Vaginal delivery

A vaginal delivery is the birth of offspring in mammals (babies in humans) through the vagina (also called the "birth canal").[1] It is the most common method of childbirth worldwide.[2] It is considered the preferred method of delivery, with lower morbidity and mortality than Caesarean sections (C-sections).[3]
Epidemiology
United States
70% of births in the United States in 2019 were vaginal deliveries.[4]
Global
80% of births globally in 2021 were vaginal deliveries, with rates varying from 95% in sub-Saharan Africa to 45% in the Caribbean.[2]
Benefits of vaginal delivery
Mother
Benefits for the mother include
- Avoiding surgery and resulting quicker recovery time and shorter hospital admission[5]
- Quicker onset of lactation[6]
- Decreased complications in future pregnancies, including placenta previa[7]
Infant
Benefits for the infant include:
- Decreased infant respiratory conditions, including infant respiratory distress syndrome, transient tachypnea of the newborn, and respiratory-related NICU admissions[5]
- Improved immune function, possibly due to the infant's exposure to normal vaginal and gut bacteria during vaginal birth[8]
Types of vaginal delivery
Different types of vaginal deliveries have different terms:
- A spontaneous vaginal delivery (SVD) occurs when a pregnant woman goes into labor without the use of drugs or techniques to induce labor and delivers their baby without forceps, vacuum extraction, or a cesarean section.[1]
- An induced vaginal delivery is a delivery involving labor induction, where drugs or manual techniques are used to initiate labor.[9] Vaginal delivery can be either spontaneous or induced.
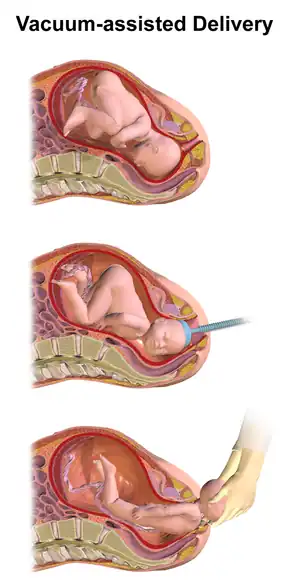
- An assisted vaginal delivery (AVD) or instrumental vaginal delivery occurs when a pregnant woman requires the use of special instruments such as forceps or a vacuum extractor to deliver her baby vaginally.[10] Both spontaneous and induced vaginal delivery can be assisted. Examples of instruments to assist delivery include obstretical forcepts and vacuum extraction with a vacuum cup device.[10]
A normal vaginal delivery (NVD) is defined as any vaginal delivery, assisted or unassisted.[11]
Stages of labor
Labor is characterized by uterine contractions which push the fetus through the birth canal and results in delivery.[12] Labor is divided into three stages.
- First stage of labor starts with the onset of contractions and finishes when the cervix is fully dilated at 10 cm.[13] This stage can further be divided into latent and active labor. The latent phase is defined by cervical dilation of 0 to 6 cm. The active phase is defined by cervical dilation of 6 cm to 10 cm.
- Second stage of labor starts when the cervix is dilated to 10 cm and finishes with the birth of the fetus. This is stage is characterized by strong contractions and active pushing by the mother. It can last from 20 minutes to 2 hours.[14]
- Third stage of labor starts after the birth of the fetus and is finished when the placenta is delivered.[13] It can last from 5 to 30 minutes.
Risks and complications of vaginal delivery
Complications of vaginal delivery can be grouped into the following criteria; failure to progress, abnormal fetal heart rate tracing, intrapartum hemorrhage, and post-partum hemorrhage.
Failure to progress occurs when the labor process slows or stops entirely, indicated by slowed cervical dilation.[3] Factors that place a woman's pregnancy at higher risk include advanced maternal age, Premature Rupture of Membranes (PROM) and induction of labor.[15] Oxytocin, a uterotonic agent, can be administered to augment labor. Cesarean section is also commonly considered when the pregnancy fails to progress.
Abnormal fetal heart tracing suggests that the fetus' heart rate has slowed during labor due to head compression, cord compression, hypoxemia or anemia.[3] This issue is often resolved by discontinuing labor augmenting agents such as oxytocin. If the abnormal fetal heart rate persists, a cesarean section is indicated.
Intrapartum hemorrhage is characterized by the presence of copious blood during labor. The bleeding may be due to placental abruption, uterine rupture, placenta accrete, undiagnosed placenta previa, or vasa previa.[3] Cesarean section is indicated.
Post-partum hemorrhage is defined by the loss of at least 1,000 mL of blood accompanied with symptoms of hypovolemia within 24 hours after delivery. Typically, the first symptom is excessive bleeding accompanied by tachycardia. Significant loss of blood may also result in hypotension, nausea, dyspnea, and chest pain.[16] It is estimated that between 3% to 5% of women giving birth vaginally will experience post-partum hemorrhage. Risk factors include fetal macrosomia, pre-eclampsia, and prolonged labor.[16] Prevention consists of administering oxytocin (Pitocin) at delivery and early umbilical cord clamping.[17] Post-partum hemorrhage is usually attributed to uterus atony, when the uterus fails to contract after delivering the baby.[18]
Contraindications to vaginal delivery
Spontaneous vaginal delivery at term is the preferred outcome of pregnancy, and according to the International Federation of Gynecology and Obstetrics, will be recommended if there are no evidence-based clinical indications for cesarean section.[19] However, there are some contraindications for vaginal delivery that would result in conversion to cesarean delivery. The decision to switch to cesarean delivery is made by the health care provider and mother, and is sometimes delayed until the mother is in labor.
Breech birth presentations occur when the fetus' buttocks or lower extremities are poised to deliver before the fetus' upper extremities or head. The three types of breech positions are footling breech, frank breech, and complete breech. Breech positions can result in conversion from vaginal to cesarean delivery because it is more difficult for the baby to deliver through the birth canal, there is a risk for cord prolapse, and there is a slightly elevated risk for birth defects of breech babies.
Complete placenta previa occurs when the placenta covers the opening of the cervix. If placenta previa is present at the time of delivery, vaginal delivery is contraindicated because the placenta is blocking the fetus’ passageway to the vaginal canal.
Herpes simplex virus with active genital lesions or prodromal symptoms is a contraindication for vaginal delivery so as to avoid mother-fetal transfer of HSV lesions.
Untreated human immunodeficiency virus (HIV) infection is a contraindication for vaginal delivery to avoid mother-fetal transfer of human immunodeficiency virus. [20]
See also
References
- 1 2 Patterson DA, Winslow M, Matus CD (August 2008). "Spontaneous vaginal delivery". American Family Physician. 78 (3): 336–41. PMID 18711948.
- 1 2 "Caesarean section rates continue to rise, amid growing inequalities in access: WHO". www.who.int. Retrieved 2021-08-30.
- 1 2 3 4 Desai NM, Tsukerman A (2021). "Vaginal Delivery". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 32644623. Retrieved 2021-08-30.
- ↑ "FastStats". www.cdc.gov. 2021-03-24. Retrieved 2021-08-30.
- 1 2 Gregory KD, Jackson S, Korst L, Fridman M (January 2012). "Cesarean versus vaginal delivery: whose risks? Whose benefits?". American Journal of Perinatology. 29 (1): 7–18. doi:10.1055/s-0031-1285829. PMID 21833896.
- ↑ Chapman DJ, Pérez-Escamilla R (April 1999). "Identification of risk factors for delayed onset of lactation". Journal of the American Dietetic Association. 99 (4): 450–4, quiz 455-6. doi:10.1016/s0002-8223(99)00109-1. PMID 10207398.
- ↑ Gurol-Urganci I, Cromwell DA, Edozien LC, Smith GC, Onwere C, Mahmood TA, et al. (November 2011). "Risk of placenta previa in second birth after first birth cesarean section: a population-based study and meta-analysis". BMC Pregnancy and Childbirth. 11 (1): 95. doi:10.1186/1471-2393-11-95. PMC 3247856. PMID 22103697.
- ↑ Neu J, Rushing J (June 2011). "Cesarean versus vaginal delivery: long-term infant outcomes and the hygiene hypothesis". Clinics in Perinatology. 38 (2): 321–31. doi:10.1016/j.clp.2011.03.008. PMC 3110651. PMID 21645799.
- ↑ Gunay T, Turgut A, Demircivi Bor E, Hocaoglu M (May 2020). "Comparison of maternal and fetal complications in pregnant women with breech presentation undergoing spontaneous or induced vaginal delivery, or cesarean delivery". Taiwanese Journal of Obstetrics & Gynecology. 59 (3): 392–397. doi:10.1016/j.tjog.2020.03.010. PMID 32416886.
- 1 2 Verma, Ganga L.; Spalding, Jessica J.; Wilkinson, Marc D.; Hofmeyr, G. Justus; Vannevel, Valerie; O'Mahony, Fidelma (2021-09-24). "Instruments for assisted vaginal birth". The Cochrane Database of Systematic Reviews. 2021 (9): CD005455. doi:10.1002/14651858.CD005455.pub3. ISSN 1469-493X. PMC 8462579. PMID 34559884.
- ↑ Omona, Kizito (2021-11-03), Ray, Amita (ed.), "Vaginal Delivery", Empowering Midwives and Obstetric Nurses, IntechOpen, doi:10.5772/intechopen.96097, ISBN 978-1-83969-065-5, S2CID 241148030, retrieved 2021-12-06
- ↑ "Labor". www.hopkinsmedicine.org. Retrieved 2021-09-13.
- 1 2 Hutchison, Julia; Mahdy, Heba; Hutchison, Justin (2021), "Stages of Labor", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 31335010, retrieved 2021-09-13
- ↑ "Labor and Birth". Office on Womens Health. September 13, 2021. Retrieved September 13, 2021.
{{cite web}}: CS1 maint: url-status (link) - ↑ Sheiner E, Levy A, Feinstein U, Hallak M, Mazor M (March 2002). "Risk factors and outcome of failure to progress during the first stage of labor: a population-based study". Acta Obstetricia et Gynecologica Scandinavica. 81 (3): 222–6. PMID 11966478.
- 1 2 Evensen, Ann; Anderson, Janice M.; Fontaine, Patricia (2017-04-01). "Postpartum Hemorrhage: Prevention and Treatment". American Family Physician. 95 (7): 442–449. ISSN 0002-838X. PMID 28409600.
- ↑ "How is postpartum hemorrhage prevented?". www.medscape.com. Retrieved 2021-09-13.
- ↑ Ray, C. Le; Fraser, W.; Rozenberg, P.; Langer, B.; Subtil, D.; Goffinet, F. (2011-10-01). "Duration of passive and active phases of the second stage of labour and risk of severe postpartum haemorrhage in low-risk nulliparous women". European Journal of Obstetrics and Gynecology and Reproductive Biology. 158 (2): 167–172. doi:10.1016/j.ejogrb.2011.04.035. ISSN 0301-2115. PMID 21640464.
- ↑ International Federation Gynecology and Obstetrics. "FIGO Ethics and Professionalism Guideline: Decision Making about Vaginal and Caesarean Delivery" (PDF).
{{cite journal}}: Cite journal requires|journal=(help)CS1 maint: uses authors parameter (link) - ↑ Patterson D, Winslow M, Matus C (August 2008). "Spontaneous Vaginal Delivery". American Family Physician. 78 (3): 336–341. PMID 18711948.