Otomycosis
| Otomycosis | |
|---|---|
| Other names: Fungal external otitis | |
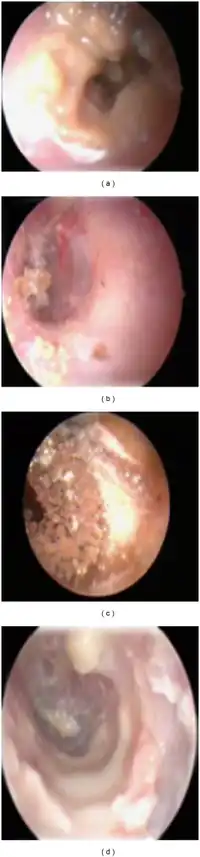 | |
| Otomycotic debris and spores in relation to the ear canal. | |
| Symptoms | varies widely, only itching in early cases, hearing impairment if the fungal debris blocks the ear canal, severe pressure type pain in advanced cases |
| Complications | perforation of the tympanic membrane, rarely invasion of the middle ear |
Otomycosis is a fungal ear infection,[1] a superficial mycotic infection of the outer ear canal. It is more common in tropical countries. The infection may be either subacute or acute and is characterized by malodorous discharge, inflammation, pruritus, scaling, and severe discomfort. The mycosis results in inflammation, superficial epithelial exfoliation, masses of debris containing hyphae, suppuration, and pain.[2]
Signs and Symptoms
Otomycosis does not usually cause as much canal skin edema as does acute bacterial external otitis. While a severe pressure type of pain is a prominent feature of advanced cases, the ear is usually much less tender, if at all, to traction or tragal pressure. Appearance of the fungus is variable, most commonly gray, white, or black, often intermixed with cerumen and clinging to the canal skin. Gray concretions may be present. It can require significant time to remove, best done with suction and microscopic ear instruments, by an ENT specialist.
Cause
Most fungal ear infections are caused by Aspergillus niger, Aspergillus fumigatus, Penicillium and Candida albicans.[3]Otomycosis commonly results from overuse of antibacterial ear drops, which should never be used for more than 7 days. In such cases the fungus is an opportunist that results from antibacterial suppression of the normal bacterial flora, combined with the steroid the drops also contain. [4]
Diagnosis
Otoscopy (exam of the ear) is best done with a binocular microscope that provides adequate lighting, depth perception, and the ability to instrument the ear to comfortably remove the fungus. Findings range from scattered saprophytic fungal colonies of various colors, causing no symptoms, to densely packed fungal debris, often intermixed with cerumen (wax), filling the entire canal and involving the tympanic membrane (eardrum). The fungus can cling to the skin and tympanic membrane, presumably because of invading hyphae, and can require significant time to accomplish complete removal.
Treatment
Treatment of otomycosis typically includes microscopic suction to remove fungal mass, topical antibiotics to be discontinued, and treatment with antifungal eardrops for three weeks.[5]
References
- ↑ "Otomycosis". Medical Dictionary. TheFreeDictionary. Archived from the original on 2019-03-23. Retrieved 2022-03-07.
- ↑ Kaur R, Mittal N, Kakkar M, Aggarwal AK, Mathur MD (August 2000). "Otomycosis: a clinicomycologic study". Ear Nose Throat J. 79 (8): 606–9. doi:10.1177/014556130007900815. PMID 10969470.
- ↑ Munguia R, Daniel SJ (April 2008). "Ototopical antifungals and otomycosis: a review". Int. J. Pediatr. Otorhinolaryngol. 72 (4): 453–9. doi:10.1016/j.ijporl.2007.12.005. PMID 18279975.
- ↑ Vennewald I, Klemm E (March 2010). "Otomycosis: Diagnosis and treatment". Clin Dermatol. 28 (2): 202–11. doi:10.1016/j.clindermatol.2009.12.003. PMID 20347664.
- ↑ Sangaré I, Amona FM, Ouedraogo RW, Zida A, Ouedraogo MS (June 2021). "Otomycosis in Africa: Epidemiology, diagnosis and treatment". J Mycol Med. 31 (2): 101115. doi:10.1016/j.mycmed.2021.101115. PMID 33516991.
External links
| Classification |
|---|