Tidal volume
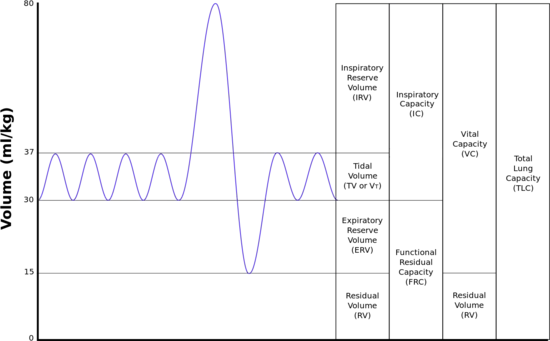 | |
| TLC | Total lung capacity: the volume in the lungs at maximal inflation, the sum of VC and RV. |
|---|---|
| TV | Tidal volume: that volume of air moved into or out of the lungs during quiet breathing (TV indicates a subdivision of the lung; when tidal volume is precisely measured, as in gas exchange calculation, the symbol TV or VT is used.) |
| RV | Residual volume: the volume of air remaining in the lungs after a maximal exhalation |
| ERV | Expiratory reserve volume: the maximal volume of air that can be exhaled from the end-expiratory position |
| IRV | Inspiratory reserve volume: the maximal volume that can be inhaled from the end-inspiratory level |
| IC | Inspiratory capacity: the sum of IRV and TV |
| IVC | Inspiratory vital capacity: the maximum volume of air inhaled from the point of maximum expiration |
| VC | Vital capacity: the volume of air breathed out after the deepest inhalation. |
| VT | Tidal volume: that volume of air moved into or out of the lungs during quiet breathing (VT indicates a subdivision of the lung; when tidal volume is precisely measured, as in gas exchange calculation, the symbol TV or VT is used.) |
| FRC | Functional residual capacity: the volume in the lungs at the end-expiratory position |
| RV/TLC% | Residual volume expressed as percent of TLC |
| VA | Alveolar gas volume |
| VL | Actual volume of the lung including the volume of the conducting airway. |
| FVC | Forced vital capacity: the determination of the vital capacity from a maximally forced expiratory effort |
| FEVt | Forced expiratory volume (time): a generic term indicating the volume of air exhaled under forced conditions in the first t seconds |
| FEV1 | Volume that has been exhaled at the end of the first second of forced expiration |
| FEFx | Forced expiratory flow related to some portion of the FVC curve; modifiers refer to amount of FVC already exhaled |
| FEFmax | The maximum instantaneous flow achieved during a FVC maneuver |
| FIF | Forced inspiratory flow: (Specific measurement of the forced inspiratory curve is denoted by nomenclature analogous to that for the forced expiratory curve. For example, maximum inspiratory flow is denoted FIFmax. Unless otherwise specified, volume qualifiers indicate the volume inspired from RV at the point of measurement.) |
| PEF | Peak expiratory flow: The highest forced expiratory flow measured with a peak flow meter |
| MVV | Maximal voluntary ventilation: volume of air expired in a specified period during repetitive maximal effort |
Tidal volume (symbol VT or TV) is the volume of air moved into or out of the lungs during a normal breath.[1] In a healthy, young human adult, tidal volume is approximately 500 ml per inspiration or 7 ml/kg of body mass.[2]
Mechanical ventilation
Tidal volume plays a significant role during mechanical ventilation to ensure adequate ventilation without causing trauma to the lungs. Tidal volume is measured in milliliters and ventilation volumes are estimated based on a patient's ideal body mass. Measurement of tidal volume can be affected (usually overestimated) by leaks in the breathing circuit or the introduction of additional gas, for example during the introduction of nebulized drugs.
Ventilator-induced lung injury such as Acute lung injury (ALI) /Acute Respiratory Distress Syndrome (ARDS) can be caused by ventilation with very large tidal volumes in normal lungs, as well as ventilation with moderate or small volumes in previously injured lungs, and research shows that the incidence of ALI increases with higher tidal volume settings in nonneurologically-impaired patients. .[3] Similarly A 2018 systematic review by The Cochrane Collaboration provided evidence that low tidal volume ventilation reduced post operative pneumonia and reduced the requirement for both invasive and non invasive ventilation after surgery[4]
Initial settings of mechanical ventilation:
Patients without pre-existing lung disease
Protective lung ventilation strategies should be applied with VT 6ml/kg to 8ml/kg with RR = 12 to 20 and an average starting target minute ventilation of 7 L/min.
Patients with chronic obstructive lung disease
Protective lung volumes apply 6ml/kg to 8ml/kg with a rate high enough for proper alveolar ventilation but does not create or aggravate intrinsic positive end-expiry pressure (peep).
Acute respiratory distress syndrome
Protective lung ventilation strategies apply. VT 6 to 8 ml/kg or as low as 5 ml/kg in severe cases. Permissive hypercapnia can be employed in an attempt to minimize aggressive ventilation leading to lung injury. Higher peeps are often required however not all ARDS patients require the same peep levels. Patient should be started on 6 ml/kg and peep increased till plateau pressure is 30 cm H20 in most severe cases.
References
- ↑ Haddad, Moshe; Sharma, Sandeep (2021), "Physiology, Lung", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 31424761, retrieved 2021-03-17
- ↑ Beardsell, I et al: MCEM Part A:MCQs, page 33, Royal Society of Medicine Press, 2009
- ↑ Gajic, Ognjen; Saqib Dara; Jose Mendez; Abedola Adensanya; Emir Festic; Sean Caples; Rimki Rana; Jennifer StSauver; James Lymp; Bekele Afessa (2004). "Ventilator-associated lung injury in patients without acute lung injury at the onset of mechanical ventilation". Critical Care Medicine. 32 (9): 1817–1824. doi:10.1097/01.CCM.0000133019.52531.30. PMID 15343007. S2CID 6386675.
- ↑ Guay, Joanne; Ochroch, Edward A; Kopp, Sandra (2018-07-09). "Intraoperative use of low volume ventilation to decrease postoperative mortality, mechanical ventilation, lengths of stay and lung injury in adults without acute lung injury". Cochrane Database of Systematic Reviews. 7: CD011151. doi:10.1002/14651858.cd011151.pub3. ISSN 1465-1858. PMC 6513630. PMID 29985541.
External links
- Ricard JD (May 2003). "Are we really reducing tidal volume—and should we?". American Journal of Respiratory and Critical Care Medicine. 167 (10): 1297–8. doi:10.1164/rccm.2303003. PMID 12738592.