Uterus didelphys
| Uterus didelphys | |
|---|---|
| Other names | Bicervical bicornuate uterus |
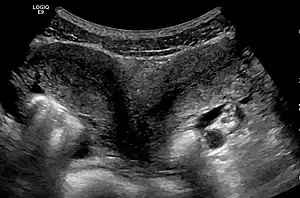 | |
| Ultrasound showing didelphys | |
| Specialty | Gynaecology |
Uterus didelphys (sometimes also uterus didelphis) represents a uterine malformation where the uterus is present as a paired organ when the embryogenetic fusion of the Müllerian ducts fails to occur. As a result, there is a double uterus with two separate cervices, and possibly a double vagina as well. Each uterus has a single horn linked to the ipsilateral fallopian tube that faces its ovary.
Most non-human mammals do not have a single uterus with no separation of horns. Marsupials and rodents have a double uterus (uterus duplex). In other animals (e.g. nematodes), the term 'didelphic' refers to a double genital tract, as opposed to monodelphic, with a single tract.
Signs and symptoms
Persons with the condition may be asymptomatic and unaware of having a double uterus. However, a study by Heinonen showed that certain conditions are more common. In his study of 26 women with a double uterus gynecological complaints included dysmenorrhea and dyspareunia. All patients displayed a double vagina. The fetal survival rate in 18 patients who delivered was 67.5%. Premature delivery occurred in 21% of the pregnancies. Breech presentation occurred in 43% of women and cesarean section was performed in 82% of the cases.[1]
Cause

The uterus is formed during embryogenesis by the fusion of the two paramesonephric ducts (also called Müllerian ducts). This process usually fuses the two Müllerian ducts into a single uterine body but fails to take place in these affected women who maintain their double Müllerian systems. A didelphic uterus will have a double cervix and is usually associated with a double vagina. The cause of the fusion failure is not known. Associated defects may affect the vagina, the renal system and, less commonly, the skeleton.
The condition is less common than these other uterine malformations: arcuate uterus, septate uterus, and bicornuate uterus. It has been estimated to occur in 1/3,000 women.[2]
Syndrome
A specific association of uterus didelphys (double uterus), unilateral hematocolpos (inadequate draining of menstrual blood) and ipsilateral renal agenesis (having only one kidney) has been described.[3]
Diagnosis
A pelvic examination will typically reveal a double vagina and a double cervix. Investigations are usually prompted on the basis of such findings as well as when reproductive problems are encountered. Not all cases of uterus didelphys involve duplication of the cervix and vagina.
Helpful techniques to investigate the uterine structure are transvaginal ultrasonography and sonohysterography, hysterosalpingography, MRI, and hysteroscopy. More recently 3-D ultrasonography has been advocated as an excellent non-invasive method to evaluate uterine malformations.[4]
Uterus didelphys is often confused with a complete uterine septum. Often more than one method of investigation is necessary to accurately diagnose the condition. Correct diagnosis is crucial as treatment for these two conditions are very different.[5] Whereas most doctors recommend removal of a uterine septum, they generally concur that it is better not to operate on a uterus didelphys. In either case, a highly qualified reproductive endocrinologist should be consulted.
Management
Patients with a double uterus may need special attention during pregnancy as premature birth and malpresentation are common. Cesarean section was performed in 82% of patients reported by Heinonen.[1]
Uterus didelphys, in certain studies, has also been found associated with higher rate of infertility, miscarriage, intrauterine growth retardation, and postpartum bleed.[5]
Epidemiology
In the United States, uterus didelphys is reported to occur in 0.1–0.5% of women. It is difficult to know the exact occurrence of this anomaly, as it may go undetected in the absence of medical and reproductive complications.
Multiple pregnancy
A number of twin gestations have occurred where each uterus carried its pregnancy separately. There have only been about 100 cases worldwide of a woman with a double uterus being pregnant in both wombs at the same time.[6] Prior to 2005 only 11 cases had been reported worldwide.[7]
Maricia Tescu of Iasi, Romania, gave birth to a premature son in 11 December 2004. Her second baby boy, was born via C-section at full term 59 days later, in early February 2005.[8][9]
In February 26, 2009, Sarah Reinfelder of Sault Ste. Marie, Michigan delivered two healthy, although seven weeks premature, infants by cesarean section at Marquette General Hospital.[10] It is possible that the deliveries occur at different times, thus the delivery interval could be days or even weeks. In September 15, 2011, Andreea Barbosa of St. Petersburg, Florida gave birth to fraternal twins, a boy and a girl, via C-section.[11] In October 23, 2020, Kelly Fairhurst of Essex, England delivered twins, a boy and a girl, at 35 weeks via a planned C-section.[12]
Triplets
A UK woman with a double uterus gave birth to triplets in 2006. Hannah Kersey, of Northam, Devon, gave birth to a pair of identical twin girls from an egg that implanted into one womb and then divided, and to an female infant from a single egg that implanted into the other womb. This was the first known birth of viable triplets in a woman with a double uterus.[13] A triplet pregnancy in a woman with uterus didelphys was reported from Israel in 1981; one baby died in utero, and of the remaining babies, one was delivered at 27 weeks gestation and the other 72 days later.[14] In 2019, Arifa Sultana of Bangladesh gave premature birth in February and then via emergency Ceasarean section to twins, 26 days later.[15][16]
See also
References
- 1 2 Heinonen, P.K. (1984). "Uterus didelphys: a report of 26 cases". European Journal of Obstetrics & Gynecology and Reproductive Biology. 17 (5): 345–50. doi:10.1016/0028-2243(84)90113-8. PMID 6479426.
- ↑ Grimbizis, G. F.; Camus, M; Tarlatzis, BC; Bontis, JN; Devroey, P (2001). "Clinical implications of uterine malformations and hysteroscopic treatment results". Human Reproduction Update. 7 (2): 161–74. doi:10.1093/humupd/7.2.161. PMID 11284660.
- ↑ Madureira, A. J.; Mariz, C. M.; Bernardes, J. C.; Ramos, I. M. (2006). "Case 94: Uterus Didelphys with Obstructing Hemivaginal Septum and Ipsilateral Renal Agenesis". Radiology. 239 (2): 602–6. doi:10.1148/radiol.2392031187. PMID 16641359.
- ↑ Woelfer, B; Salim, R; Banerjee, S; Elson, J; Regan, L; Jurkovic, D (2001). "Reproductive outcomes in women with congenital uterine anomalies detected by three-dimensional ultrasound screening". Obstetrics & Gynecology. 98 (6): 1099–103. doi:10.1016/S0029-7844(01)01599-X. PMID 11755560. S2CID 37650526.
- 1 2 Pui, M (2004). "Imaging diagnosis of congenital uterine malformation". Computerized Medical Imaging and Graphics. 28 (7): 425–33. doi:10.1016/j.compmedimag.2004.05.008. PMID 15464882.
- ↑ "American Woman With Double Uterus Expecting Two Babies Who Are Not Twins". www.medicalnewstoday.com. 2010-07-20. Retrieved 2021-12-06.
- ↑ "Twins are born two months apart". 2005-02-09. Retrieved 2021-12-06.
- ↑ "Twins are born two months apart". 2005-02-09. Retrieved 2021-12-06.
- ↑ "Pregnant While Pregnant: 12 Women Who Went Through It (And 2 Ways It Can Happen)". BabyGaga. 2018-12-16. Retrieved 2021-12-06.
- ↑ "Mich. woman with 2 wombs delivers twin daughters". Associated Press. February 28, 2009. Retrieved 2018-12-28.
- ↑ "Mom with two uteruses has twins: What causes rare condition?". www.cbsnews.com. Retrieved 2021-12-06.
- ↑ Fairhurst, Kelly (2021-04-02). "Experience: I carried a twin in each of my wombs". the Guardian. Retrieved 2021-12-06.
- ↑ "Triplets for woman with two wombs". BBC News. December 21, 2006. Retrieved 2007-06-27.
- ↑ Mashiach, S; Ben-Rafael, Z; Dor, J; Serr, DM (1981). "Triplet pregnancy in uterus didelphys with delivery interval of 72 days". Obstetrics and Gynecology. 58 (4): 519–21. PMID 7279347.
- ↑ "Bangladesh woman with two wombs has twins one month after first birth". BBC News. 2019-03-28. Retrieved 2021-12-06.
- ↑ "Woman with two wombs gives birth twice, less than a month apart". CBS. March 29, 2019. Retrieved 2018-04-16.