to improved public and client health and reductions in public nuisance but stressed the limitations of the evidence and called for further and more comprehensive evaluation studies into the impact of such services.”[41] To that end, the two non-European injecting facilities, Australia’s Sydney Medically Supervised Injecting Centre (MSIC) and Canada’s Vancouver Insite Supervised Injection Site have had more rigorous research designs as a part of their mandate to operate.[42]
The NSW government has provided extensive funding for ongoing evaluations of the Sydney MSIC, with a formal comprehensive evaluation produced in 2003, 18 months after the centre was opened. Other later evaluations studied various aspects of the operation - service provision (2005), community attitudes (2006), referral and client health (2007) and a fourth (2007) service operation and overdose related events.[43] Other evaluations of drug-related crime in the area were completed in 2006, 2008 and 2010, the SAHA International cost-effectiveness evaluation in 2008 and a final independent KPMG evaluation in 2010.
The Vancouver Insite facility was evaluated during the first three years of its operation by researchers from the BC Center for Excellence in HIV/AIDS with published and some unpublished reports available. In March 2008 a final report was released that evaluated the performance of the Vancouver Insite against its stated objectives.
Some posit that safe injection sites help reduce improperly discarded needles in public, [44][45][46][47] including a report by the Canadian Mental Health Association in 2018.[48]
Client characteristics and utilization
The 2010 KPMG evaluation of the Sydney MSIC found that it had made service contact with its target population,[49] with 12,050 visitors to the Centre for a total of 604,022 injections between May 2001 and April 2010, where clients averaged 14 years of illicit drug use and where 39–51% across the various years were heroin injectors[50] and 35% in 2007 had experienced an overdose previously.[51]
The Drug Free Australia 2010 analysis found that the 7% of clients who attended the centre more than 98 times in a year were still injecting 80% of the time outside the centre, while the 26% who visited 10-98 times per year injected 95% of the time on the street, in a car, a toilet, at home or someone else’s home.[52] With injector safety the most prominent rationale for the establishment of injecting rooms, the analysis questioned such low utilization rates in light of the room’s capacity for 330 injections per day,[53] but where between 2001 and 2010 it had averaged just 185 injections per day.[52]
The Expert Advisory Committee for Insite[54] cited 8,000 people who had visited its facility, with 18% accounting for 80% of all visits to, less than 10% using the site for all injections, a median number of 8 visits across all clientele, and 600 visits per day, of which 80% were to inject, showing that the facility was near capacity. Drug Free Australia has noted that for the 1,506 injectors who most regularly use the centre, who would cumulatively inject somewhere between 6,000 and 9,000 times daily, the less than 500 injections in Insite daily represents at best one injection in every 12 by its highest utilizers inside the facility.
Two surveys of approximately 1,000 users established some key user characteristics – clients averaged 15 years of drug use, 51% injected heroin and 32% cocaine, 87% were infected with Hepatitis C virus and 17% with HIV, 20% were homeless with numerous others living in single resident rooms, 80% had been incarcerated, 21% were using methadone and 59% reported a non-fatal overdose during their lifetime.
European consumption rooms cater more so to users older than 30 years, mainly with problematic heroin and cocaine habits. Various studies have documented an ageing population of clients over time. Whereas in 1990, in one study, 50% of clients were 25 years or younger, by 2001 the percentage was 15%. Clients across European consumption rooms are characterized by heavy injecting drug use, a continuous use of illicit drugs and deriving from a poorer demographic. German studies found that between 19% and 27% of clients were from unstable accommodation. In the injecting rooms near Madrid, 42% of the marginalized target group were homeless, while the number was 60% for the Can Tunis area of Barcelona. In a German study 15% of clients had never accessed addiction treatment of any kind.[55]
Client utilization in the European situation is more difficult to analyze. Studies on sites in Frankfurt and Zurich found that clients used facilities 5 times a week[56] and in Rotterdam 6 times a week and twice in the previous 24 hours.[57] A study of clients in Frankfurt in 1997 found that 63% claimed to be daily visitors, while in another surveyed non-random sample from 18 German consumption rooms, 84% claimed use of the facility at least once weekly, with 51% claiming at least once per day utilization.[58]
Client referral
Evaluators of the Sydney MSIC found that over an eight-year period staff provided 47,396 other occasions of service (94.6 per 1,000 visits) including advice on drug and alcohol treatment on 7,856 occasions, 22,531 occasions where staff had provided vein care and safer injecting advice, with a total of 8,508 referrals to other services where 3,871 of those referrals were to treatment.[59] Of the 3,871 referrals to treatment 1,292 were to detox and 434 to abstinence-based rehabilitation or therapy.[60] The evaluators asserted that the MSIC was thereby evidenced as a gateway for treatment.[61]
Drug Free Australia has heavily criticized the MSIC referral rates to treatment as abnormally and unjustifiably low. They note that the 2010 MSIC evaluation does not give the percentage of clients referred to drug treatment, but that the 2007 evaluation records just 11% of clients over 6 years referred to treatment. They further cite the 2010 evaluation’s appeal to smoking cessation surveys which demonstrate that 20% of all tobacco smokers, using the most addictive of all commonly used drugs, are currently ready to quit at any point in time. Alternatively, the MSIC has had opportunity to continuously assist their clients over a period of many years and not just at a single point of time.[62]
The Expert Advisory Committee found that Insite had referred clients such that it had contributed to an increased use of detoxification services and increased engagement in treatment. Insite had encouraged users to seek counseling. Funding has been supplied by the Canadian government for detoxification rooms above Insite.[63]
SIS sites and social disorder
A longitudinal study—Urban Social Issues Study (USIS)—from January 2018 and February 2019—undertaken by University of Lethbridge's professor Em M. Pijl and commissioned by the City of Lethbridge, Alberta, Canada explore "any unintended consequences" of supervised consumption services (SCS) within the "surrounding community".[19]: 16 The USIS study was undertaken in response to a drug crisis in Lethbridge that impacted "many neighbourhoods in many different ways." Researchers studied the "perceptions and observations of social disorder by business owners and operators" in a neighborhood where SCS was introduced.[19]: 16 The report cautioned, that drug abuse-related antisocial behavior in Lethbridge, in particular, and in cities, in general, has increased, as the "quantity and type of drugs in circulation" increases. As the use of crystal meth eclipses the use of opiates, users exhibit more "erratic behavior". Crystal meth and other "uppers" also "require more frequent use" than "downers" like opiates.[19]: 11 The report also notes that not all social disorder in communities that have a SCS, can be "unequivocally and entirely attributed" to the SCS, partly because of the "ongoing drug epidemic."[19]: 11 Other variables that explain increased anti-social behaviour includes an increase in the number of people aggregating outdoors as part of seasonal trends with warmer temperatures.[19]: 16
Philadelphia's WPVI-TV Action News team traveled to Toronto, Canada in 2018 to make first hand field observations of several safe consumption sites already in operation. A drug addict interviewed by the reporter said she visits the site to obtain supply, but did not stick around and used the supplies to shoot up drugs elsewhere and acknowledged the site attracts drug users and drug dealers. A neighbor interviewed by the reporter said there was drug use before, but he reports it has increased since the site opened.[64]
WPVI-TV's Chad Pradelli narrated the news team's observation as:
Over the two days we sat outside several of Toronto's safe injection facilities, we witnessed prevalent drug use out front, drug deals, and even violence. We watched as one man harassed several people passing by on the sidewalk, even putting one in a chokehold. One guy decided to fight back and security arrived.[64]
Sydney, Australia
The Sydney MSIC client survey conducted in 2005, found that public injecting (defined as injecting in a street, park, public toilet or car), which is a high risk practice with both health and public amenity impacts, was reported as the main alternative to injecting at the MSIC by 78% of clients. 49% of clients indicated resorting to public injection if the MSIC was not available on the day of registration with the MSIC. From this, the evaluators calculated a total 191,673 public injections averted by the centre.[65]
Public amenity can be further improved by reduced numbers of publicly disposed needles and syringes. Data from the Sydney MSIC’s 2003 report indicated reductions in needles and syringe counts and resident and business-operator sightings of injections in public places decreased marginally but could not be certain that there was any effect by the MSIC beyond the heroin drought which had commenced some months prior to the opening of the MSIC.[66] The Drug Free Australia analysis pointed to the needle, syringe and public sighting decreases being almost exactly equivalent to the 20% decreases in the number of needles distributed from local pharmacies, needle exchanges and the MSIC, thereby indicating no clear impact by the MSIC.[67]
Vancouver, Canada
Observations before and after the opening of the Vancouver, British Columbia, Canada Insite facility indicated a reduction in public injecting. "Self-reports" of INSITE users and "informal observations" at INSITE, Sydney and some European SISs suggest that SISs "can reduce rates of public self-injection."[63]
Alberta, Canada
In response to the opioid epidemic in the province of Alberta, the Alberta Health Services's (AHS), Alberta Health, Indigenous Relations, Justice and Solicitor General including the Office of the Chief Medical Examiner, and the College of Physicians and Surgeons of Alberta met to discuss potential solutions. In the November 2016 Alberta Health report that resulted from that meeting, the introduction of supervised consumption services, along with numerous other responses to the crisis, was listed as a viable solution.[68]: 1 The 2016 Alberta Health report stated that, SIS, "reduce overdose deaths, improve access to medical and social supports, and are not found to increase drug use and criminal activity."[68]: 3
According to January 2020 Edmonton Journal editorial, by 2020 Alberta had seven SIS with a "100-per-cent success rate at reversing the more than 4,300 overdoses" that occurred from November 2017—when the first SIS opened in the province—until August 2019.[69]
Calgary
Safeworks Supervised Consumption Services (SCS)
Safeworks was located at the Sheldon M. Chumir Health Centre, which operated for several months, as a temporary facility, became fully operational starting April 30, 2018 with services available 24 hours, 7 days a week.[70]: 1 From the day it initially launched in October 30, 2017 to March 31, 2019, 71,096 people had used its services[70]: 1 The staff "responded to a total of 954 overdoses."[70]: 2 In one month alone, "848 unique individuals" made 5,613 visits to the SCS.[70]: 1 Its program is monitored by the Province of Alberta in partnership with the Institute of Health Economics.[70]: 2
In the City of Lethbridge's commissioned 2020 102-page report, the author noted that "Calgary’s Sheldon Chumir SCS has received considerable negative press about the "rampant" social disorder around the SCS, a neighbourhood that is mixed residential and commercial."[19]: 15 According to a May 2019 Calgary Herald article, the 250 meter radius around the safe consumption site Safeworks in Calgary located within the Sheldon M. Chumir Centre has seen a major spike in crime since its opening and described in a report by the police as having become "ground zero for drug, violent and property crimes in the downtown." Within this zone, statistics by the police in 2018 showed a call volume increase to the police by 276% for drug related matters 29% overall increase relative to the three-year average statistics.[71] In May 2019, the Calgary Herald, said that Health Canada announced in February 2019 of approval for Siteworks to operate for another year, conditional to addressing neighborhood safety issues, drug debris and public disorder.[72] There has been a plan for mobile safe consumption site intending to operate in the Forest Lawn, Calgary, Alberta, however in response to the statistics at the permanent site at the Sheldon M. Chumir Centre, community leaders have withdrawn their support.[73]
By September 2019, the number of overdose treatment at Safeworks spiked. The staff were overwhelmed and 13.5% of their staff took psychological leave. They have had dealt with 134 overdose reversals in 2019 which was 300% more than the same time period from the previous year. The center's director reported they're dealing with an average of one overdose reversal every other day.[74]
Lethbridge
ARCHES (Closed August 2020)
In response to the mounting death toll of drug overdose in Lethbridge, the city opened its first SCS in February, 2018.[19]: 15 The controversial[75] SCS, known as ARCHES was once the busiest SCS in North America.[76]
The province defunded ARCHES after an audit ordered by government discovered misuse and mismanagement of public monies. Around 70% of ARCHES funding comes from the province,[77] and it chose to shut it down on August 31, 2020 after the funding was revoked.[76] The audit found “funding misappropriation, non-compliance with grant agreement [and] inappropriate governance and organizational operations.”[77] The government is looking into the matter to determine if criminal charges are warranted.[78]
The City of Lethbridge commissioned a report that included an Urban Social Issues Study (USIS) which examined unintended consequences of the SIS site in Lethbridge.[19] The research found that in smaller cities, such as Lethbridge, that in communities with a SCS, social disorder may be more noticeable. The report's author, University of Lethbridge's Em M. Pijl, said that news media tended to the "personal experiences of business owners and residents who work and/or live near an SCS", which contrasts with "scholarly literature that demonstrates a lack of negative neighbourhood impacts related to SCSs."[19]: 14
Impact on blood-borne viruses
The 2003 evaluators of the Sydney MSIC found that it “had not increased blood-borne virus transmission”[49] with the data more specifically showing no improvement in HIV infection incidence, no improvement in Hep B infections,[79] either worse or no improvement (depending on the suburb studied) in new Hep C notifications,[80] no improvement in reuse of others' syringes and injecting equipment, no improvement in tests taken for HIV and Hep C and initial improvement in tests taken for Hep B but worsening again in 2002.[81] The 2010 evaluation found no measurable impact on blood-borne diseases.[82]
Impact on community levels of overdose
Over a nine-year period the Sydney MSIC managed 3,426 overdose-related events with not one fatality[83] while Vancouver’s Insite had managed 336 overdose events in 2007 with not a single fatality.
The 2010 MSIC evaluators found that over 9 years of operation it had made no discernible impact on heroin overdoses at the community level with no improvement in overdose presentations at hospital emergency wards.[84]: 19–20
Research by injecting room evaluators in 2007 presented statistical evidence that there had been later reductions in ambulance callouts during injecting room hours,[85][86][87] but failed to make any mention of the introduction of sniffer dog policing, introduced to the drug hot-spots around the injecting room a year after it opened.[88]
Site experience of overdose
While overdoses are managed on-site at Vancouver, Sydney and the facility near Madrid, German consumption rooms are forced to call an ambulance due to naloxone being administered only by doctors. A study of German consumption rooms indicated that an ambulance was called in 71% of emergencies and naloxone administered in 59% of cases. The facilities in Sydney and Frankfurt indicate 2.2-8.4% of emergencies resulting in hospitalization.[89]
Vancouver’s Insite yielded 13 overdoses per 10,000 injections shortly after commencement,[90] but in 2009 had more than doubled to 27 per 10,000.[91] The Sydney MSIC recorded 96 overdoses per 10,000 injections for those using heroin.[92] Commenting on the high overdose rates in the Sydney MSIC, the evaluators suggested that,
- “In this study of the Sydney injecting room there were 9.2 (sic) heroin overdoses per 1000 heroin injections in the centre. This rate of overdose is higher than amongst heroin injectors generally. The injecting room clients seem to have been a high-risk group with a higher rate of heroin injections than others not using the injection room facilities. They were more often injecting on the streets and they appear to have taken greater risks and used more heroin whilst in the injecting room.[93]
The Drug Free Australia 2010 analysis of the Sydney MSIC evaluations found overdose levels in the MSIC 32 times higher than clients’ own recorded histories of overdose prior to registering to use the facility.[94] The Drug Free Australia calculations compared the registration data for overdose histories published in the MSIC’s 2003 evaluation document, which allowed comparison rates of overdose from a period before a heroin drought reduced overdoses Australia-wide, with rates of overdose drawn from data in the 2010 evaluation. Drug Free Australia has expressed concern that the evaluators, in using injecting room overdose data to calculate quite incorrect 'lives saved' estimates, failed to examine the extent to which overdoses were over-represented in the injecting room against data they had available to them on clients’ prior histories of overdose.
Against other measures the Sydney MSIC’s overdose rate is highly disproportionate. Estimates of the number of dependent heroin users in Australia completed for the year 1997,[95] compared with estimates of the number of total non-fatal and fatal overdoses in Australia for 1997/98[96] yields a rate of 2 overdoses for every 10,000 injections against the MSIC’s rate of 96 overdoses for every 10,000 injections in the 2003 evaluation and rates as high as 146 overdoses per 10,000 injections in the year 2009/10.[97]
A review of the MSIC registration surveys recording each client’s previous overdose histories[98] reveals that MSIC clients’ previous overdose history were less prone to overdose than various other previously studied heroin injector cohorts in Australia.[99]
People living with HIV/AIDS
The results of a research project undertaken at the Dr. Peter Centre (DPC), a 24-bed residential HIV/AIDS care facility located in Vancouver, were published in the Journal of the International AIDS Society in March 2014, stating that the provision of supervised injection services at the facility improved health outcomes for DPC residents. The DPC considers the incorporation of such services as central to a "comprehensive harm reduction strategy" and the research team concluded, through interviews with 13 residents, that "the harm reduction policy altered the structural-environmental context of healthcare services and thus mediated access to palliative and supportive care services", in addition to creating a setting in which drug use could be discussed honestly. Highly active antiretroviral therapy (HAART) medication adherence and survival are cited as two improved health outcomes.[100]
Calculations of intervention
The European Monitoring Centre (EMCDDA) 2004 Review of Drug Consumption Rooms[2] calculated the number of lives saved for all 25 drug consumption rooms across Germany. It calculated from known overdose mortality rates per 100 dependent heroin users (2%) and the number of injections per 100 person years per dependent heroin user (1,000 injections per year per user). Their calculation indicated that 100 dependent heroin users, cumulatively injecting 100,000 times a year, would statistically have 2 overdose fatalities annually. Thus 500,000 injections results in 10 expected fatalities averted by the entirety of injecting facilities across Germany.
Drug Free Australia has noted that the EMCDDA review’s 2% overdose fatality rate appears excessive in light of mortality studies done by the EMCDDA for 5 European countries, (Germany was not included, but Spain, with the highest heroin overdose mortality, was still well below 2%). The percentages by country were Barcelona, Spain 1.4%; Rome, Italy 0.2%; Sweden 0.7%; Amsterdam, Netherlands unknown; Vienna, Austria 0.2%.[101]
The Canadian Expert Advisory Committee 2008 review of Insite did not declare the method by which it concluded that 1.08 lives are saved by the facility each year,[102] but Drug Free Australia claims that the EMCDDA method, used with Canadian data and assumptions, yields the same result.[103] Canadian heroin mortality in 2002/3 was roughly the same as Australia’s at 1% (958 deaths from more than 80,000 dependent heroin users)[104] and mortality percentages for 2006 or 2007, Drug Free Australia claims, might well be expected to be little changed. Further, the Expert Advisory Committee clearly state their assumption that a typical Canadian heroin user injects 4 times daily.[105]
The conclusion of the 2003 Sydney MSIC evaluators was that “a small number of opioid overdoses managed at the MSIC might have been fatal had they occurred elsewhere”, calculating that the centre had saved 4 lives per annum during the evaluation period.[106] Estimates were directly calculated from the 329 heroin overdose interventions in the centre. A later SAHA International evaluation of the MSIC calculated 25 lives saved by the facility in a single year.[107]
Drug Free Australia cites two statistics together which demonstrate that the Sydney MSIC cannot statistically claim to save even one life per year. The first is that 1% of dependent heroin users die from fatal overdose each year in Australia. The second is that a dependent heroin user averages ‘at least’ three injections per day according to the MSIC 2003 evaluation’s researchers. Taking these two statistics together, it is clear that the injecting room would need to host 300 injections per day (ie enough heroin injections for 100 heroin addicts injecting 3 times daily) before they could claim they had saved the life of the one (1%) of those 100 who would have died annually. But the injecting room averages just half that number with less than 150 opiate injections per day. Drug Free Australia has shown that the 2003 and 2008 MSIC evaluators indefensibly failed to factor the vastly elevated number of overdoses in the centre into their calculations of lives saved.[108]
Crime
The Sydney MSIC was judged by its evaluators to have caused no increase in crime[49] and not to have caused a ‘honey-pot effect’ of drawing users and drug dealers to the Kings Cross area.[109] The Drug Free Australia analysis pointed to data within the report clearly demonstrating that drug-related loitering and drug dealing worsened at the station entrance 25 metres opposite the MSIC[110] and at the rear door of the centre.[111] A later 2010 evaluation of crime in Kings Cross claimed that drug-related crime had decreased at the same rate as the rest of Sydney after a heroin shortage intervened 6 months before the MSIC opened, but Drug Free Australia has asserted that the evaluators failed to make any mention or assessment of the impact of police sniffer dogs introduced 12 months after the MSIC opened to deter drug dealers and users from the back lanes of Kings Cross, which might well be expected to have decreased drug-related crime more than areas of Sydney not policed by sniffer dogs.[112]
Testimony of ex-clients reported to the NSW Legislative Council[113] alleged that the extremely high overdose rates were due to clients experimenting with poly-drug cocktails and higher doses of heroin in the knowledge that staff were present to ensure their safety. The 2003 evaluation explanation for high overdose rates citing greater amounts of heroin used[114] has been cited by Drug Free Australia as cause for concern. NSW Member of Parliament, Andrew Fraser, made the same allegation regarding the MSIC as a site for experimentation, citing testimony of another ex-client in a Parliamentary speech in 2010.[115]
Observations before and after the opening of Insite indicated no increases in drug dealing or petty crime in the area. There was no evidence that the facility influenced drug use in the community, but concerns that Insite ‘sends the wrong message’ to non-users could not be addressed from existing data.[116] The European experience has been mixed.[117]
Financial impropriety by SCS service providers
Audit of Lethbridge ARCHES SCS by Deloitte accounting firm ordered by the Alberta provincial government found the SCS had $1.6 million in unaccounted funds between 2017 and 2018; additionally they've found led $342,943 of grant funds had been expended on senior executive compensation despite the grant agreement allowing only $80,000. Beyond this, an additional $13,000 was spent on parties, staff retreats, entertainment and gift cards,[78] and numerous other inappropriate expenditures.[78]
Community perception
316 residents and 210 business completed surveys regarding the MSIC in 2005.. The community survey conducted by NSW Department of Health in Kings Cross area of NSW, Australia in 2005 evaluation indicated 73% of residents, (a reduction from 78% in 2003), and 68% of business operators supported the MSIC's presence.[118] The evaluation commented that residents without landline telephones were excluded from the survey. Contesting the reliability of these evaluation surveys is a 2010 petition to the NSW Parliament by 63 business owners immediately surrounding the MSIC to move the facility elsewhere because it has adversely affected their businesses.[119]
The Expert Advisory Committee for Vancouver’s Insite found that health professionals, local police, the local community and the general public have positive or neutral views of the service, with opposition decreasing over time.[116]
Drug Free Australia has expressed concern that supporters, staff and various NSW politicians continually has represented each overdose intervention in the centre to the Australian media as a life saved, when such an equation was clearly false.[120]
Predicted cost effectiveness
The cost of running Insite per annum is $3 million Canadian. Mathematical modeling showed cost to benefit ratios of one dollar spent ranging from 1.5 to 4.02 in benefit. However, the Expert Advisory Committee expressed reservation about the certainty of Insite’s cost effectiveness until proper longitudinal studies had been undertaken. Mathematical models for HIV transmissions foregone had not been locally validated and mathematical modeling from lives saved by the facility had not been validated.[63] The Sydney MSIC cost upwards of $2.7 million Australian per annum in 2007.[121] Drug Free Australia has asserted that in 2003 the cost of running the Sydney MSIC equated to 400 NSW government-funded rehabilitation places[122] while the Health Minister for the Canadian Government, Tony Clements, has stated that the money for Insite would be better spent on treatment for clients.[123]
See also
- Drug liberalization
- Drug policy of the Soviet Union
- Drug policy reform
- Illicit drug use in Australia
- Needle and syringe programmes
- Responsible drug use
References
- 1 2 Alan Ogborne; et al. (March 31, 2008). "Vancouver's INSITE service and other Supervised injection sites: What has been learned from research? - Final report of the Expert Advisory Committee". Health Canada.
- 1 2 3 4 5 6 7 Dagmar Hedrich; et al. (April 2010). "Chapter 11: Drug consumption facilities in Europe and beyond". Harm reduction: evidence, impacts and challenges. EMCDDA.
- ↑ "Overdose Prevention Centers" (PDF).
- ↑ Academies, Committee on the Prevention of HIV Infection Among Injecting Drug Users in High-Risk Countries, Board on Global Health, Institute of Medicine of the National (2007). Preventing HIV infection among injecting drug users in high-risk countries an assessment of the evidence. Washington, D.C.: National Academies Press. doi:10.17226/11731. ISBN 978-0-309-10280-3.
- ↑ Learmonth, Andrew (17 December 2020). "Boris Johnson pledges to discuss safe drug consumption rooms for users". The National. Retrieved 21 January 2021.
- ↑ Townsend, Mark (17 August 2019). "Safe injection rooms are key to halting rise in drug deaths – expert". The Guardian. Retrieved 21 January 2021.
- 1 2 "Denmark's 'Fix Rooms' Give Drug Users a Safe Haven".
- ↑ Busby, Mattha (21 November 2018). "How 'fixing rooms' are saving the lives of drug addicts in Europe". The Guardian. Retrieved 28 January 2021.
- ↑ Easton, Mark (12 October 2017). "Are UK drug consumption rooms likely?". BBC News. Retrieved 21 January 2021.
- ↑ Felice J. Freyer (22 Jun 2021). "A government-sanctioned place to inject illicit drugs? It may come first to Somerville". The Boston Globe.
- 1 2 3 4 Dolan, Kate; Kimber, Jo; Fry, Craig; Fitzgerald, John; Mcdonald, David; Trautman, Franz (2000). "Drug consumption facilities in Europe and the establishment of supervised injection centres in Australia" (PDF). Drug and Alcohol Review. 19 (3): 337–346. doi:10.1080/713659379. Archived from the original (PDF) on 2004-09-24.
- ↑ Thomas, Matthew. "Sydney's Medically Supervised Injecting Centre". Australian Parliamentary Library. Retrieved 28 October 2020.
- ↑ "Medically supervised injecting room". Health.vic. Retrieved 28 October 2020.
- ↑ Hedrich, Dagmar (February 2004). "European report on drug consumption rooms" (PDF). European Monitoring Centre for Drugs and Drug Addiction. Retrieved October 5, 2020.
- ↑ Robert Haemmig; Ingrid van Beek (2005). "13 Supervised Injecting Room". In Richard Pates; Andrew McBride; Karin Arnold (eds.). Injecting Illicit Drugs. Blackwell Publishing. pp. 160–169. ISBN 978-1-4051-1360-1.
- 1 2 Van Beek, Ingrid (2004). In the eye of the needle: Diary of medically supervised injecting centre. Crows Nest: Allen & Unwin. ISBN 978-1-74114-381-2. OCLC 57515258.
- 1 2 "Debate over supervised consumption sites ramps up across Alberta". Global News. Retrieved 2020-10-07.
- ↑ Roulston, Tom; Nixon, Liam (July 23, 2020). "ARCHES audit findings turned over to Lethbridge police for investigation". Global News. Retrieved 2020-09-27.
- 1 2 3 4 5 6 7 8 9 10 Pijl, Em M. (January 13, 2020). Urban social issues study: Impacts of the Lethbridge supervised consumption site on the local neighbourhood (PDF) (Report). University of Lethbridge for the City of Lethbridge. p. 102. Retrieved January 26, 2020. Report commissioned by the City of Lethbridge
- 1 2 Vogt, Terry (2020-03-05). "Government review says Lethbridge SCS has 'most problems in the province'". Calgary. Retrieved 2020-10-07.
- ↑ Labby, Bryan (September 26, 2020). "3 weeks after province ends funding for injection site, unsanctioned space opens in Lethbridge". CBC News.
- ↑ Gunn, Connor. "Galt Gardens pop-up injection site moves location on 2nd night". Lethbridge News Now. Retrieved 2020-09-27.
- ↑ "Unsanctioned injection site sets up in Galt Gardens". The Lethbridge Herald - News and Sports from around Lethbridge. 2020-09-26. Retrieved 2020-09-27.
- ↑ Ferris, Danica (September 29, 2020). "Pop-up overdose prevention site operators fined $300 by City of Lethbridge". Global News. Retrieved 2020-10-03.
- ↑ "Lethbridge group sets up unsanctioned overdose prevention site in Galt Gardens". Global News. Retrieved 2020-09-27.
- ↑ Korol, Todd (October 5, 2020). "Lethbridge drug-consumption site seeks Health Canada's permission to operate". The Globe and Mail. Retrieved 2020-10-07.
- ↑ Goulet, Justin (September 29, 2020). "Organizer of pop-up injection site issued fine". Lethbridge News Now. Retrieved 2020-10-01.
- ↑ Barrow, Tyler (2020-09-28). "Protestors gather outside Lethbridge city hall frustrated over pop-up overdose prevention site". Calgary. Retrieved 2020-09-29.
- ↑ New York City allows the nation's 1st supervised consumption sites for illegal drugs
- ↑ Kral, Alex H.; Lambdin, Barrot H.; Wenger, Lynn D.; Davidson, Pete J. (2020-08-06). "Evaluation of an Unsanctioned Safe Consumption Site in the United States". New England Journal of Medicine. 383 (6): 589–590. doi:10.1056/NEJMc2015435. ISSN 0028-4793. PMID 32640126.
- ↑ "Safehouse drops South Philly plans, looks to Kensington after judge suspends launch". Billy Penn. Retrieved 2020-10-07.
- ↑ Lauren del Valle and Dakin Andone. "Plans are on hold for a Philadelphia safe-injection site to combat overdoses". CNN. Retrieved 2020-10-07.
- ↑ In Philadelphia, Judges Rule Against Opening 'Supervised' Site To Inject Opioids
- ↑ KKTV (December 4, 2018). "DEA responds to proposed safe injection site in Colorado for illegal drugs". KKTV. Retrieved 2019-04-20.
- ↑ TANENBAUM, MICHAEL (February 26, 2020). "Safehouse's plan to open overdose prevention site in South Philly sparks contentious reaction". www.phillyvoice.com. Retrieved 2020-10-07.
- ↑ Whelan, Aubrey (April 3, 2019). "Supervised injection site supporters countersue feds, saying their Philly mission comes from religious and medical imperatives". The Inquirer Daily News. Retrieved 2019-04-20.
- ↑ Church of Safe Injection gets Maine CDC approval for needle program
- ↑ Cities Planning Supervised Drug Injection Sites Fear Justice Department Reaction
- ↑ Hayes, Elizabeth (March 15, 2018). "A legal site in Portland to inject heroin? Elected officials, advocates explore the idea". Portland Business Journal. Retrieved April 28, 2019.
- ↑ Somerville Delays Plan To Open First Supervised Drug Use Clinic In Massachusetts
- ↑ EMCDDA"European report on drug consumption rooms" (PDF). 2004. p. 27. Retrieved 2010-04-28.
- ↑ EMCDDA "Harm Reduction: Evidence, Impacts and Challenges". 2010. p. 308. Retrieved 2010-06-09.
- ↑ "MSIC Evaluations". 2008. Retrieved 2010-01-09.
- ↑ Townsend, Mark (17 August 2019). "Safe injection rooms are key to halting rise in drug deaths – expert". The Guardian. Retrieved 1 December 2021.
- ↑ Holpuch, Amanda (8 August 2017). "Secret supervised drug injection facility has been operating at US site for years". The Guardian. Retrieved 1 December 2021.
- ↑ Smith, Callum (9 August 2019). "Discarded needles prompt calls for safe injection sites, more addictions supports in N.B." Global News. Retrieved 1 December 2021.
- ↑ Dubinski, Kate (2 May 2018). "Why this children's mentoring program is supporting supervised consumption sites". CBC. Retrieved 1 December 2021.
- ↑ MacLean, Cameron (18 April 2018). "Supervised injection site needed for drug users in Manitoba: Canadian Mental Health Association report". CBC News. Retrieved 1 December 2021.
- 1 2 3 2003 MSIC Evaluation Committee "Final Report of the Evaluation of the Sydney Medically Supervised Injecting Centre" (PDF). Archived from the original (PDF) on 2009-10-29. Retrieved 2010-01-09. 2003 p. xvi
- ↑ name=KPMG "Further Evaluation of the Medically Supervised Injecting Centre during its extended Trial period (2007-2011)" (PDF). Retrieved 2010-10-23. pp. 14, 85
- ↑ NCHECR, "Sydney Medically Supervised Injecting Centre Evaluation Report No. 4" (PDF). Archived from the original (PDF) on 2009-10-29. Retrieved 2010-01-09. 2007 pp. 14-17
- 1 2 "Drug Free Australia Analysis of the KPMG Injecting Room Evaluation" (PDF). Drug Free Australia. 2010. Retrieved 2010-10-23. p. 4
- ↑ 2003 MSIC Evaluation Committee "Final Report of the Evaluation of the Sydney Medically Supervised Injecting Centre" (PDF). Archived from the original (PDF) on 2009-10-29. Retrieved 2010-01-09. 2003 p. 38
- ↑ see Research Conclusions and Limitations - 1. INSITE Utilization and User Characteristics "Final Report of the Vancouver Insite Expert Advisory Committee". 2008-04-03. Retrieved 2010-04-19.
- ↑ Hedrich, D "A Report on European Consumption Rooms" (PDF). Retrieved 2010-05-28. EMCDDA 2004 pp. 31-33
- ↑ EMCDDA"European report on drug consumption rooms" (PDF). Retrieved 2010-04-28. 2004 pp. 35–36
- ↑ Eur Addict Res 2003;9:94–100 Van Der Poel, Agnes; Barendregt, Cas; Van De Mheen, Dike (2003). "Drug Consumption Rooms in Rotterdam: An Explorative Description". European Addiction Research. 9 (2): 94–100. doi:10.1159/000068807. PMID 12644736. S2CID 37030027.
- ↑ Hedrich, D "A Report on European Consumption Rooms" (PDF). Retrieved 2010-05-28. EMCDDA 2004 p. 35
- ↑ name=KPMG "Further Evaluation of the Medically Supervised Injecting Centre during its extended Trial period (2007-2011)" (PDF). Retrieved 2010-10-23. pp. 24, 115–16
- ↑ name=KPMG "Further Evaluation of the Medically Supervised Injecting Centre during its extended Trial period (2007-2011)" (PDF). Retrieved 2010-10-23. p. 129
- ↑ name=KPMG "Further Evaluation of the Medically Supervised Injecting Centre during its extended Trial period (2007-2011)" (PDF). Retrieved 2010-10-23. p. 3
- ↑ "Drug Free Australia Analysis of the KPMG Injecting Room Evaluation" (PDF). Drug Free Australia. 2010. Retrieved 2010-10-23. pp. 17–18
- 1 2 3 see "Final Report of the Vancouver Insite Expert Advisory Committee". 2008-04-03. Retrieved 2010-04-19.
- 1 2 Pradelli, Chad (July 18, 2018). "Opioid Crisis: Action News investigates safe injection sites in Canada". WPVI-TV Action News. Retrieved March 22, 2020.
- ↑ NCHECR, "Sydney Medically Supervised Injecting Centre Evaluation Report No. 4" (PDF). Archived (PDF) from the original on 2018-04-17. Retrieved 2019-02-06. 2007 pp. 7, 39
- ↑ 2003 MSIC Evaluation Committee "Final Report of the Evaluation of the Sydney Medically Supervised Injecting Centre" (PDF). Archived from the original (PDF) on 2009-10-29. Retrieved 2010-01-09. 2003 p. 125
- ↑ "The Case for Closure - Detailed Evidence" (PDF). Drug Free Australia. 2008. Archived from the original (PDF) on 2011-02-15. Retrieved 2010-01-09. p. 32
- 1 2 "Responding to Alberta's Opioid Crisis" (PDF). Alberta Health Services (AHS), Office of the Chief Medical Officer of Health. Public progress report: 9. November 30, 2016. Retrieved January 26, 2020.
- ↑ McGarrigle, Colin; Breakenridge, Dave; Mah, Bill (January 24, 2020). "Balanced view of consumption sites required". Edmonton Journal. Editorial. Retrieved January 26, 2020.
- 1 2 3 4 5 "March 2019: Supervised Consumption Services" (PDF), Alberta Health Services (AHS), Safeworks Monthly Report, p. 4, April 11, 2019, retrieved January 26, 2020
- ↑ Hudes, Sammy (May 21, 2019). "Crime near Calgary's only safe consumption site remains a concern". Calgary Herald. Retrieved January 26, 2020.
- ↑ Breakenridge, Rob (2019-02-05). "Breakenridge: Fix crime issues around Safeworks or risk losing it | Calgary Herald". Retrieved 2019-10-11.
- ↑ Logan, Shawn (2019-02-05). "Forest Lawn withdraws support for mobile safe consumption vehicle | Calgary Herald". Retrieved 2019-10-11.
- ↑ Villani, Mark (September 12, 2019). "Spike in overdose treatments overwhelms staff at Calgary shelters". CTV News Calgary. Retrieved October 25, 2019.
- ↑ Goulet, Justin. "ARCHES ceases supervised consumption services in Lethbridge". Lethbridge News Now. Retrieved 2020-09-26.
- 1 2 Fletcher, Robson (September 23, 2020). "Opioid overdoses spike amid COVID-19 pandemic, with more than 3 Albertans dying per day". CBC.
- 1 2 "MLA Shannon Phillips and others react to ARCHES losing provincial funding after government-ordered audit". Global News. Retrieved 2020-09-26.
- 1 2 3 Bourne, Kirby; Therien, Eloise (July 16, 2020). "Government pulls grant funding from Lethbridge safe consumption site citing fund mismanagement". Globalnews.ca. Retrieved 2020-09-26.
- ↑ 2003 MSIC Evaluation Committee "Final Report of the Evaluation of the Sydney Medically Supervised Injecting Centre" (PDF). Archived from the original (PDF) on 2009-10-29. Retrieved 2010-01-09. 2003 pp. 71–72
- ↑ 2003 MSIC Evaluation Committee "Final Report of the Evaluation of the Sydney Medically Supervised Injecting Centre" (PDF). Archived from the original (PDF) on 2009-10-29. Retrieved 2010-01-09. 2003 p. 80
- ↑ 2003 MSIC Evaluation Committee "Final Report of the Evaluation of the Sydney Medically Supervised Injecting Centre" (PDF). Archived from the original (PDF) on 2009-10-29. Retrieved 2010-01-09. 2003 pp. 91–98
- ↑ name=KPMG "Further Evaluation of the Medically Supervised Injecting Centre during its extended Trial period (2007-2011)" (PDF). Retrieved 2010-10-23. p. 4
- ↑ name=KPMG "Further Evaluation of the Medically Supervised Injecting Centre during its extended Trial period (2007-2011)" (PDF). Retrieved 2010-10-23. p. 2
- ↑ "Further Evaluation of the Medically Supervised Injecting Centre during its extended Trial period (2007-2011)" (PDF). Retrieved 2010-10-23.
- ↑ Salmon, Allison; Van Beek, Ingrid; Amin, Janaki; Kaldor, John; Maher, Lisa (February 2010). "The impact of a supervised injecting facility on ambulance call-outs in Sydney, Australia". Addiction. 105 (4): 676–683. doi:10.1111/j.1360-0443.2009.02837.x. PMID 20148794. Archived from the original on 2013-01-05.
- ↑ Beletsky, Leo; Davis, Corey S; Anderson, Evan; Burris, Scott (February 2008). "The law (and politics) of safe injection facilities in the United States". American Journal of Public Health. 98 (2): 231–7. doi:10.2105/AJPH.2006.103747. PMC 2376869. PMID 18172151.
- ↑ Kerr, Thomas; Kimber, Jo; Rhodes, Tim (January 2007). "Drug use settings: an emerging focus for research and intervention". The International Journal on Drug Policy. 18 (1): 1–4. doi:10.1016/j.drugpo.2006.12.016. PMID 17689337.
- ↑ "Police to crack down on Kings Cross drug trade". Retrieved 2010-01-09. 2003
- ↑ Hedrich, D "A Report on European Consumption Rooms" (PDF). Retrieved 2010-05-28. EMCDDA 2004 p. 46
- ↑ Kerr T, Tyndall MW, Lai C, Montaner JSG, Wood E. "Drug-related overdoses within a medically supervised safer injection facility" (PDF). 2008. Retrieved 2010-05-01.
- ↑ see "User Statistics". 2009. Retrieved 2010-05-01.
- ↑ 2003 MSIC Evaluation Committee "Final Report of the Evaluation of the Sydney Medically Supervised Injecting Centre" (PDF). Archived from the original (PDF) on 2009-10-29. Retrieved 2010-01-09. 2003 p. 24
- ↑ 2003 MSIC Evaluation Committee "Final Report of the Evaluation of the Sydney Medically Supervised Injecting Centre" (PDF). Archived from the original (PDF) on 2009-10-29. Retrieved 2010-01-09. 2003 p. 59
- ↑ "Drug Free Australia Analysis of the KPMG Injecting Room Evaluation" (PDF). Drug Free Australia. 2010. Retrieved 2010-10-23. p. 9
- ↑ Hall W, Ross J, Lynskey M, Law M, Degenhardt L Degenhardt, Louisa J.; Law, Matthew G.; Lynskey, Michael T.; Ross, Joanne E.; Hall, Wayne D. (2000-11-20). "How many dependent heroin users are there in Australia?". The Medical Journal of Australia. 173 (10): 528–531. doi:10.5694/j.1326-5377.2000.tb139321.x. PMID 11194736. S2CID 38177886. Retrieved 2010-05-01. MJA 2000; 173: 528-531
- ↑ Warner-Smith M, Lynskey M, Darke S, Hall W "Heroin overdose: prevalence, correlates, consequences and interventions" (PDF). Archived from the original (PDF) on 2014-06-21. Retrieved 2010-05-01. p. 12
- ↑ name=KPMG "Further Evaluation of the Medically Supervised Injecting Centre during its extended Trial period (2007-2011)" (PDF). Retrieved 2010-10-23. p. 159
- ↑ 2003 MSIC Evaluation Committee "Final Report of the Evaluation of the Sydney Medically Supervised Injecting Centre" (PDF). Archived from the original (PDF) on 2009-10-29. Retrieved 2010-01-09. 2003 p. 16
- ↑ "The Case for Closure - Detailed Evidence" (PDF). Drug Free Australia. 2008. Archived from the original (PDF) on 2011-02-15. Retrieved 2010-01-09. p. 55
- ↑ McNeil, R; et al. (13 March 2014). "Impact of supervised drug consumption services on access to and engagement with care at a palliative and supportive care facility for people living with HIV/AIDS: a qualitative study". Journal of the International AIDS Society. 17 (1): 18855. doi:10.7448/IAS.17.1.18855. PMC 3955762. PMID 24629844.
- ↑ "Drug Free Australia Analysis of the KPMG Injecting Room Evaluation" (PDF). Drug Free Australia. 2010. Retrieved 2010-10-23. pp. 7–8
- ↑ see Executive Summary – Cost Benefit/Effectiveness section "Final Report of the Vancouver Insite Expert Advisory Committee". 2008-04-03. Retrieved 2010-04-19.
- ↑ "Drug Free Australia Analysis of the KPMG Injecting Room Evaluation" (PDF). Drug Free Australia. 2010. Retrieved 2010-10-23. p. 8
- ↑ Popova S, Rehm J, Fischer B "An overview of illegal opioid use and health services utilization in Canada" (PDF). Public Health=2010-10-23. 2006. p. 1
- ↑ see Background section"Final Report of the Vancouver Insite Expert Advisory Committee". 2008-04-03. Retrieved 2010-04-19.
- ↑ 2003 MSIC Evaluation Committee "Final Report of the Evaluation of the Sydney Medically Supervised Injecting Centre" (PDF). Archived from the original (PDF) on 2009-10-29. Retrieved 2010-01-09. 2003 pp. 58–59
- ↑ name=KPMG "Further Evaluation of the Medically Supervised Injecting Centre during its extended Trial period (2007-2011)" (PDF). Retrieved 2010-10-23. p. 198
- ↑ "Drug Free Australia Analysis of the KPMG Injecting Room Evaluation" (PDF). Drug Free Australia. 2010. Retrieved 2010-10-23. pp. 9–10
- ↑ 2003 MSIC Evaluation Committee "Final Report of the Evaluation of the Sydney Medically Supervised Injecting Centre" (PDF). Archived from the original (PDF) on 2009-10-29. Retrieved 2010-01-09. 2003 p. 204
- ↑ 2003 MSIC Evaluation Committee "Final Report of the Evaluation of the Sydney Medically Supervised Injecting Centre" (PDF). Archived from the original (PDF) on 2009-10-29. Retrieved 2010-01-09. 2003 pp. 146–47
- ↑ 2003 MSIC Evaluation Committee "Final Report of the Evaluation of the Sydney Medically Supervised Injecting Centre" (PDF). Archived from the original (PDF) on 2009-10-29. Retrieved 2010-01-09. 2003 p. 140
- ↑ "Drug Free Australia Analysis of the KPMG Injecting Room Evaluation" (PDF). Drug Free Australia. 2010. Retrieved 2010-10-23. pp. 12–13
- ↑ NSW Parliament Hansard "Rev Dr Gordon Moyes Injecting Room Hansard". Retrieved 2010-01-09. 26 June 2007
- ↑ 2003 MSIC Evaluation Committee "Final Report of the Evaluation of the Sydney Medically Supervised Injecting Centre" (PDF). Archived from the original (PDF) on 2009-10-29. Retrieved 2010-01-09. 2003 pp. 62–63
- ↑ Andrew Fraser MP "NSW Hansard – 21 October 2010". NSW Hansard. 2010. Retrieved 2010-10-23.
- 1 2 see Executive Summary of "Final Report of the Vancouver Insite Expert Advisory Committee". 2008-04-03. Retrieved 2010-04-19.
- ↑ see Sections A7 to A9 of Appendix B "Final Report of the Vancouver Insite Expert Advisory Committee". 2008-04-03. Retrieved 2010-04-19.
- ↑ NCHECR "Interim Evaluation Report No 2: Evaluation of Community Attitudes towards the Sydney MSIC, March 2006" (PDF). Archived (PDF) from the original on 2007-09-02. Retrieved 2010-01-09. p. 3
- ↑ Pru Goward MP "NSW Hansard – 21 October 2010". NSW Hansard. 2010. Retrieved 2010-10-23.
- ↑ "The Case for Closure" (PDF). Drug Free Australia. 2008. p. 2. Retrieved 2010-01-09.
- ↑ NCHECR, "Sydney Medically Supervised Injecting Centre Evaluation Report No. 4" (PDF). Archived from the original (PDF) on 2009-10-29. Retrieved 2010-01-09. 2007 p. 35
- ↑ Drug Free Australia "The Case for Closure: Detailed Evidence" (PDF). p. 39. Archived from the original (PDF) on 2011-02-15. Retrieved 2010-01-09.
- ↑ Clement, T. (2 June 2008). "Canadian Parliament Hansard". Retrieved 2010-05-31.
External links
- Community member in Philadelphia objects to SCS - Video on NBC 10 Philadelphia journalist's confirmed Twitter account.