Hearing loss
| Hearing loss | |
|---|---|
| Other names: Hearing impaired, Hard of hearing; anakusis or anacusis is total deafness[1] | |
 | |
| The international symbol of deafness and hearing loss | |
| Specialty | Otorhinolaryngology, audiology |
| Symptoms | Decreased ability to hear |
| Complications | Loneliness, Social isolation[2] |
| Types | Conductive, sensorineural, and mixed hearing loss, central auditory dysfunction[3] |
| Causes | Genetics, aging, exposure to noise, some infections, birth complications, trauma to the ear, certain medications or toxins[2] |
| Diagnostic method | Hearing tests |
| Prevention | Immunization, proper care around pregnancy, avoiding loud noise, avoiding certain medications[2] |
| Treatment | Hearing aids, sign language, cochlear implants, subtitles[2] |
| Frequency | 1.33 billion / 18.5% (2015)[4] |
Hearing loss, also known as hearing impairment, is a partial or total inability to hear.[5] A deaf person has little to no hearing.[2] Hearing loss may occur in one or both ears.[2] In children, hearing problems can affect the ability to learn spoken language and in adults it can create difficulties with social interaction and at work.[6] Hearing loss can be temporary or permanent. Hearing loss related to age usually affects both ears and is due to cochlear hair cell loss.[7] In some people, particularly older people, hearing loss can result in loneliness.[2]
Hearing loss may be caused by a number of factors, including: genetics, ageing, exposure to noise, some infections, birth complications, trauma to the ear, and certain medications or toxins.[2] A common condition that results in hearing loss is chronic ear infections.[2] Certain infections during pregnancy, such as cytomegalovirus, syphilis and rubella, may also cause hearing loss in the child.[2][8] Hearing loss is diagnosed when hearing testing finds that a person is unable to hear 25 decibels in at least one ear.[2] Testing for poor hearing is recommended for all newborns.[6] Hearing loss can be categorized as mild (25 to 40 dB), moderate (41 to 55 dB), moderate-severe (56 to 70 dB), severe (71 to 90 dB), or profound (greater than 90 dB).[2] There are three main types of hearing loss: conductive hearing loss, sensorineural hearing loss, and mixed hearing loss.[3]
About half of hearing loss globally is preventable through public health measures.[2] Such practices include immunization, proper care around pregnancy, avoiding loud noise, and avoiding certain medications.[2] The World Health Organization recommends that young people limit exposure to loud sounds and the use of personal audio players to an hour a day in an effort to limit exposure to noise.[9] Early identification and support are particularly important in children.[2] For many hearing aids, sign language, cochlear implants and subtitles are useful.[2] Lip reading is another useful skill some develop.[2] Access to hearing aids, however, is limited in many areas of the world.[2]
As of 2013 hearing loss affects about 1.1 billion people to some degree.[10] It causes disability in about 466 million people (5% of the global population), and moderate to severe disability in 124 million people.[2][11][12] Of those with moderate to severe disability 108 million live in low and middle income countries.[11] Of those with hearing loss, it began during childhood for 65 million.[13] Those who use sign language and are members of Deaf culture see themselves as having a difference rather than an illness.[14] Most members of Deaf culture oppose attempts to cure deafness[15][16][17] and some within this community view cochlear implants with concern as they have the potential to eliminate their culture.[18] The term "hearing impairment" is often viewed negatively as it emphasizes what people cannot do.[14]
Definition

- Hearing loss is defined as diminished acuity to sounds which would otherwise be heard normally.[13] The terms hearing impaired or hard of hearing are usually reserved for people who have relative inability to hear sound in the speech frequencies. The severity of hearing loss is categorized according to the increase in intensity of sound above the usual level required for the listener to detect it.
- Deafness is defined as a degree of loss such that a person is unable to understand speech, even in the presence of amplification.[13] In profound deafness, even the highest intensity sounds produced by an audiometer (an instrument used to measure hearing by producing pure tone sounds through a range of frequencies) may not be detected. In total deafness, no sounds at all, regardless of amplification or method of production, can be heard.
- Speech perception is another aspect of hearing which involves the perceived clarity of a word rather than the intensity of sound made by the word. In humans, this is usually measured with speech discrimination tests, which measure not only the ability to detect sound, but also the ability to understand speech. There are very rare types of hearing loss that affect speech discrimination alone. One example is auditory neuropathy, a variety of hearing loss in which the outer hair cells of the cochlea are intact and functioning, but sound information is not faithfully transmitted by the auditory nerve to the brain.[19]
Use of the terms "hearing impaired", "deaf-mute", or "deaf and dumb" to describe deaf and hard of hearing people is discouraged by many in the deaf community as well as advocacy organizations, as they are offensive to many deaf and hard of hearing people.[20][21]
Hearing standards
Human hearing extends in frequency from 20 to 20,000 Hz, and in intensity from 0 dB to 120 dB HL or more. 0 dB does not represent absence of sound, but rather the softest sound an average unimpaired human ear can hear; some people can hear down to −5 or even −10 dB. Sound is generally uncomfortably loud above 90 dB and 115 dB represents the threshold of pain. The ear does not hear all frequencies equally well: hearing sensitivity peaks around 3000 Hz. There are many qualities of human hearing besides frequency range and intensity that cannot easily be measured quantitatively. However, for many practical purposes, normal hearing is defined by a frequency versus intensity graph, or audiogram, charting sensitivity thresholds of hearing at defined frequencies. Because of the cumulative impact of age and exposure to noise and other acoustic insults, 'typical' hearing may not be normal.[22][23]
Signs and symptoms
- difficulty using the telephone
- loss of sound localization
- difficulty understanding speech, especially of children and women whose voices are of a higher frequency.
- difficulty understanding speech in the presence of background noise (cocktail party effect)
- sounds or speech sounding dull, muffled or attenuated
- need for increased volume on television, radio, music and other audio sources
Hearing loss is sensory, but may have accompanying symptoms:
- pain or pressure in the ears
- a blocked feeling
There may also be accompanying secondary symptoms:
- hyperacusis, heightened sensitivity with accompanying auditory pain to certain intensities and frequencies of sound, sometimes defined as "auditory recruitment"
- tinnitus, ringing, buzzing, hissing or other sounds in the ear when no external sound is present
- vertigo and disequilibrium
- tympanophonia, also known as autophonia, abnormal hearing of one's own voice and respiratory sounds, usually as a result of a patulous (a constantly open) eustachian tube or dehiscent superior semicircular canals
- disturbances of facial movement (indicating a possible tumour or stroke) or in persons with Bell's Palsy
Complications
Hearing loss is associated with Alzheimer's disease and dementia. The risk increases with the hearing loss degree. There are several hypotheses including cognitive resources being redistributed to hearing and social isolation from hearing loss having a negative effect.[24] According to preliminary data, hearing aid using can slow down the decline in cognitive functions.[25]
Cognitive decline
Hearing loss is an increasing concern especially in aging populations, the prevalence of hearing loss increase about two-fold for each decade increase in age after age 40.[26] While the secular trend might decrease individual level risk of developing hearing loss, the prevalence of hearing loss is expected to rise due to the aging population in the US. Another concern about aging process is cognitive decline, which may progress to mild cognitive impairment and eventually dementia.[27] The association between hearing loss and cognitive decline has been studied in various research settings. Despite the variability in study design and protocols, the majority of these studies have found consistent association between age-related hearing loss and cognitive decline, cognitive impairment, and dementia.[28] The association between age-related hearing loss and Alzheimer's disease was found to be nonsignificant, and this finding supports the hypothesis that hearing loss is associated with dementia independent of Alzheimer pathology.[28] There are several hypothesis about the underlying causal mechanism for age-related hearing loss and cognitive decline. One hypothesis is that this association can be explained by common etiology or shared neurobiological pathology with decline in other physiological system.[29] Another possible cognitive mechanism emphasize on individual's cognitive load. As people developing hearing loss in the process of aging, the cognitive load demanded by auditory perception increases, which may lead to change in brain structure and eventually to dementia.[30] One other hypothesis suggests that the association between hearing loss and cognitive decline is mediated through various psychosocial factors, such as decrease in social contact and increase in social isolation.[29] Findings on the association between hearing loss and dementia have significant public health implication, since about 9% of dementia cases can be attributed to hearing loss.[31]
Falls
Falls have important health implications, especially for an aging population where they can lead to significant morbidity and mortality. Elderly people are particularly vulnerable to the consequences of injuries caused by falls, since older individuals typically have greater bone fragility and poorer protective reflexes.[32] Fall-related injury can also lead to burdens on the financial and health care systems.[32] In literature, age-related hearing loss is found to be significantly associated with incident falls.[33] There is also a potential dose-response relationship between hearing loss and falls---greater severity of hearing loss is associated with increased difficulties in postural control and increased prevalence of falls.[34] The underlying causal link between the association of hearing loss and falls is yet to be elucidated. There are several hypotheses that indicate that there may be a common process between decline in auditory system and increase in incident falls, driven by physiological, cognitive, and behavioral factors.[34] This evidence suggests that treating hearing loss has potential to increase health-related quality of life in older adults.[34]
Depression
Depression is one of the leading causes of morbidity and mortality worldwide. In older adults, the suicide rate is higher than it is for younger adults, and more suicide cases are attributable to depression.[35] Different studies have been done to investigate potential risk factors that can give rise to depression in later life. Some chronic diseases are found to be significantly associated with risk of developing depression, such as coronary heart disease, pulmonary disease, vision loss and hearing loss.[36] Hearing loss can attribute to decrease in health-related quality of life, increase in social isolation and decline in social engagement, which are all risk factors for increased risk of developing depression symptoms.[37]
Spoken language ability
Post-lingual deafness is hearing loss that is sustained after the acquisition of language, which can occur due to disease, trauma, or as a side-effect of a medicine. Typically, hearing loss is gradual and often detected by family and friends of affected individuals long before the patients themselves will acknowledge the disability.[38] Post-lingual deafness is far more common than pre-lingual deafness. Those who lose their hearing later in life, such as in late adolescence or adulthood, face their own challenges, living with the adaptations that allow them to live independently.
Prelingual deafness is profound hearing loss that is sustained before the acquisition of language, which can occur due to a congenital condition or through hearing loss before birth or in early infancy. Prelingual deafness impairs an individual's ability to acquire a spoken language in children, but deaf children can acquire spoken language through support from cochlear implants (sometimes combined with hearing aids).[39][40] Non-signing (hearing) parents of deaf babies (90-95% of cases) usually go with oral approach without the support of sign language as the these families lack previous experience with sign language and cannot competently provide it to their children. Unfortunately, this may in some rare cases (late implantation or not sufficient benefit from cochlear implants) bring the risk of language deprivation for the deaf baby[41] because the deaf baby wouldn't have a sign language if the child is unable to acquire spoken language successfully. The 5-10% of cases of deaf babies born into signing families have the potential of age-appropriate development of language due to early exposure to sign language by sign-competent parents, thus they have the potential to meet language milestones, but in sign language in lieu of spoken language.[42]
Causes
Hearing loss has multiple causes, including ageing, genetics, perinatal problems and acquired causes like noise and disease. For some kinds of hearing loss the cause may be classified as of unknown cause.
Noise
Noise-induced hearing loss (NIHL) typically manifests as elevated hearing thresholds (i.e. less sensitivity or muting). Noise exposure is the cause of approximately half of all cases of hearing loss, causing some degree of problems in 5% of the population globally.[44] The majority of hearing loss is not due to age, but due to noise exposure.[45] Various governmental, industry and standards organizations set noise standards.[46] Many people are unaware of the presence of environmental sound at damaging levels, or of the level at which sound becomes harmful. Common sources of damaging noise levels include car stereos, children's toys, motor vehicles, crowds, lawn and maintenance equipment, power tools, gun use, musical instruments, and even hair dryers. Noise damage is cumulative; all sources of damage must be considered to assess risk. In the US, 12.5% of children aged 6–19 years have permanent hearing damage from excessive noise exposure.[47] The World Health Organization estimates that half of those between 12 and 35 are at risk from using personal audio devices that are too loud.[9] Hearing loss in adolescents may be caused by loud noise from toys, music by headphones, and concerts or events.[48]
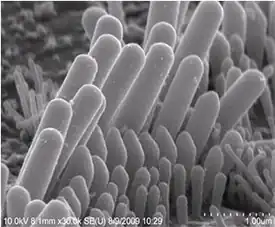
NIHL is caused by long-term exposure to sounds that are either too loud or last too long.[43] This kind of noise exposure can damage the sensory hair cells in the ear that allow one to hear.[43] Once these hair cells are damaged, they do not grow back and a person's ability to hear is diminished.[43] Sounds at or below 70 A-weighted decibels, even after long exposure, are unlikely to cause hearing loss.[49] However, long or repeated exposure to sounds at or above 85 decibels can cause hearing loss.[49] The louder the sound, the shorter the amount of time it takes for noise-induced hearing loss to happen.[49]
Toxins
Some medications may reversibly affect hearing. These medications are considered ototoxic. This includes loop diuretics such as furosemide and bumetanide, non-steroidal anti-inflammatory drugs (NSAIDs) both over-the-counter (aspirin, ibuprofen, naproxen) as well as prescription (celecoxib, diclofenac, etc.), paracetamol, quinine, and macrolide antibiotics.[50] Others may cause permanent hearing loss.[51] The most important group is the aminoglycosides (main member gentamicin) and platinum based chemotherapeutics such as cisplatin and carboplatin.[52][53]
In addition to medications, hearing loss can also result from specific chemicals in the environment: metals, such as lead; solvents, such as toluene (found in crude oil, gasoline[54] and automobile exhaust,[54] for example); and asphyxiants.[55] Combined with noise, these ototoxic chemicals have an additive effect on a person's hearing loss.[55] Hearing loss due to chemicals starts in the high frequency range and is irreversible. It damages the cochlea with lesions and degrades central portions of the auditory system.[55] For some ototoxic chemical exposures, particularly styrene,[56] the risk of hearing loss can be higher than being exposed to noise alone. The effects is greatest when the combined exposure include impulse noise.[57][58] A 2018 informational bulletin by the US Occupational Safety and Health Administration (OSHA) and the National Institute for Occupational Safety and Health (NIOSH) introduces the issue, provides examples of ototoxic chemicals, lists the industries and occupations at risk and provides prevention information.[59]
Injury
There can be damage either to the ear, whether the external or middle ear, to the cochlea, or to the brain centers that process the aural information conveyed by the ears. Damage to the middle ear may include fracture and discontinuity of the ossicular chain. Damage to the inner ear (cochlea) may be caused by temporal bone fracture. People who sustain head injury are especially vulnerable to hearing loss or tinnitus, either temporary or permanent.[60][61]
Age
There is a progressive loss of ability to hear high frequencies with aging known as presbycusis. For men, this can start as early as 25 and women at 30. Although genetically variable it is a normal concomitant of ageing and is distinct from hearing losses caused by noise exposure, toxins or disease agents.[62] Common conditions that can increase the risk of hearing loss in elderly people are high blood pressure, diabetes or the use of certain medications harmful to the ear.[63][64] While everyone loses hearing with age, the amount and type of hearing loss is variable.[65]
Age-related hearing loss is one of the most common conditions affecting older and elderly adults.[43] Approximately one in three people in the US between the ages of 65 and 74 has hearing loss, and nearly half of those older than 75 have difficulty hearing.[43] Having trouble hearing can make it hard to understand and follow a doctor's advice, respond to warnings, and hear phones, doorbells, and smoke alarms.[43] Hearing loss can also make it hard to enjoy talking with family and friends, leading to feelings of isolation.[43] Age-related hearing loss most often occurs in both ears, affecting them equally.[43] Because the loss is gradual, if one has age-related hearing loss one may not realize that they' have lost some of their ability to hear.[43] There are many causes of age-related hearing loss.[43] Most commonly, it arises from changes in the inner ear as we age, but it can also result from changes in the middle ear, or from complex changes along the nerve pathways from the ear to the brain.[43]
Genetics
Hearing loss can be inherited. Around 75–80% of all these cases are inherited by recessive genes, 20–25% are inherited by dominant genes, 1–2% are inherited by X-linked patterns, and fewer than 1% are inherited by mitochondrial inheritance.[66] Syndromic deafness occurs when there are other signs or medical problems aside from deafness in an individual,[66] such as Usher syndrome, Stickler syndrome, Waardenburg syndrome, Alport's syndrome, and neurofibromatosis type 2. Nonsyndromic deafness occurs when there are no other signs or medical problems associated with an individual other than deafness.[66]
Other conditions
Fetal alcohol spectrum disorders are reported to cause hearing loss in up to 64% of infants born to alcoholic mothers, from the ototoxic effect on the developing fetus plus malnutrition during pregnancy from the excess alcohol intake. Premature birth can be associated with sensorineural hearing loss because of an increased risk of hypoxia, hyperbilirubinaemia, ototoxic medication and infection as well as noise exposure in the neonatal units. The risk of hearing loss is greatest for those weighing less than 1500 g at birth.
Disorders responsible for hearing loss include auditory neuropathy,[67][68] Down syndrome,[69] Charcot–Marie–Tooth disease variant 1E,[70] autoimmune disease, multiple sclerosis, meningitis, cholesteatoma, otosclerosis, perilymph fistula, Ménière's disease, recurring ear infections, strokes, superior semicircular canal dehiscence, Pierre Robin, Treacher-Collins, Retinitis Pigmentosa, Pedreds, and Turners syndrome, syphilis, vestibular schwannoma, and viral infections such as measles, mumps, congenital rubella (also called German measles) syndrome, several varieties of herpes viruses,[71] HIV/AIDS,[72] and West Nile virus.
Pathophysiology
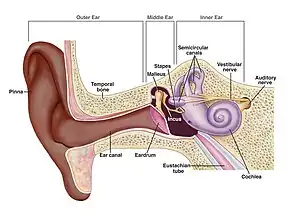
Sound waves reach the outer ear and are conducted down the ear canal to the eardrum, causing it to vibrate. The vibrations are transferred by the 3 tiny ear bones of the middle ear to the fluid in the inner ear. The fluid moves hair cells (stereocilia), and their movement generates nerve impulses which are then taken to the brain by the cochlear nerve.[73][74] The auditory nerve takes the impulses to the brainstem, which sends the impulses to the midbrain. Finally, the signal goes to the auditory cortex of the temporal lobe to be interpreted as sound.[75]
Hearing loss is most commonly caused by long-term exposure to loud noises, from recreation or from work, that damage the hair cells, which do not grow back on their own.[76][77][7]
Older people may lose their hearing from long exposure to noise, changes in the inner ear, changes in the middle ear, or from changes along the nerves from the ear to the brain.[78]
Diagnosis
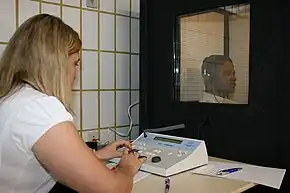
Identification of a hearing loss is usually conducted by a general practitioner medical doctor, otolaryngologist, certified and licensed audiologist, school or industrial audiometrist, or other audiometric technician. Diagnosis of the cause of a hearing loss is carried out by a specialist physician (audiovestibular physician) or otorhinolaryngologist.
Hearing loss is generally measured by playing generated or recorded sounds, and determining whether the person can hear them. Hearing sensitivity varies according to the frequency of sounds. To take this into account, hearing sensitivity can be measured for a range of frequencies and plotted on an audiogram. Other method for quantifying hearing loss is a hearing test using a mobile application or hearing apps, which includes a hearing test.[79][80] Hearing diagnosis using mobile application is similar to the audiometry procedure.[79] Another method for quantifying hearing loss is a speech-in-noise test. which gives an indication of how well one can understand speech in a noisy environment.[81] Otoacoustic emissions test is an objective hearing test that may be administered to toddlers and children too young to cooperate in a conventional hearing test. Auditory brainstem response testing is an electrophysiological test used to test for hearing deficits caused by pathology within the ear, the cochlear nerve and also within the brainstem.
A case history (usually a written form, with questionnaire) can provide valuable information about the context of the hearing loss, and indicate what kind of diagnostic procedures to employ. Examinations include otoscopy, tympanometry, and differential testing with the Weber, Rinne, Bing and Schwabach tests. In case of infection or inflammation, blood or other body fluids may be submitted for laboratory analysis. MRI and CT scans can be useful to identify the pathology of many causes of hearing loss.
Hearing loss is categorized by severity, type, and configuration. Furthermore, a hearing loss may exist in only one ear (unilateral) or in both ears (bilateral). Hearing loss can be temporary or permanent, sudden or progressive. The severity of a hearing loss is ranked according to ranges of nominal thresholds in which a sound must be so it can be detected by an individual. It is measured in decibels of hearing loss, or dB HL. There are three main types of hearing loss: conductive hearing loss, sensorineural hearing loss, and mixed hearing loss.[13] An additional problem which is increasingly recognised is auditory processing disorder which is not a hearing loss as such but a difficulty perceiving sound. The shape of an audiogram shows the relative configuration of the hearing loss, such as a Carhart notch for otosclerosis, 'noise' notch for noise-induced damage, high frequency rolloff for presbycusis, or a flat audiogram for conductive hearing loss. In conjunction with speech audiometry, it may indicate central auditory processing disorder, or the presence of a schwannoma or other tumor.
People with unilateral hearing loss or single-sided deafness (SSD) have difficulty in hearing conversation on their impaired side, localizing sound, and understanding speech in the presence of background noise. One reason for the hearing problems these patients often experience is due to the head shadow effect.[82]
Prevention
It is estimated that half of cases of hearing loss are preventable.[83] About 60% of hearing loss in children under the age of 15 can be avoided.[2] A number of preventive strategies are effective including: immunization against rubella to prevent congenital rubella syndrome, immunization against H. influenza and S. pneumoniae to reduce cases of meningitis, and avoiding or protecting against excessive noise exposure.[13] The World Health Organization also recommends immunization against measles, mumps, and meningitis, efforts to prevent premature birth, and avoidance of certain medication as prevention.[84] World Hearing Day is a yearly event to promote actions to prevent hearing damage.
Noise exposure is the most significant risk factor for noise-induced hearing loss that can be prevented. Different programs exist for specific populations such as school-age children, adolescents and workers.[85] Education regarding noise exposure increases the use of hearing protectors.[86] The use of antioxidants is being studied for the prevention of noise-induced hearing loss, particularly for scenarios in which noise exposure cannot be reduced, such as during military operations.[87]
Workplace noise regulation
Noise is widely recognized as an occupational hazard. In the United States, the National Institute for Occupational Safety and Health (NIOSH) and the Occupational Safety and Health Administration (OSHA) work together to provide standards and enforcement on workplace noise levels.[88][89] The hierarchy of hazard controls demonstrates the different levels of controls to reduce or eliminate exposure to noise and prevent hearing loss, including engineering controls and personal protective equipment (PPE).[90] Other programs and initiative have been created to prevent hearing loss in the workplace. For example, the Safe-in-Sound Award was created to recognize organizations that can demonstrate results of successful noise control and other interventions.[91] Additionally, the Buy Quiet program was created to encourage employers to purchase quieter machinery and tools.[92] By purchasing less noisy power tools like those found on the NIOSH Power Tools Database and limiting exposure to ototoxic chemicals, great strides can be made in preventing hearing loss.[93]
Companies can also provide personal hearing protector devices tailored to both the worker and type of employment. Some hearing protectors universally block out all noise, and some allow for certain noises to be heard. Workers are more likely to wear hearing protector devices when they are properly fitted.[94]
Often interventions to prevent noise-induced hearing loss have many components. A 2017 Cochrane review found that stricter legislation might reduce noise levels.[95] Providing workers with information on their noise exposure levels was not shown to decrease exposure to noise. Ear protection, if used correctly, can reduce noise to safer levels, but often, providing them is not sufficient to prevent hearing loss. Engineering noise out and other solutions such as proper maintenance of equipment can lead to noise reduction, but further field studies on resulting noise exposures following such interventions are needed. Other possible solutions include improved enforcement of existing legislation and better implementation of well-designed prevention programmes, which have not yet been proven conclusively to be effective. The conclusion of the Cochrane Review was that further research could modify what is now regarding the effectiveness of the evaluated interventions.[95]
The Institute for Occupational Safety and Health of the German Social Accident Insurance has created a hearing impairment calculator based on the ISO 1999 model for studying threshold shift in relatively homogeneous groups of people, such as workers with the same type of job. The ISO 1999 model estimates how much hearing impairment in a group can be ascribed to age and noise exposure. The result is calculated via an algebraic equation that uses the A-weighted noise exposure level, how many years the people were exposed to this noise, how old the people are, and their sex. The model’s estimations are only useful for people without hearing loss due to non-job related exposure and can be used for prevention activities.[96]
Screening
The United States Preventive Services Task Force recommends neonatal hearing screening for all newborns.[6]
The American Academy of Pediatrics advises that children should have their hearing tested several times throughout their schooling:[47]
- When they enter school
- At ages 6, 8, and 10
- At least once during middle school
- At least once during high school
While the American College of Physicians indicated that there is not enough evidence to determine the utility of screening in adults over 50 years old who do not have any symptoms,[97] the American Language, Speech Pathology and Hearing Association recommends that adults should be screened at least every decade through age 50 and at 3-year intervals thereafter, to minimize the detrimental effects of the untreated condition on quality of life.[98] For the same reason, the US Office of Disease Prevention and Health Promotion included as one of Healthy People 2020 objectives: to increase the proportion of persons who have had a hearing examination.[99]
Management

Management depends on the specific cause if known as well as the extent, type and configuration of the hearing loss. Sudden hearing loss due to and underlying nerve problem may be treated with corticosteroids.[100]
Most hearing loss, that resulting from age and noise, is progressive and irreversible, and there are currently no approved or recommended treatments. A few specific kinds of hearing loss are amenable to surgical treatment. In other cases, treatment is addressed to underlying pathologies, but any hearing loss incurred may be permanent. Some management options include hearing aids, cochlear implants, assistive technology, and closed captioning.[7] This choice depends on the level of hearing loss, type of hearing loss, and personal preference. Hearing apps are another option.[80] For people with bilateral hearing loss, it is not clear if bilateral hearing aids (hearing aids in both ears) are better than a unilateral hearing aid (hearing aid in one ear).[7]
Epidemiology
_world_map_-_DALY_-_WHO2004.svg.png.webp)
|
no data
<250
250–295
295–340
340–385
385–430
430–475
|
475–520
520–565
565–610
610–655
655–700
>700
|
Globally, hearing loss affects about 10% of the population to some degree.[44] It caused moderate to severe disability in 124.2 million people as of 2004 (107.9 million of whom are in low and middle income countries).[11] Of these 65 million acquired the condition during childhood.[13] At birth ~3 per 1000 in developed countries and more than 6 per 1000 in developing countries have hearing problems.[13]
Hearing loss increases with age. In those between 20 and 35 rates of hearing loss are 3% while in those 44 to 55 it is 11% and in those 65 to 85 it is 43%.[6]
A 2017 report by the World Health Organization estimated the costs of unaddressed hearing loss and the cost-effectiveness of interventions, for the health-care sector, for the education sector and as broad societal costs.[101] Globally, the annual cost of unaddressed hearing loss was estimated to be in the range of $750–790 billion international dollars.
The International Organization for Standardization (ISO) developed the ISO 1999 standards for the estimation of hearing thresholds and noise-induced hearing impairment.[102] They used data from two noise and hearing study databases, one presented by Burns and Robinson (Hearing and Noise in Industry, Her Majesty's Stationery Office, London, 1970) and by Passchier-Vermeer (1968).[103] As race are some of the factors that can affect the expected distribution of pure-tone hearing thresholds several other national or regional datasets exist, from Sweden,[104] Norway,[105] South Korea,[106] the United States[107] and Spain.[108]
In the United States hearing is one of the health outcomes measure by the National Health and Nutrition Examination Survey (NHANES), a survey research program conducted by the National Center for Health Statistics. It examines health and nutritional status of adults and children in the United States. Data from the United States in 2011-2012 found that rates of hearing loss has declined among adults aged 20 to 69 years, when compared with the results from an earlier time period (1999-2004). It also found that adult hearing loss is associated with increasing age, sex, race/ethnicity, educational level, and noise exposure.[109] Nearly one in four adults had audiometric results suggesting noise-induced hearing loss. Almost one in four adults who reported excellent or good hearing had a similar pattern (5.5% on both sides and 18% on one side). Among people who reported exposure to loud noise at work, almost one third had such changes.[110]
Society and culture
%252C_2008.jpg.webp)
People with extreme hearing loss may communicate through sign languages. Sign languages convey meaning through manual communication and body language instead of acoustically conveyed sound patterns. This involves the simultaneous combination of hand shapes, orientation and movement of the hands, arms or body, and facial expressions to express a speaker's thoughts. "Sign languages are based on the idea that vision is the most useful tool a deaf person has to communicate and receive information".[111]
Deaf culture refers to a tight-knit cultural group of people whose primary language is signed, and who practice social and cultural norms which are distinct from those of the surrounding hearing community. This community does not automatically include all those who are clinically or legally deaf, nor does it exclude every hearing person. According to Baker and Padden, it includes any person or persons who "identifies him/herself as a member of the Deaf community, and other members accept that person as a part of the community,"[112] an example being children of deaf adults with normal hearing ability. It includes the set of social beliefs, behaviors, art, literary traditions, history, values, and shared institutions of communities that are influenced by deafness and which use sign languages as the main means of communication.[113][114] Members of the Deaf community tend to view deafness as a difference in human experience rather than a disability or disease.[115][116] When used as a cultural label especially within the culture, the word deaf is often written with a capital D and referred to as "big D Deaf" in speech and sign. When used as a label for the audiological condition, it is written with a lower case d.[113][114]
Research
Stem cell transplant and gene therapy
A 2005 study achieved successful regrowth of cochlea cells in guinea pigs.[117] However, the regrowth of cochlear hair cells does not imply the restoration of hearing sensitivity, as the sensory cells may or may not make connections with neurons that carry the signals from hair cells to the brain. A 2008 study has shown that gene therapy targeting Atoh1 can cause hair cell growth and attract neuronal processes in embryonic mice. Some hope that a similar treatment will one day ameliorate hearing loss in humans.[118]
Recent research, reported in 2012 achieved growth of cochlear nerve cells resulting in hearing improvements in gerbils,[119] using stem cells. Also reported in 2013 was regrowth of hair cells in deaf adult mice using a drug intervention resulting in hearing improvement.[120] The Hearing Health Foundation in the US has embarked on a project called the Hearing Restoration Project.[121] Also Action on Hearing Loss in the UK is also aiming to restore hearing.[122]
Researchers reported in 2015 that genetically deaf mice which were treated with TMC1 gene therapy recovered some of their hearing.[123][124] In 2017, additional studies were performed to treat Usher syndrome[125] and here, a recombinant adeno-associated virus seemed to outperform the older vectors.[126][127]
Audition
Besides research studies seeking to improve hearing, such as the ones listed above, research studies on the deaf have also been carried out in order to understand more about audition. Pijil and Shwarz (2005) conducted their study on the deaf who lost their hearing later in life and, hence, used cochlear implants to hear. They discovered further evidence for rate coding of pitch, a system that codes for information for frequencies by the rate that neurons fire in the auditory system, especially for lower frequencies as they are coded by the frequencies that neurons fire from the basilar membrane in a synchronous manner. Their results showed that the subjects could identify different pitches that were proportional to the frequency stimulated by a single electrode. The lower frequencies were detected when the basilar membrane was stimulated, providing even further evidence for rate coding.[128]
See also
References
- ↑ Elsevier, Dorland's Illustrated Medical Dictionary, Elsevier, archived from the original on 2014-01-11, retrieved 2020-08-06.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 "Deafness and hearing loss Fact sheet N°300". March 2015. Archived from the original on 16 May 2015. Retrieved 23 May 2015.
{{cite web}}: CS1 maint: unfit URL (link) - 1 2 Shearer AE, Hildebrand MS, Smith RJ (2014). "Deafness and Hereditary Hearing Loss Overview". In Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJ, Stephens K, Amemiya A (eds.). GeneReviews [Internet]. Seattle (WA): University of Washington, Seattle. PMID 20301607. Archived from the original on 2019-02-09. Retrieved 2020-08-06.
- ↑ Global Burden of Disease Study 2013 Collaborators (October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- ↑ "Deafness". Encyclopædia Britannica Online. Encyclopædia Britannica Inc. 2011. Archived from the original on 2012-06-25. Retrieved 2012-02-22.
- 1 2 3 4 Lasak JM, Allen P, McVay T, Lewis D (March 2014). "Hearing loss: diagnosis and management". Primary Care. 41 (1): 19–31. doi:10.1016/j.pop.2013.10.003. PMID 24439878.
- 1 2 3 4 Schilder, Anne Gm; Chong, Lee Yee; Ftouh, Saoussen; Burton, Martin J. (2017). "Bilateral versus unilateral hearing aids for bilateral hearing impairment in adults". The Cochrane Database of Systematic Reviews. 12: CD012665. doi:10.1002/14651858.CD012665.pub2. ISSN 1469-493X. PMC 6486194. PMID 29256573.
- ↑ Fowler KB (December 2013). "Congenital cytomegalovirus infection: audiologic outcome". Clinical Infectious Diseases. 57 Suppl 4 (suppl_4): S182-4. doi:10.1093/cid/cit609. PMC 3836573. PMID 24257423.
- 1 2 "1.1 billion people at risk of hearing loss WHO highlights serious threat posed by exposure to recreational noise" (PDF). who.int. 27 February 2015. Archived (PDF) from the original on 1 May 2015. Retrieved 2 March 2015.
- ↑ Global Burden of Disease Study 2013 Collaborators (August 2015). "Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 386 (9995): 743–800. doi:10.1016/s0140-6736(15)60692-4. PMC 4561509. PMID 26063472.
- 1 2 3 WHO (2008). The global burden of disease: 2004 update (PDF). Geneva, Switzerland: World Health Organization. p. 35. ISBN 9789241563710. Archived (PDF) from the original on 2013-06-24.
- ↑ Olusanya BO, Neumann KJ, Saunders JE (May 2014). "The global burden of disabling hearing impairment: a call to action". Bulletin of the World Health Organization. 92 (5): 367–73. doi:10.2471/blt.13.128728. PMC 4007124. PMID 24839326.
- 1 2 3 4 5 6 7 Elzouki, Abdelaziz Y (2012). Textbook of clinical pediatrics (2 ed.). Berlin: Springer. p. 602. ISBN 9783642022012. Archived from the original on 2015-12-14.
- 1 2 "Community and Culture - Frequently Asked Questions". nad.org. National Association of the Deaf. Archived from the original on 27 December 2015. Retrieved 31 July 2014.
- ↑ "Sound and Fury - Cochlear Implants - Essay". www.pbs.org. PBS. Archived from the original on 2015-07-06. Retrieved 2015-08-01.
- ↑ "Understanding Deafness: Not Everyone Wants to Be 'Fixed'". www.theatlantic.com. The Atlantic. 2013-08-09. Archived from the original on 2015-07-30. Retrieved 2015-08-01.
- ↑ Williams, Sally (2012-09-13). "Why not all deaf people want to be cured". www.telegraph.co.uk. The Daily Telegraph. Archived from the original on 2015-09-24. Retrieved 2015-08-02.
- ↑ Sparrow, Robert (2005). "Defending Deaf Culture: The Case of Cochlear Implants" (PDF). The Journal of Political Philosophy. 13 (2): 135–152. doi:10.1111/j.1467-9760.2005.00217.x. Archived (PDF) from the original on 4 December 2014. Retrieved 30 November 2014.
- ↑ eBook: Current Diagnosis & Treatment in Otolaryngology: Head & Neck Surgery, Lalwani, Anil K. (Ed.) Chapter 44: Audiologic Testing by Brady M. Klaves, PhD, Jennifer McKee Bold, AuD, Access Medicine
- ↑ Bennett, ReBecca (May 2019). "Time for Change". The Hearing Journal. 72 (5): 16. doi:10.1097/01.HJ.0000559500.67179.7d.
- ↑ "Community and Culture - Frequently Asked Questions". nad.org. National Association of the Deaf. Archived from the original on 2015-12-27. Retrieved 27 Jan 2016.
- ↑ ANSI 7029:2000/BS 6951 Acoustics - Statistical distribution of hearing thresholds as a function of age
- ↑ ANSI S3.5-1997 Speech Intelligibility Index (SII)
- ↑ Thomson RS, Auduong P, Miller AT, Gurgel RK (April 2017). "Hearing loss as a risk factor for dementia: A systematic review". Laryngoscope Investigative Otolaryngology. 2 (2): 69–79. doi:10.1002/lio2.65. PMC 5527366. PMID 28894825.
- ↑ Hoppe U, Hesse G (2017-12-18). "Hearing aids: indications, technology, adaptation, and quality control". GMS Current Topics in Otorhinolaryngology, Head and Neck Surgery. 16: Doc08. doi:10.3205/cto000147. PMC 5738937. PMID 29279726.
- ↑ Lin FR, Niparko JK, Ferrucci L (November 2011). "Hearing loss prevalence in the United States". Archives of Internal Medicine. 171 (20): 1851–2. doi:10.1001/archinternmed.2011.506. PMID 22083573. Archived from the original on 2021-08-28. Retrieved 2020-08-06.
- ↑ Park HL, O'Connell JE, Thomson RG (December 2003). "A systematic review of cognitive decline in the general elderly population". International Journal of Geriatric Psychiatry. 18 (12): 1121–34. doi:10.1002/gps.1023. PMID 14677145. Archived from the original on 2021-08-28. Retrieved 2020-08-06.
- 1 2 Loughrey DG, Kelly ME, Kelley GA, Brennan S, Lawlor BA (February 2018). "Association of Age-Related Hearing Loss With Cognitive Function, Cognitive Impairment, and Dementia: A Systematic Review and Meta-analysis". JAMA Otolaryngology-- Head & Neck Surgery. 144 (2): 115–126. doi:10.1001/jamaoto.2017.2513. PMC 5824986. PMID 29222544. Archived from the original on 2021-08-28. Retrieved 2020-08-06.
- 1 2 Thomson RS, Auduong P, Miller AT, Gurgel RK (April 2017). "Hearing loss as a risk factor for dementia: A systematic review". Laryngoscope Investigative Otolaryngology. 2 (2): 69–79. doi:10.1002/lio2.65. PMID 28894825. Archived from the original on 2021-08-28. Retrieved 2020-08-06.
- ↑ Pichora-Fuller MK, Mick P, Reed M (August 2015). "Hearing, Cognition, and Healthy Aging: Social and Public Health Implications of the Links between Age-Related Declines in Hearing and Cognition". Seminars in Hearing. 36 (3): 122–39. doi:10.1055/s-0035-1555116. PMID 27516713. Archived from the original on 2021-08-28. Retrieved 2020-08-06.
- ↑ Ford AH, Hankey GJ, Yeap BB, Golledge J, Flicker L, Almeida OP (June 2018). "Hearing loss and the risk of dementia in later life". Maturitas. 112: 1–11. doi:10.1016/j.maturitas.2018.03.004. PMID 29704910. Archived from the original on 2021-08-28. Retrieved 2020-08-06.
- 1 2 Dhital A, Pey T, Stanford MR (September 2010). "Visual loss and falls: a review". Eye. 24 (9): 1437–46. doi:10.1038/eye.2010.60. PMID 20448666. Archived from the original on 2021-02-28. Retrieved 2020-08-06.
- ↑ Jiam NT, Li C, Agrawal Y (November 2016). "Hearing loss and falls: A systematic review and meta-analysis". The Laryngoscope. 126 (11): 2587–2596. doi:10.1002/lary.25927. PMID 27010669. Archived from the original on 2020-03-03. Retrieved 2020-08-06.
- 1 2 3 Agmon M, Lavie L, Doumas M (June 2017). "The Association between Hearing Loss, Postural Control, and Mobility in Older Adults: A Systematic Review". Journal of the American Academy of Audiology. 28 (6): 575–588. doi:10.3766/jaaa.16044. PMID 28590900.
- ↑ Fiske A, Wetherell JL, Gatz M (April 2009). "Depression in older adults". Annual Review of Clinical Psychology. 5 (1): 363–89. doi:10.1146/annurev.clinpsy.032408.153621. PMC 2852580. PMID 19327033.
- ↑ Huang CQ, Dong BR, Lu ZC, Yue JR, Liu QX (April 2010). "Chronic diseases and risk for depression in old age: a meta-analysis of published literature". Ageing Research Reviews. Microbes and Ageing. 9 (2): 131–41. doi:10.1016/j.arr.2009.05.005. PMID 19524072.
- ↑ Arlinger S (July 2003). "Negative consequences of uncorrected hearing loss--a review". International Journal of Audiology. 42 Suppl 2 (sup2): 2S17-20. doi:10.3109/14992020309074639. PMID 12918624. Archived from the original on 2021-08-28. Retrieved 2020-08-06.
- ↑ Meyer C, Scarinci N, Ryan B, Hickson L (December 2015). ""This Is a Partnership Between All of Us": Audiologists' Perceptions of Family Member Involvement in Hearing Rehabilitation". American Journal of Audiology. 24 (4): 536–48. doi:10.1044/2015_AJA-15-0026. PMID 26649683. Archived from the original on 2021-08-28. Retrieved 2020-08-06.
- ↑ Niparko JK, Tobey EA, Thal DJ, Eisenberg LS, Wang NY, Quittner AL, Fink NE (April 2010). "Spoken language development in children following cochlear implantation". JAMA. 303 (15): 1498–506. doi:10.1001/jama.2010.451. PMC 3073449. PMID 20407059.
- ↑ Kral A, O'Donoghue GM (October 2010). "Profound deafness in childhood". The New England Journal of Medicine. 363 (15): 1438–50. doi:10.1056/NEJMra0911225. PMID 20925546. Archived from the original on 2021-08-28. Retrieved 2020-08-06.
- ↑ Hall WC (May 2017). "What You Don't Know Can Hurt You: The Risk of Language Deprivation by Impairing Sign Language Development in Deaf Children". Maternal and Child Health Journal. 21 (5): 961–965. doi:10.1007/s10995-017-2287-y. PMC 5392137. PMID 28185206.
- ↑ Mayberry, Rachel (2007). "When timing is everything: Age of first-language acquisition effects on second-language learning". Applied Psycholinguistics. 28 (3): 537–549. doi:10.1017/s0142716407070294.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 National Institute on Deafness and Other Communication Disorders (16 March 2022). "Age-Related Hearing Loss". National Institutes of Health. Archived from the original on 7 August 2020. Retrieved 6 August 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - 1 2 Oishi N, Schacht J (June 2011). "Emerging treatments for noise-induced hearing loss". Expert Opinion on Emerging Drugs. 16 (2): 235–45. doi:10.1517/14728214.2011.552427. PMC 3102156. PMID 21247358.
- ↑ "CDC - NIOSH Science Blog – A Story of Impact..." cdc.gov. Archived from the original on 2015-06-13.
- ↑ In the United States, United States Environmental Protection Agency, Occupational Safety and Health Administration, National Institute for Occupational Safety and Health, Mine Safety and Health Administration, and numerous state government agencies among others, set noise standards.
- 1 2 "Noise-Induced Hearing Loss: Promoting Hearing Health Among Youth". CDC Healthy Youth!. CDC. 2009-07-01. Archived from the original on 2009-12-21.
- ↑ de Laat JA, van Deelen L, Wiefferink K (September 2016). "Hearing Screening and Prevention of Hearing Loss in Adolescents". The Journal of Adolescent Health. 59 (3): 243–245. doi:10.1016/j.jadohealth.2016.06.017. PMID 27562364.
- 1 2 3 National Institute on Deafness and Other Communication Disorders (16 March 2022). "Noise-Induced Hearing Loss". National Institutes of Health. Archived from the original on 14 April 2020. Retrieved 2 February 2023.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ Curhan SG, Shargorodsky J, Eavey R, Curhan GC (September 2012). "Analgesic use and the risk of hearing loss in women". American Journal of Epidemiology. 176 (6): 544–54. doi:10.1093/aje/kws146. PMC 3530351. PMID 22933387.
- ↑ Cone, Barbara; Dorn, Patricia; Konrad-Martin, Dawn; Lister, Jennifer; Ortiz, Candice; Schairer, Kim. "Ototoxic Medications (Medication Effects)". American Speech-Language-Hearing Association. Archived from the original on 2020-08-03.
- ↑ Rybak LP, Mukherjea D, Jajoo S, Ramkumar V (November 2009). "Cisplatin ototoxicity and protection: clinical and experimental studies". The Tohoku Journal of Experimental Medicine. 219 (3): 177–86. doi:10.1620/tjem.219.177. PMC 2927105. PMID 19851045.
- ↑ Rybak LP, Ramkumar V (October 2007). "Ototoxicity". Kidney International. 72 (8): 931–5. doi:10.1038/sj.ki.5002434. PMID 17653135.
- 1 2 "Tox Town – Toluene – Toxic chemicals and environmental health risks where you live and work – Text Version". toxtown.nlm.nih.gov. Archived from the original on 2010-06-09. Retrieved 2010-06-09.
- 1 2 3 Morata, Thais C. "Addressing the Risk for Hearing Loss from Industrial Chemicals". CDC. Archived from the original on 2009-01-22. Retrieved 2008-06-05.
- ↑ Johnson, Ann-Christin (2008-09-09). "Occupational exposure to chemicals and hearing impairment – the need for a noise notation" (PDF). Karolinska Institutet: 1–48. Archived from the original (PDF) on 2012-09-06. Retrieved 2009-06-19.
- ↑ Venet T, Campo P, Thomas A, Cour C, Rieger B, Cosnier F (March 2015). "The tonotopicity of styrene-induced hearing loss depends on the associated noise spectrum". Neurotoxicology and Teratology. 48: 56–63. doi:10.1016/j.ntt.2015.02.003. PMID 25689156.
- ↑ Fuente A, Qiu W, Zhang M, Xie H, Kardous CA, Campo P, Morata TC (March 2018). "Use of the kurtosis statistic in an evaluation of the effects of noise and solvent exposures on the hearing thresholds of workers: An exploratory study" (PDF). The Journal of the Acoustical Society of America. 143 (3): 1704–1710. Bibcode:2018ASAJ..143.1704F. doi:10.1121/1.5028368. PMID 29604694. Archived (PDF) from the original on 2019-08-31. Retrieved 2020-08-06.
- ↑ "Preventing Hearing Loss Caused by Chemical (Ototoxicity) and Noise Exposure" (PDF). Archived (PDF) from the original on 4 April 2018. Retrieved 4 April 2018.
- ↑ Oesterle EC (March 2013). "Changes in the adult vertebrate auditory sensory epithelium after trauma". Hearing Research. 297: 91–8. doi:10.1016/j.heares.2012.11.010. PMC 3637947. PMID 23178236.
- ↑ Eggermont JJ (January 2017). "Acquired hearing loss and brain plasticity". Hearing Research. 343: 176–190. doi:10.1016/j.heares.2016.05.008. PMID 27233916.
- ↑ Robinson DW, Sutton GJ (1979). "Age effect in hearing - a comparative analysis of published threshold data". Audiology. 18 (4): 320–34. doi:10.3109/00206097909072634. PMID 475664.
- ↑ Worrall L, Hickson LM (2003). "Communication activity limitations". In Worrall LE, Hickson LM (eds.). Communication disability in aging: from prevention to intervention. Clifton Park, NY: Delmar Learning. pp. 141–142.
- ↑ Akinpelu OV, Mujica-Mota M, Daniel SJ (March 2014). "Is type 2 diabetes mellitus associated with alterations in hearing? A systematic review and meta-analysis". The Laryngoscope. 124 (3): 767–76. doi:10.1002/lary.24354. PMID 23945844.
- ↑ "Hearing Loss and Older Adults" (Last Updated June 3, 2016). National Institute on Deafness and Other Communication Disorders. 2016-01-26. Archived from the original on October 4, 2016. Retrieved September 11, 2016.
- 1 2 3 Rehm, Heidi. "The Genetics of Deafness; A Guide for Patients and Families" (PDF). Harvard Medical School Center For Hereditary Deafness. Harvard Medical School. Archived from the original (PDF) on 2013-10-19.
- ↑ Starr A, Sininger YS, Pratt H (2011). "The varieties of auditory neuropathy". Journal of Basic and Clinical Physiology and Pharmacology. 11 (3): 215–30. doi:10.1515/JBCPP.2000.11.3.215. PMID 11041385. Archived from the original on 2021-08-28. Retrieved 2020-08-06.
- ↑ Starr A, Picton TW, Sininger Y, Hood LJ, Berlin CI (June 1996). "Auditory neuropathy". Brain. 119 ( Pt 3) (3): 741–53. doi:10.1093/brain/119.3.741. PMID 8673487.
- ↑ Rodman R, Pine HS (June 2012). "The otolaryngologist's approach to the patient with Down syndrome". Otolaryngologic Clinics of North America. 45 (3): 599–629, vii–viii. doi:10.1016/j.otc.2012.03.010. PMID 22588039.
- ↑ McKusick, Victor A.; Kniffen, Cassandra L. (30 January 2012). "# 118300 CHARCOT-MARIE-TOOTH DISEASE AND DEAFNESS". Online Mendelian Inheritance in Man. Archived from the original on 1 October 2018. Retrieved 2 March 2018.
- ↑ Byl FM, Adour KK (March 1977). "Auditory symptoms associated with herpes zoster or idiopathic facial paralysis". The Laryngoscope. 87 (3): 372–9. doi:10.1288/00005537-197703000-00010. PMID 557156.
- ↑ Araújo E, Zucki F, Corteletti LC, Lopes AC, Feniman MR, Alvarenga K (2012). "Hearing loss and acquired immune deficiency syndrome: systematic review". Jornal da Sociedade Brasileira de Fonoaudiologia. 24 (2): 188–92. doi:10.1590/s2179-64912012000200017. PMID 22832689.
- ↑ "How We Hear". American Speech-Language-Hearing Association. Archived from the original on 3 March 2018. Retrieved 2 March 2018.
- ↑ "How We Hear". Archived from the original on 1 May 2017.
- ↑ "How Do We Hear?". NIDCD. January 3, 2018. Archived from the original on August 13, 2020. Retrieved August 6, 2020.
- ↑ "What Is Noise-Induced Hearing Loss?". NIH - Noisy Planet. December 27, 2017. Archived from the original on October 17, 2020. Retrieved August 6, 2020.
- ↑ "CDC - Noise and Hearing Loss Prevention - Preventing Hearing Loss, Risk Factors - NIOSH Workplace Safety and Health Topic". NIOSH/CDC. 5 February 2018. Archived from the original on 3 March 2018. Retrieved 3 March 2018.
- ↑ "Age-Related Hearing Loss". NIDCD. 18 August 2015. Archived from the original on 7 August 2020. Retrieved 6 August 2020.
- 1 2 Shojaeemend H, Ayatollahi H (October 2018). "Automated Audiometry: A Review of the Implementation and Evaluation Methods". Healthcare Informatics Research. 24 (4): 263–275. doi:10.4258/hir.2018.24.4.263. PMC 6230538. PMID 30443414.
- 1 2 Keidser G, Convery E (April 2016). "Self-Fitting Hearing Aids: Status Quo and Future Predictions". Trends in Hearing. 20: 233121651664328. doi:10.1177/2331216516643284. PMC 4871211. PMID 27072929.
- ↑ Jansen S, Luts H, Dejonckere P, van Wieringen A, Wouters J (2013). "Efficient hearing screening in noise-exposed listeners using the digit triplet test" (PDF). Ear and Hearing. 34 (6): 773–8. doi:10.1097/AUD.0b013e318297920b. PMID 23782715. Archived (PDF) from the original on 2017-09-22. Retrieved 2020-08-06.
- ↑ Lieu JE (May 2004). "Speech-language and educational consequences of unilateral hearing loss in children". Archives of Otolaryngology–Head & Neck Surgery. 130 (5): 524–30. doi:10.1001/archotol.130.5.524. PMID 15148171.
- ↑ Graham, edited by John M.; Baguley, David M. (2009). Ballantyne's Deafness (7th ed.). Chichester: John Wiley & Sons. p. 16. ISBN 978-0-470-74441-3. Archived from the original on 2017-09-08.
- ↑ "Childhood hearing loss: act now, here's how!" (PDF). WHO. 2016. p. 6. Archived (PDF) from the original on 6 March 2016. Retrieved 2 March 2016.
Over 30% of childhood hearing loss is caused by diseases such as measles, mumps, rubella, meningitis and ear infections. These can be prevented through immunization and good hygiene practices. Another 17% of childhood hearing loss results from complications at birth, including prematurity, low birth weight, birth asphyxia and neonatal jaundice. Improved maternal and child health practices would help to prevent these complications. The use of ototoxic medicines in expectant mothers and newborns, which is responsible for 4% of childhood hearing loss, could potentially be avoided.
- ↑ Davis A, McMahon CM, Pichora-Fuller KM, Russ S, Lin F, Olusanya BO, Chadha S, Tremblay KL (April 2016). "Aging and Hearing Health: The Life-course Approach". The Gerontologist. 56 Suppl 2 (Suppl_2): S256-67. doi:10.1093/geront/gnw033. PMC 6283365. PMID 26994265.
- ↑ El Dib RP, Mathew JL, Martins RH (April 2012). El Dib RP (ed.). "Interventions to promote the wearing of hearing protection". The Cochrane Database of Systematic Reviews. 4 (4): CD005234. doi:10.1002/14651858.CD005234.pub5. PMID 22513929.
- ↑ Stucken EZ, Hong RS (October 2014). "Noise-induced hearing loss: an occupational medicine perspective". Current Opinion in Otolaryngology & Head and Neck Surgery. 22 (5): 388–93. doi:10.1097/moo.0000000000000079. PMID 25188429.
- ↑ "Noise and Hearing Loss Prevention". Centers for Disease Control and Prevention: National Institute for Occupational Safety and Health. Archived from the original on July 9, 2016. Retrieved July 15, 2016.
- ↑ "Safety and Health Topics: Occupational Noise Exposure". Occupational Safety and Health Administration. Archived from the original on May 6, 2016. Retrieved July 15, 2015.
- ↑ "Controls for Noise Exposure". Centers for Disease Control and Prevention: National Institute for Occupational Safety and Health. Archived from the original on July 4, 2016. Retrieved July 15, 2016.
- ↑ "Excellence in Hearing Loss Prevention Award". Safe-in-Sound. Archived from the original on May 27, 2016. Retrieved July 15, 2016.
- ↑ "Buy Quiet". Centers for Disease Control and Prevention: National Institute for Occupational Safety and Health. Archived from the original on August 8, 2016. Retrieved July 15, 2016.
- ↑ "PowerTools Database". Centers for Disease Control and Prevention: National Institute for Occupational Safety and Health. Archived from the original on June 30, 2016. Retrieved July 15, 2016.
- ↑ "CDC - NIOSH Publications and Products - Occupationally-Induced Hearing Loss (2010-136)". CDC.gov. 2010. doi:10.26616/NIOSHPUB2010136. Archived from the original on 2016-05-12.
- 1 2 Tikka C, Verbeek JH, Kateman E, Morata TC, Dreschler WA, Ferrite S (July 2017). "Interventions to prevent occupational noise-induced hearing loss". The Cochrane Database of Systematic Reviews. 7: CD006396. doi:10.1002/14651858.cd006396.pub4. PMC 6353150. PMID 28685503.
- ↑ Institute for Occupational Safety and Health of the German Social Accident Insurance. "Hearing impairment calculator". Archived from the original on 2020-08-09.
- ↑ Moyer, Virginia A. (2012-11-06). "Screening for Hearing Loss in Older Adults: U.S. Preventive Services Task Force Recommendation Statement". Annals of Internal Medicine. The American College of Physicians. pp. 655–661. Archived from the original on 2012-10-27. Retrieved 2012-11-06.
- ↑ "Who Should be Screened for Hearing Loss". www.asha.org. Archived from the original on 2017-03-17. Retrieved 2017-03-17.
- ↑ "Hearing and Other Sensory or Communication Disorders | Healthy People 2020". www.healthypeople.gov. Archived from the original on 2017-03-18. Retrieved 2017-03-17.
- ↑ Chandrasekhar SS, Tsai Do BS, Schwartz SR, Bontempo LJ, Faucett EA, Finestone SA, et al. (August 2019). "Clinical Practice Guideline: Sudden Hearing Loss (Update) Executive Summary". Otolaryngology–Head and Neck Surgery. 161 (2): 195–210. doi:10.1177/0194599819859883. PMID 31369349.
- ↑ World Health Organization, WHO (2017). Global costs of unaddressed hearing loss and cost-effectiveness of interventions: a WHO report. Geneva: World Health Organization. pp. 5–10. ISBN 978-92-4-151204-6.
- ↑ ISO, International Organization for Standardization (2013). Acoustics—Estimation of noise induced hearing loss. Geneva, Switzerland: International Organization for Standardization. p. 20.
- ↑ Passchier-Vermeer, W (1969). Hearing loss due to exposure to steady state broadband noise. Delft, Netherlands: TNO, Instituut voor gezondheidstechniek. pp. Report 35 Identifier 473589.
- ↑ Johansson M, Arlinger S (2004-07-07). "Reference data for evaluation of occupationally noise-induced hearing loss". Noise & Health. 6 (24): 35–41. PMID 15703139.
- ↑ Tambs K, Hoffman HJ, Borchgrevink HM, Holmen J, Engdahl B (May 2006). "Hearing loss induced by occupational and impulse noise: results on threshold shifts by frequencies, age and gender from the Nord-Trøndelag Hearing Loss Study". International Journal of Audiology. 45 (5): 309–17. doi:10.1080/14992020600582166. PMID 16717022.
- ↑ Jun HJ, Hwang SY, Lee SH, Lee JE, Song JJ, Chae S (March 2015). "The prevalence of hearing loss in South Korea: data from a population-based study". The Laryngoscope. 125 (3): 690–4. doi:10.1002/lary.24913. PMID 25216153. Archived from the original on 2021-08-28. Retrieved 2020-08-06.
- ↑ Flamme GA, Deiters K, Needham T (March 2011). "Distributions of pure-tone hearing threshold levels among adolescents and adults in the United States by gender, ethnicity, and age: Results from the US National Health and Nutrition Examination Survey". International Journal of Audiology. 50 Suppl 1: S11-20. doi:10.3109/14992027.2010.540582. PMID 21288063.
- ↑ Rodríguez Valiente A, Roldán Fidalgo A, García Berrocal JR, Ramírez Camacho R (August 2015). "Hearing threshold levels for an otologically screened population in Spain". International Journal of Audiology. 54 (8): 499–506. doi:10.3109/14992027.2015.1009643. PMID 25832123.
- ↑ Hoffman HJ, Dobie RA, Losonczy KG, Themann CL, Flamme GA (March 2017). "Declining Prevalence of Hearing Loss in US Adults Aged 20 to 69 Years". JAMA Otolaryngology–Head & Neck Surgery. 143 (3): 274–285. doi:10.1001/jamaoto.2016.3527. PMC 5576493. PMID 27978564.
- ↑ Carroll YI, Eichwald J, Scinicariello F, Hoffman HJ, Deitchman S, Radke MS, Themann CL, Breysse P (February 2017). "Vital Signs: Noise-Induced Hearing Loss Among Adults - United States 2011-2012". MMWR. Morbidity and Mortality Weekly Report. 66 (5): 139–144. doi:10.15585/mmwr.mm6605e3. PMC 5657963. PMID 28182600.
- ↑ "American Sign Language". NIDCD. 2015-08-18. Archived from the original on 15 November 2016. Retrieved 17 November 2016.
- ↑ Baker, Charlotte; Carol Padden (1978). American Sign Language: A Look at Its Story, Structure and Community.
- 1 2 Padden, Carol A.; Humphries, Tom (Tom L.) (2005). Inside Deaf Culture. Cambridge, MA: Harvard University Press. p. 1. ISBN 978-0-674-01506-7. Archived from the original on 2020-07-31. Retrieved 2020-08-06.
- 1 2 Jamie Berke (9 February 2010). "Deaf Culture - Big D Small D". About.com. Archived from the original on 4 March 2016. Retrieved 22 November 2013.
- ↑ Ladd, Paddy (2003). Understanding Deaf Culture: In Search of Deafhood. Multilingual Matters. p. 502. ISBN 978-1-85359-545-5. Archived from the original on 2020-07-31. Retrieved 2020-08-06.
- ↑ Lane, Harlan L.; Richard Pillard; Ulf Hedberg (2011). The People of the Eye: Deaf Ethnicity and Ancestry. Oxford University Press. p. 269. ISBN 978-0-19-975929-3. Archived from the original on 2020-08-09. Retrieved 2020-08-06.
- ↑ Coghlan, Andy (2005-02-14). "Gene therapy is first deafness 'cure'". NewScientist.com News Service. Archived from the original on 2008-09-14.
- ↑ Gubbels SP, Woessner DW, Mitchell JC, Ricci AJ, Brigande JV (September 2008). "Functional auditory hair cells produced in the mammalian cochlea by in utero gene transfer". Nature. 455 (7212): 537–41. Bibcode:2008Natur.455..537G. doi:10.1038/nature07265. PMC 2925035. PMID 18754012.
- ↑ Gewin, Virginia (2012-09-12). "Human embryonic stem cells restore gerbil hearing". Nature News. doi:10.1038/nature.2012.11402. Archived from the original on 2012-12-14. Retrieved 2013-01-22.
- ↑ Ander, Davida. "Drug may reverse permanent deafness by regenerating cells of inner ear: Harvard study". National Post. National Post. Archived from the original on 2013-02-16.
- ↑ "Hearing Health Foundation". HHF. Archived from the original on 2013-01-27. Retrieved 2013-01-22.
- ↑ "Biomedical research – Action On Hearing Loss". RNID. Archived from the original on 2013-01-23. Retrieved 2013-01-22.
- ↑ Gallacher, James (9 July 2015). "Deafness could be treated by virus, say scientists". UK: BBC. Archived from the original on 9 July 2015. Retrieved 9 July 2015.
- ↑ Askew C, Rochat C, Pan B, Asai Y, Ahmed H, Child E, Schneider BL, Aebischer P, Holt JR (July 2015). "Tmc gene therapy restores auditory function in deaf mice". Science Translational Medicine. 7 (295): 295ra108. doi:10.1126/scitranslmed.aab1996. PMC 7298700. PMID 26157030.
- ↑ Isgrig K, Shteamer JW, Belyantseva IA, Drummond MC, Fitzgerald TS, Vijayakumar S, Jones SM, Griffith AJ, Friedman TB, Cunningham LL, Chien WW (March 2017). "Gene Therapy Restores Balance and Auditory Functions in a Mouse Model of Usher Syndrome". Molecular Therapy. 25 (3): 780–791. doi:10.1016/j.ymthe.2017.01.007. PMC 5363211. PMID 28254438.
- ↑ Landegger LD, Pan B, Askew C, Wassmer SJ, Gluck SD, Galvin A, Taylor R, Forge A, Stankovic KM, Holt JR, Vandenberghe LH (March 2017). "A synthetic AAV vector enables safe and efficient gene transfer to the mammalian inner ear". Nature Biotechnology. 35 (3): 280–284. doi:10.1038/nbt.3781. PMC 5340646. PMID 28165475.
- ↑ Pan B, Askew C, Galvin A, Heman-Ackah S, Asai Y, Indzhykulian AA, Jodelka FM, Hastings ML, Lentz JJ, Vandenberghe LH, Holt JR, Géléoc GS (March 2017). "Gene therapy restores auditory and vestibular function in a mouse model of Usher syndrome type 1c". Nature Biotechnology. 35 (3): 264–272. doi:10.1038/nbt.3801. PMC 5340578. PMID 28165476.
- ↑ Carlson NR (2010). Physiology of behavior (11th ed.). Upper Saddle River, New Jersey: Pearson Education, Inc.
External links
| Classification | |
|---|---|
| External resources |
| Wikiquote has quotations related to: Hearing loss |
- Hearing loss at Curlie
- National Institute for the Prevention of Deafness and other Communication Disorders Archived 2020-08-07 at the Wayback Machine
- World Health Organization Global Costs of unaddressed hearing loss and cost-effectiveness of interventions, 2017 Archived 2021-08-28 at the Wayback Machine
- World Health Organization, Deafness and Hearing Loss Archived 2020-08-06 at the Wayback Machine
- "Hearing Loss in Children". Hearing Loss in Children Home. Archived from the original on 18 March 2017. Retrieved 17 March 2017.
- Occupational Noise and Hearing Loss Prevention Archived 2020-11-04 at the Wayback Machine (NIOSH)
- OSHA-NIOSH 2018. Preventing Hearing Loss Caused by Chemical (Ototoxicity) and Noise Exposure Safety and Health Information Bulletin (SHIB), Occupational Safety and Health Administration and the National Institute for Occupational Safety and Health. SHIB 03-08-2018. DHHS (NIOSH) Publication No. 2018-124.
- Centers for Disease Control and Prevention Vital Signs- Hearing Loss Loud Noises Damage Hearing Archived 2020-07-28 at the Wayback Machine
- "Using Total Worker Health Concepts to Address Hearing Health (2019-155)". 27 September 2019. doi:10.26616/NIOSHPUB2019155revised. Archived from the original on 8 December 2019. Retrieved 4 March 2020.