Trogocytosis
Trogocytosis (Greek: trogo; gnaw) is when a cell nibbles another cell.[1] It's a process whereby lymphocytes (B, T and NK cells) conjugated to antigen-presenting cells extract surface molecules from these cells and express them on their own surface.[2] The molecular reorganization occurring at the interface between the lymphocyte and the antigen-presenting cell during conjugation is also called "immunological synapse".
Steps in the discovery of trogocytosis
First indication for the existence of this process dates back late 70s when several research groups reported on the presence of unexpected molecules such as Major Histocompatibility complex molecules (MHC) on T cells. The notion that membrane fragments, and not isolated molecules, could be captured by T cells on antigen-presenting cells was suggested by the capture of MHC molecules fused to the green fluorescent protein (GFP) in their intracellular portion.[3] The demonstration that membrane fragments were involved in this transfer process came when fluorescent probes incorporated in the plasma membrane of the antigen-presenting cell as well as non-MHC molecules were found to be captured by T cells together with the antigen.[4][5]
Cell types performing trogocytosis
Trogocytosis has been initially documented in T, B, and NK cells both in vivo and in vitro. On T cells and B cells, trogocytosis is triggered when the T cell receptor (TCR) on T cells or B cell receptor (BCR) on B cells interacts with the antigen recognized on antigen-presenting cells. Like in lymphocytes, trogocytosis occurs with PMN (polymorphonuclear leukocytes, also known as granulocytes) and is associated with effective ADCC (Antibody dependent cell mediated cytotoxicity).
It was shown that in order to initiate ADCC in vitro, PMN's have to adhere to their target cells and form tight junctions with antibody opsonized tumor cells. This cell clustering precedes mutual membrane lipid exchange between effector and target cell during ADCC and does not happen in the absence of opsonizing antibodies.[6] Trogocytosis also occurs in monocytes, and dendritic cells. Outside the immune system, similar transfer of membrane fragments have been documented between sperm and oocytes, a process thought to contribute to gamete fusion.[7]
Lately the term has been attributed to macrophages, such as the CNS resident microglia, which are able to partially remove small portions of neuronal axons during postnatal development.[8]
Mechanisms of trogocytosis
Trogocytosis involves the transfer of plasma membrane fragments from the presenting cell to the lymphocyte. Trogocytosis is specifically triggered by antigen receptor signalling on T and B cells, by killer inhibitory and killer activatory receptor on NK cells and by various receptors on other cells including Fc receptor and scavenger class A receptor. It is likely that trogocytosis does not involve the capture of vesicles such as exosomes secreted by antigen-presenting cells. Rather, molecules could move from antigen-presenting cells to lymphocytes conveyed by membrane nanotubes or membrane fragments could be torn by T cells due to physical forces required for immunological synapse formation and deformation. Depending on the two cell types involved in conjugates, trogocytosis can be unidirectional or bidirectional. Proteins transferred by trogocytosis are many and mostly include proteins inserted in or closely associated to the plasma membrane (proteins spanning the lipid bilayer or inserted in the extracellular or intracellular leaflets). For instance, human lymphocytes were recently shown to acquire the inner-membrane protein H-Ras, a G-protein vital for common lymphocyte functions and a prominent participant in human cancer, from the cells they scan.[9] The transfer was cell contact-dependent and occurred in the context of cell-conjugate formation. Moreover, the acquisition of oncogenic H-RasG12V by NK- and T lymphocytes had important biological functions in the adopting lymphocytes: the transferred H-RasG12V induced ERK phosphorylation, increased interferon-γ and tumor necrosis factor-α secretion, enhanced lymphocyte proliferation, and augmented NK-mediated target cell killing.
Physiological consequences
Trogocytosis can have physiological consequences in two ways: either because "recipient" cells acquire and make use of molecules they do not usually express or because «donor» cells are stripped of molecules, which may alter their interaction with cellular partners. Acquired molecules, such as regulatory molecules with extracellular or intracellular components might alter the lymphocytes activity and direct several lymphocyte functions, such as migration to the adequate injured tissues. Such gained plasma membrane fragments could also contribute to the capacity to proliferate, because lipids are highly energetic claiming components to establish. Trogocytosis might have appeared first in very primitive organisms to feed off other cells. Most of the biological functions identified for trogocytosis have been reported for lymphocytes and dendritic cells. Major findings along these lines are:
- cytotoxic T lymphocytes having captured antigenic peptide-MHC complexes can be killed by CTL specific for this antigen (a process termed fratricide)
- helper T lymphocyte having captured antigenic peptide-MHC complexes are involved in a negative regulatory feed-back loop leading to their inactivation[10]
- dendritic cells stripped of antigenic peptide-MHC complexes by T cells through trogocytosis contribute to affinity maturation of T cell response by selecting high-affinity T cell[11]
- down-modulation of costimulatory molecules on dendritic cells mediated by T cells leads to regulation of T cell response[12]
- transfer of antigen between dendritic cells by trogocytosis favours reactivation of memory T cells at the expenses of naive T cells[13]
- transfer of antigen between dendritic cells by trogocytosis contributes to allograft rejection[14]
Implications of trogocytosis in serotherapeutic approaches
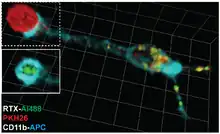
Therapeutic antibodies can be used to treat cancer. An example is rituximab, a therapeutic antibody used to treat chronic lymphocytic leukemia, recognizes the CD20 molecule expressed by tumor cells and leads to their elimination.[15] However, using too much of the antibody results in part from the removal of rituximab-CD20 complexes from the tumor cell surface by monocytes through trogocytosis. This effect leads to tumors cell escape by antigenic modulation. Reducing the dose of therapeutic antibodies to limit the extent of trogocytosis might improve their therapeutic efficacy.[16]
Epratuzumab (a CD22 Mab) acts using trogocytosis to transfer CD22 and other B-cell proteins from B cells to effector cells.[17]
Trogocytosis-based assays as immunomonitoring tools
TRAP assays (TRogocytosis Analysis Protocol) allow to identify, characterize and purify T and B cells recognizing their specific antigen based on their ability to extract molecules (in that case, fluorescent probes) from the plasma membrane of antigen-presenting cells.[18] These assays require equipment such as a flow cytometer but are otherwise very cheap, easy to perform, fast (can be performed within 3 hours) and applicable to any population of T or B cells. TRAP assays have been successfully used to detect T cell responses against viral infections,[19] cancer,[20] autoimmune diseases[21] and vaccines.[22]
See also
The process of Trogocytosis is considered different from but similar to the unrelated processes known as Phagocytosis and Paracytophagy.
References
- ↑ Dance, Amber (2019). "Core Concept: Cells nibble one another via the under-appreciated process of trogocytosis". Proceedings of the National Academy of Sciences. 116 (36): 17608–17610. doi:10.1073/pnas.1912252116. PMC 6731757. PMID 31481628.
- ↑ Joly, Etienne; Hudrisier, Denis (September 2003). "What is trogocytosis and what is its purpose?". Nature Immunology. 4 (9): 815. doi:10.1038/ni0903-815. PMID 12942076.
- ↑ Huang, J.; Yang, Y; Sepulveda, H; Shi, W; Hwang, I; Peterson, PA; Jackson, MR; Sprent, J; Cai, Z (29 October 1999). "TCR-Mediated Internalization of Peptide-MHC Complexes Acquired by T Cells". Science. 286 (5441): 952–954. doi:10.1126/science.286.5441.952. PMID 10542149.
- ↑ Patel, Dhaval M.; Arnold, Paula Y.; White, Gregory A.; Nardella, John P.; Mannie, Mark D. (15 November 1999). "Class II MHC/Peptide Complexes Are Released from APC and Are Acquired by T Cell Responders During Specific Antigen Recognition". The Journal of Immunology. 163 (10): 5201–5210. PMID 10553040.
- ↑ Hudrisier, Denis; Riond, Joelle; Mazarguil, Honoré; Gairin, Jean Edouard; Joly, Etienne (15 March 2001). "Cutting Edge: CTLs Rapidly Capture Membrane Fragments from Target Cells in a TCR Signaling-Dependent Manner". The Journal of Immunology. 166 (6): 3645–3649. doi:10.4049/jimmunol.166.6.3645. PMID 11238601.
- ↑ Horner, Heike; Frank, Carola; Dechant, Claudia; Repp, Roland; Glennie, Martin; Herrmann, Martin; Stockmeyer, Bernhard (1 July 2007). "Intimate Cell Conjugate Formation and Exchange of Membrane Lipids Precede Apoptosis Induction in Target Cells during Antibody-Dependent, Granulocyte-Mediated Cytotoxicity". The Journal of Immunology. 179 (1): 337–345. doi:10.4049/jimmunol.179.1.337. PMID 17579054.
- ↑ Barraud‐Lange, Virginie; Naud‐Barriant, Nathalie; Bomsel, Morgane; Wolf, Jean‐Philippe; Ziyyat, Ahmed (15 June 2007). "Transfer of oocyte membrane fragments to fertilizing spermatozoa". The FASEB Journal. 21 (13): 3446–3449. doi:10.1096/fj.06-8035hyp. PMID 17575263. S2CID 35630271.
- ↑ Weinhard, Laetitia; di Bartolomei, Giulia; Bolasco, Giulia; Machado, Pedro; Schieber, Nicole L.; Neniskyte, Urte; Exiga, Melanie; Vadisiute, Auguste; Raggioli, Angelo; Schertel, Andreas; Schwab, Yannick; Gross, Cornelius T. (26 March 2018). "Microglia remodel synapses by presynaptic trogocytosis and spine head filopodia induction". Nature Communications. 9 (1): 1228. Bibcode:2018NatCo...9.1228W. doi:10.1038/s41467-018-03566-5. PMC 5964317. PMID 29581545.
- ↑ Rechavi, Oded; Goldstein, Itamar; Vernitsky, Helly; Rotblat, Barak; Kloog, Yoel; Kanellopoulos, Jean (21 November 2007). "Intercellular Transfer of Oncogenic H-Ras at the Immunological Synapse". PLOS ONE. 2 (11): e1204. Bibcode:2007PLoSO...2.1204R. doi:10.1371/journal.pone.0001204. PMC 2065899. PMID 18030338.
- ↑ Helft, Julie; Jacquet, Alexandra; Joncker, Nathalie T.; Grandjean, Isabelle; Dorothée, Guillaume; Kissenpfennig, Adrien; Malissen, Bernard; Matzinger, Polly; Lantz, Olivier (15 August 2008). "Antigen-specific T-T interactions regulate CD4 T-cell expansion". Blood. 112 (4): 1249–1258. doi:10.1182/blood-2007-09-114389. PMC 2515122. PMID 18539897.
- ↑ Kedl, Ross M.; Schaefer, Brian C.; Kappler, John W.; Marrack, Philippa (3 December 2001). "T cells down-modulate peptide-MHC complexes on APCs in vivo". Nature Immunology. 3 (1): 27–32. doi:10.1038/ni742. PMID 11731800. S2CID 20735730.
- ↑ Qureshi, Omar S.; Zheng, Yong; Nakamura, Kyoko; Attridge, Kesley; Manzotti, Claire; Schmidt, Emily M.; Baker, Jennifer; Jeffery, Louisa E.; Kaur, Satdip; Briggs, Zoe; Hou, Tie Z.; Futter, Clare E.; Anderson, Graham; Walker, Lucy S.K.; Sansom, David M. (29 April 2011). "Trans-endocytosis of CD80 and CD86: a molecular basis for the cell extrinsic function of CTLA-4". Science. 332 (6029): 600–603. Bibcode:2011Sci...332..600Q. doi:10.1126/science.1202947. PMC 3198051. PMID 21474713.
- ↑ Wakim, Linda M.; Bevan, Michael J. (31 March 2011). "Cross-dressed dendritic cells drive memory CD8+ T-cell activation after viral infection". Nature. 471 (7340): 629–632. Bibcode:2011Natur.471..629W. doi:10.1038/nature09863. PMC 3423191. PMID 21455179.
- ↑ Herrera, Osquel Barroso; Golshayan, Dela; Tibbott, Rebecca; Ochoa, Francisco Salcido; James, Martha J.; Marelli-Berg, Federica M.; Lechler, Robert I. (15 October 2004). "A Novel Pathway of Alloantigen Presentation by Dendritic Cells". The Journal of Immunology. 173 (8): 4828–4837. doi:10.4049/jimmunol.173.8.4828. PMID 15470023.
- ↑ Beum, Paul V.; Kennedy, Adam D.; Williams, Michael E.; Lindorfer, Margaret A.; Taylor, Ronald P. (15 February 2006). "The Shaving Reaction: Rituximab/CD20 Complexes Are Removed from Mantle Cell Lymphoma and Chronic Lymphocytic Leukemia Cells by THP-1 Monocytes". The Journal of Immunology. 176 (4): 2600–2609. doi:10.4049/jimmunol.176.4.2600. PMID 16456022.
- ↑ Williams, Michael E.; Densmore, John J.; Pawluczkowycz, Andrew W.; Beum, Paul V.; Kennedy, Adam D.; Lindorfer, Margaret A.; Hamil, Susan H.; Eggleton, Jane C.; Taylor, Ronald P. (15 November 2006). "Thrice-Weekly Low-Dose Rituximab Decreases CD20 Loss via Shaving and Promotes Enhanced Targeting in Chronic Lymphocytic Leukemia". The Journal of Immunology. 177 (10): 7435–7443. doi:10.4049/jimmunol.177.10.7435. PMID 17082663.
- ↑ "Epratuzumab". Immunomedics.
- ↑ Daubeuf, Sandrine; Puaux, Anne-Laure; Joly, Etienne; Hudrisier, Denis (29 December 2006). "A simple trogocytosis-based method to detect, quantify, characterize and purify antigen-specific live lymphocytes by flow cytometry, via their capture of membrane fragments from antigen-presenting cells". Nature Protocols. 1 (6): 2536–2542. doi:10.1038/nprot.2006.400. PMID 17406507. S2CID 25090649.
- ↑ Beadling, Carol; Slifka, Mark K (1 October 2006). "Quantifying viable virus-specific T cells without a priori knowledge of fine epitope specificity". Nature Medicine. 12 (10): 1208–1212. doi:10.1038/nm1413. PMID 17013384. S2CID 9102979.
- ↑ Machlenkin, Arthur; Uzana, Ronny; Frankenburg, Shoshana; Eisenberg, Galit; Eisenbach, Lea; Pitcovski, Jacob; Gorodetsky, Raphael; Nissan, Aviram; Peretz, Tamar; Lotem, Michal (15 March 2008). "Capture of Tumor Cell Membranes by Trogocytosis Facilitates Detection and Isolation of Tumor-Specific Functional CTLs". Cancer Research. 68 (6): 2006–2013. doi:10.1158/0008-5472.CAN-07-3119. PMID 18339883.
- ↑ Bahbouhi, Bouchaib; Pettré, Ségolène; Berthelot, Laureline; Garcia, Alexandra; Elong Ngono, Annie; Degauque, Nicolas; Michel, Laure; Wiertlewski, Sandrine; Lefrère, Fabienne; Meyniel, Claire; Delcroix, Catherine; Brouard, Sophie; Laplaud, David-Axel; Soulillou, Jean-Paul (June 2010). "T cell recognition of self-antigen presenting cells by protein transfer assay reveals a high frequency of anti-myelin T cells in multiple sclerosis". Brain. 133 (6): 1622–1636. doi:10.1093/brain/awq074. PMID 20435630.
- ↑ Daubeuf, Sandrine; Préville, Xavier; Momot, Marie; Misseri, Yolande; Joly, Etienne; Hudrisier, Denis (September 2009). "Improving administration regimens of CyaA-based vaccines using TRAP assays to detect antigen-specific CD8+ T cells directly ex vivo". Vaccine. 27 (41): 5565–5573. doi:10.1016/j.vaccine.2009.07.035. PMID 19647811.