Labyrinthitis
| Labyrinthitis | |
|---|---|
| Other names: Otitis interna, vestibular neuronitis, vestibular neuritis, acute labyrinthitis[1] | |
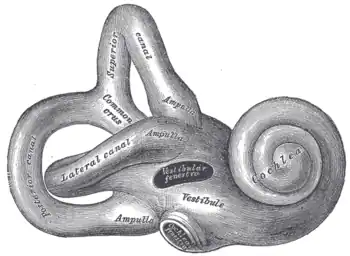 | |
| Diagram of the inner ear | |
| Specialty | Otorhinolaryngology |
| Symptoms | Vertigo, vomiting, ringing in the ears[2] |
| Usual onset | Sudden[2] |
| Duration | Few weeks[3] |
| Risk factors | Viral infection[2] |
| Diagnostic method | Based on symptom[3] |
| Differential diagnosis | Benign positional vertigo, Meniere's, stroke, head injury, cholesteatoma, tumor, multiple sclerosis[1][3] |
| Treatment | Vestibular rehabilitation[2] |
| Medication | Dimenhydrinate, methylprednisolone[3] |
| Prognosis | Usually good[3] |
| Frequency | 35 cases per million per year[3] |
Labyrinthitis, also known as vestibular neuritis, is a type of dysfunction of the inner ear.[1] Symptoms may include feeling like the world is spinning, vomiting, and ringing in the ears.[2] The feeling of world spinning is usually constant; while the presence of hearing loss is variable.[3][1] Onset is generally sudden.[2] While symptoms may improve after a few days; they may require six weeks or longer to resolve fully.[2]
The cause is believed to be due to a viral infection, such as that associated with the common cold.[2] While labyrinthitis involves inflammation of the labyrinth of the inner ear and vestibular neuritis the vestibular nerve in the inner ear; both result in similar symptoms and the terms are generally used interchangeably.[2][1] Diagnosis is based on symptoms.[3] It is a type of peripheral vestibular disorder (balance disorder).[4]
Treatment may involve the use of antihistamines, such as dimenhydrinate, for a few days.[2][3] Vestibular rehabilitation therapy has been shown to be useful.[2][5] Steroids, such as methylprednisolone, may improve recovery if used within three days of onset.[3][5] Antiviral medication have not bee found to be useful.[3] While most people recover fully, some older people may have ongoing dizziness that lasts months.[1] Recurrent episodes are uncommon.[3]
About 3 to 4 per 100,000 people are affected per year.[3] It may occur at any age; though those 30 to 60 years old are most common affected.[1][3] The condition was first described in the medical literature in 1909 by Ruttin.[3]
Signs and symptoms
The main symptoms of labyrinthitis are severe vertigo and nystagmus. The most common symptom for vestibular neuritis is the onset of vertigo that has formed from an ongoing infection or trauma.[6] The dizziness sensation that is associated with vertigo is thought to be from the inner ear labyrinth.[7] Rapid and undesired eye motion (nystagmus) often results from the improper indication of rotational motion. Nausea, anxiety, and a general ill feeling are common due to the distorted balance signals that the brain receives from the inner ear system.[8] Other common symptoms include tinnitus, ear ache, and a feeling of fullness in the ear.[9][10]
Causes
Some people will report having an upper respiratory infection (common cold) or flu prior to the onset of the symptoms of vestibular neuritis; others will have no viral symptoms prior to the vertigo attack. Especially in children, vestibular neuritis may be preceded by symptoms of a common cold. However, the causative mechanism remains uncertain.[11]
Some cases of vestibular neuritis are thought to be caused by an infection of the vestibular ganglion by the herpes simplex type 1 virus.[12] However, the cause of this condition is not fully understood, and in fact, many different viruses may be capable of infecting the vestibular nerve.
Acute localized ischemia of these structures also may be an important cause. This can also be brought on by pressure changes such as those experienced while flying or scuba diving.[13][14][15]
Mechanism
In the vestibular system, there are three canals that are semicircular in shape that input sensory clues.[16] These canals allow the brain to sense rotational motion and linear motion changes.[17] The brain then uses the sensory input clues and the visual input clues from the vestibular system to retain balance. The vestibulo–ocular reflex retains continuous visual focus during motion which is also the vestibular systems job during activity.[17]
Diagnosis
In terms of the diagnosis of this condition we find that the following is done:[18]
- Based on symptoms after ruling out other possible causes
- Abnormal head impulse test
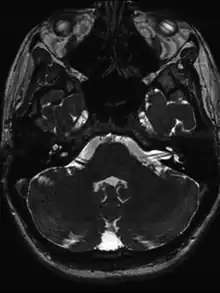
- MRI
Treatment
The treatment for vestibular neuritis depends on the cause. However, symptoms of vertigo can be treated in the same way as other vestibular dysfunctions with vestibular rehabilitation.[19]
Physical therapy
Typical treatments include combinations of head and eye movements, postural changes, and walking exercises. Specifically, exercises that may be prescribed include keeping eyes fixated on a specific target while moving the head, moving the head right to left at two targets at a significant distance apart, walking while keeping eyes fixated on a specific target, and walking while keeping eyes fixated on a specific target while also turning the head in different directions.[20] The main function behind repeating a combination of head and eye movements, postural changes and walking is that through this repetition, compensatory changes for the dysfunctions arising from peripheral vestibular structures may be promoted in the central vestibular system (brainstem and cerebellum).[20]
Vestibular rehabilitation therapy is a highly effective way to substantially reduce or eliminate residual dizziness from labyrinthitis.[21] VRT works by causing the brain to use already existing neural mechanisms for adaptation, neuroplasticity, and compensation.[19] Vestibular neuritis rehabilitation is an effective and safe management to improve symptoms.[22] The vestibular neuritis rehabilitation can improve symptoms or resolve the symptoms which is dependent on each individual. [22]
Rehabilitation strategies most commonly used are:[19]
- Gaze stability exercises – moving the head from side to side while fixated on a stationary object (aimed at assisting the eye to fixate during head rotation without the input from the lost canal vestibulo–ocular reflex). An advanced progression of this exercise would be walking in a straight line while looking side to side by turning the head.
- Habituation exercises – movements designed to provoke symptoms and subsequently reduce the negative vestibular response upon repetition. Examples of these include Brandt–Daroff exercises.
- Functional retraining – including postural control, relaxation, and balance training.
These exercises function by challenging the vestibular system. Progression occurs by increasing the amplitude of the head or focal point movements, increasing the speed of movement, and combining movements such as walking and head turning.[23]
One study found that patients who believed their illness was out of their control showed the slowest progression to full recovery, long after the initial vestibular injury had healed.[24] The study revealed that the patient who compensated well was one who, at the psychological level, was not afraid of the symptoms and had some positive control over them. Notably, a reduction in negative beliefs over time was greater in those patients treated with rehabilitation than in those untreated. "Of utmost importance, baseline beliefs were the only significant predictor of change in a handicap at 6 months follow-up."
Medication
Vestibular neuritis is generally a self-limiting disease. Treatment with drugs is neither necessary nor possible. The effect of glucocorticoids has been studied, but they have not been found to significantly affect long-term outcome.[25]
Symptomatic treatment with antihistaminics such as cinnarizine, however, can be used to suppress the symptoms of vestibular neuritis while it spontaneously regresses.[26] Prochlorperazine is another commonly prescribed medication to help alleviate the symptoms of vertigo and nausea.
Mental disorders
Because mood disorders can hamper recovery from labyrinthitis, treatment may also include any co-occurring anxiety disorder or depression. Severe anxiety episodes are usually addressed by short-term benzodiazepine therapy.[27]
Prognosis
Recovery from acute labyrinthine inflammation generally takes from one to six weeks, but it is not uncommon for residual symptoms such as dysequilibrium and dizziness to last for a couple of months.[24]
Recovery from a temporary damaged inner ear typically follows two phases:
- An acute period, which may include severe vertigo and vomiting
- approximately two weeks of sub-acute symptoms and rapid recovery
Epidemiology
Labyrinthitis affects approximately 35 million people per year (approximately 3.5 cases per 100,000 people).[28] It typically occurs in those between 30 and 60 years of age,[28] and there are no significant differences between male and female incidence rates.[28] In 95% of cases, sufferers experience a single attack and fully recover.[29] Vestibular rehabilitation showed a statistically significant increase in controlling symptoms over no intervention in people who have vestibular neuritis.[30]
References
- 1 2 3 4 5 6 7 Ferri's Clinical Advisor 2016: 5 Books in 1. Elsevier Health Sciences. 2015. p. 735. ISBN 9780323378222. Archived from the original on 2022-04-30. Retrieved 2022-04-22.
- 1 2 3 4 5 6 7 8 9 10 11 "Labyrinthitis and vestibular neuritis". nhs.uk. 23 October 2017. Archived from the original on 15 April 2022. Retrieved 27 April 2022.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Greco, A; Macri, GF; Gallo, A; Fusconi, M; De Virgilio, A; Pagliuca, G; Marinelli, C; de Vincentiis, M (2014). "Is vestibular neuritis an immune related vestibular neuropathy inducing vertigo?". Journal of Immunology Research. 2014: 459048. doi:10.1155/2014/459048. PMC 3987789. PMID 24741601.
- ↑ Hogue, JD (June 2015). "Office Evaluation of Dizziness". Primary Care. 42 (2): 249–258. doi:10.1016/j.pop.2015.01.004. PMID 25979586.
- 1 2 Edlow, JA; Carpenter, C; Akhter, M; Khoujah, D; Marcolini, E; Meurer, WJ; Morrill, D; Naples, JG; Ohle, R; Omron, R; Sharif, S; Siket, M; Upadhye, S; E Silva, LOJ; Sundberg, E; Tartt, K; Vanni, S; Newman-Toker, DE; Bellolio, F (May 2023). "Guidelines for reasonable and appropriate care in the emergency department 3 (GRACE-3): Acute dizziness and vertigo in the emergency department". Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 30 (5): 442–486. doi:10.1111/acem.14728. PMID 37166022.
- ↑ Dewyer, Nicholas A.; Kiringoda, Ruwan; McKenna, Michael J. (2018), "Inner Ear Infections (Labyrinthitis)", Infections of the Ears, Nose, Throat, and Sinuses, Springer International Publishing, pp. 79–88, doi:10.1007/978-3-319-74835-1_7, ISBN 978-3-319-74834-4
- ↑ Murdin, Louisa; Hussain, Kiran; Schilder, Anne GM (2013-08-11), "Betahistine for symptoms of vertigo", in The Cochrane Collaboration (ed.), Cochrane Database of Systematic Reviews, John Wiley & Sons, Ltd, pp. CD010696, doi:10.1002/14651858.cd010696
- ↑ "Table 1: The Single Nucleotide Polymorphisms in cathepsin B protein mined from literature (PMID: 16492714)". doi:10.7717/peerj.7425/table-1.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ "Infections of the Inner Ear". Vestibular Disorders Association. Archived from the original on 2022-01-31. Retrieved 2022-04-22.
- ↑ "Inner Ear Infection (Labyrinthitis) Symptoms, Causes, Contagious, Treatment Cure". MedicineNet. Archived from the original on 2021-04-17. Retrieved 2021-02-28.
- ↑ Keith A Marill. "Vestibular Neuronitis". Archived from the original on 2008-07-05. Retrieved 2008-06-28.
- ↑ Marill, Keith (2011-01-13). "Vestibular Neuronitis: Pathology". eMedicine, Medscape Reference. Archived from the original on 2011-08-14. Retrieved 2011-08-07.
- ↑ Martin-Saint-Laurent A, Lavernhe J, Casano G, Simkoff A (March 1990). "Clinical aspects of inflight incapacitations in commercial aviation". Aviation, Space, and Environmental Medicine. 61 (3): 256–60. PMID 2317181.
- ↑ Farmer, Jr JC, ed. (1973). Labyrinthine Dysfunction During Diving. 1st Undersea and Hyperbaric Medical Society Workshop. Vol. UHMS Publication Number WS6-15-74. Undersea and Hyperbaric Medical Society. p. 11. Archived from the original on 2009-07-03. Retrieved 2009-03-11.
- ↑ Kennedy RS (March 1974). "General history of vestibular disorders in diving". Undersea Biomedical Research. 1 (1): 73–81. PMID 4619861. Archived from the original on 2010-06-15. Retrieved 2009-03-11.
- ↑ "Labyrinthitis". www.audiologicaldiagnostics.com. Archived from the original on 2019-11-23. Retrieved 2019-12-02.
- 1 2 "Germany". International Journal of Health Care Quality Assurance. 19 (4). 2017. doi:10.1108/ijhcqa.2006.06219dab.003. ISSN 0952-6862.
- ↑ Smith, Travis; Rider, Justin; Cen, Steven; Borger, Judith (2022). "Vestibular Neuronitis". StatPearls. StatPearls Publishing. Archived from the original on 20 May 2022. Retrieved 26 May 2022.
- 1 2 3 Burton M. J.; Monsell E. M.; Rosenfeld R. M. (2008). "Extracts from the cochrane library: Vestibular rehabilitation for unilateral peripheral vestibular dysfunction (review)". Otolaryngology–Head and Neck Surgery. 138 (4): 415–417. doi:10.1016/j.otohns.2008.02.004. PMID 18359346. S2CID 9907751.
- 1 2 Walker, MF (January 2009). "Treatment of vestibular neuritis". Current Treatment Options in Neurology. 11 (1): 41–5. doi:10.1007/s11940-009-0006-8. PMID 19094835. S2CID 37693582.
- ↑ "Vestibular Rehabilitation Therapy (VRT)". Vestibular Disorders Association. 2011-12-27. Archived from the original on 2020-04-27. Retrieved 2018-05-19.
- 1 2 Fishman, Jonathan M; Burgess, Chris; Waddell, Angus (2010-07-07), "Corticosteroids for the treatment of idiopathic acute vestibular dysfunction (vestibular neuritis)", in The Cochrane Collaboration (ed.), Cochrane Database of Systematic Reviews, John Wiley & Sons, Ltd, pp. CD008607, doi:10.1002/14651858.cd008607
- ↑ "Physical Therapy Rehabilitation". Archived from the original on 2019-10-29. Retrieved 2019-10-29.
- 1 2 Bronstein, Adolfo (February 2002). "Visual and psychological aspects of vestibular disease". Current Opinion in Neurology. 15 (1): 1–3. doi:10.1097/00019052-200202000-00001. PMID 11796943.
- ↑ Fishman, JM; Burgess C; Waddell A (May 2011). "Corticosteroids for the treatment of idiopathic acute vestibular dysfunction (vestibular neuritis)". Cochrane Database Syst Rev (5): CD008607. doi:10.1002/14651858.CD008607.pub2. PMID 21563170.
- ↑ Scholtz, AW; Steindl R; Burchardi N; Bognar-Steinberg I; Baumann W (June 2012). "Comparison of the therapeutic efficacy of a fixed low-dose combination of cinnarizine and dimenhydrinate with betahistine in vestibular neuritis: a randomized, double-blind, non-inferiority study". Clin Drug Investig. 32 (6): 387–399. doi:10.2165/11632410-000000000-00000. PMID 22506537. S2CID 207301804.
- ↑ Solomon, D; Shepard, NT (July 2002). "Chronic Dizziness". Current Treatment Options in Neurology. 4 (4): 281–288. doi:10.1007/s11940-002-0028-y. PMID 12036501. S2CID 38952122.
- 1 2 3 Greco, A.; Macri, G. F.; Gallo, A.; Fusconi, M.; De Virgilio, A.; Pagliuca, G.; Marinelli, C.; de Vincentiis, M. (2014). "Is vestibular neuritis an immune related vestibular neuropathy inducing vertigo?". Journal of Immunology Research. 2014: 459048. doi:10.1155/2014/459048. ISSN 2314-7156. PMC 3987789. PMID 24741601.
- ↑ "Vestibular Neuritis". Cleveland Clinic. Archived from the original on 2019-11-20. Retrieved 2019-11-15.
- ↑ McDonnell, Michelle N; Hillier, Susan L (2015-01-13). Cochrane ENT Group (ed.). "Vestibular rehabilitation for unilateral peripheral vestibular dysfunction". Cochrane Database of Systematic Reviews. 1: CD005397. doi:10.1002/14651858.CD005397.pub4. PMID 25581507.
External links
| Classification | |
|---|---|
| External resources |
- Labyrinthitis at Curlie