Chronic mucocutaneous candidiasis
| Chronic mucocutaneous candidiasis | |
|---|---|
| Other names: CMC[1]Familial chronic mucocutaneous candidiasis ,CARD9 deficiency, Invasive candidiasis-deep dermatophytosis syndrome | |
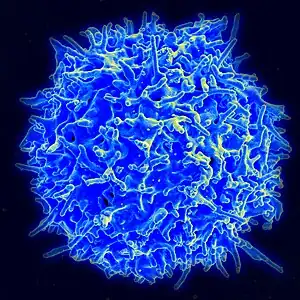 | |
| This condition is due to T-cells(immune) disorder | |
| Specialty | Infectious diseases, dermatology |
| Symptoms | Skin ulcer[2] |
| Types | CANDF1,2,3,4,5,6,7,8 and 9j |
| Diagnostic method | Thyroid function test, Liver function test[3][4] |
| Treatment | Systemic antifungal therapy[4] |
Chronic mucocutaneous candidiasis is an immune disorder of T cells,[4] it is characterized by chronic infections with Candida that are limited to mucosal surfaces, skin, and nails.[5]: 310 It can also be associated with other types of infections, such as HIV[6]
Types
The 9 types of Chronic mucocutaneous candidiasis are the following:[7]
| Type | OMIMα | Gene | Locus |
|---|---|---|---|
| CANDF1 | 114580 | - | 2p |
| CANDF2 | 212050 | CARD9 | 9q34.3 |
| CANDF3 | 607644 | - | 11 |
| CANDF4 | 613108 | CLEC7A | 12p13.2-p12.3 |
| CANDF5 | 613953 | IL17RA | 22q11 |
| CANDF6 | 613956 | IL17F | 6p12 |
| CANDF7 | 614162 | STAT1 | 2q32 |
| CANDF8 | 615527 | TRAF3IP2 | 6q21 |
| CANDF9 | 616445 | IL17RC | 3q25 |
Symptoms and signs

The symptoms of this condition are hyperkeratosis, skin ulcer, dyspareunia, endocardium abnormality, vision problems, hepatitis, seizures, hematuria and meningitis.[2]
Associated Diseases or Conditions
There are a number of disorders associated with chronic mucocutaneous candidiasis including endocrine dysfunctions, vitiligo, malabsorption syndromes, neoplasms and others. In most people, chronic mucocutaneous candidiasis is correlated to abnormalities in cell mediated immunity (T-lymphocyte mediated response)[8][9][10]
The T-lymphocytes fail to produce the necessary cytokines that are required for immunity against Candida. Current effective treatments include antifungal drugs and, for long term remissions, restoration of cellular immunity.[11]
People with autosomal-dominant mucocutaneous candidiasis may be at risk for epidermoid esophageal cancer due to the nitrosamine compounds produced by chronic candida infection.[12][13]
Cause
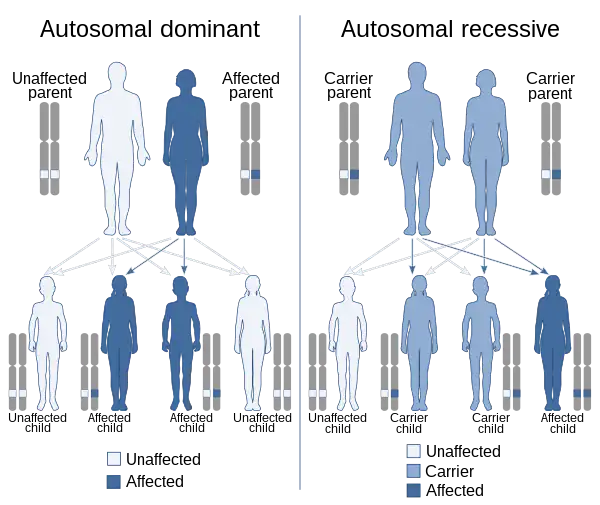
Chronic mucocutaneous candidiasis can be inherited either autosomal dominant or autosomal recessive.[1] There are 9 types of this condition with the first CANDF1 being located at 2p22.3-p21 (cytogenetically).[7]
All nine types carry information to create proteins involved in the human immune response to infections that attack the body [14](fungal)
Mechanism
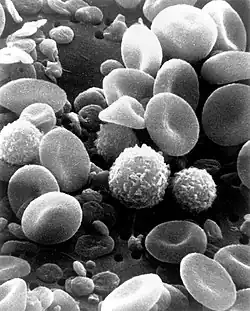
The mechanism of the human immune system has it normally fighting in an infection (like Candida). Initially Th17 cells are made by the immune system, which in turn produces interleukin-17 (IL-17). Inflammation is induced and white blood cells confront infection.[15]
Chronic mucocutaneous candidiasis mutations affect IL-17 by inhibiting its pathway. This in turn affects the human immune systems ability to fight infection, in total there are 9 possible types of this condition.[15][16]
The majority of the nine genes lead to chronic mucocutaneous candidiasis, however CARD9 gene mutations is solely responsible for causing systemic candidiasis [14]
Diagnosis
Chronic mucocutaneous candidiasis can be diagnosed in an affected individual via the following methods/tests:[3][4]
- Thyroid function test
- Liver function test
- Cellular immunity test
- Skin biopsy
- Genetic testing
Treatment
Management for an individual with chronic mucocutaneous candidiasis consists of the following (relapse occurs once treatment is ceased, in many cases):[4][17]
- Systemic antifungal therapy (e.g. Fluconazole)
- Transfer factor
- Combination therapy
- Screening (annually)
Prevalence
The frequency of this condition,Chronic mucocutaneous candidiasis, is unknown at this time.[14]
See also
References
- 1 2 RESERVED, INSERM US14 -- ALL RIGHTS. "Orphanet: Chronic mucocutaneous candidiasis". www.orpha.net. Archived from the original on 2017-07-14. Retrieved 2017-06-09.
- 1 2 "Candidiasis familial chronic mucocutaneous, autosomal recessive | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Archived from the original on 2018-04-17. Retrieved 2017-06-09.
- 1 2 "Familial chronic mucocutaneous candidiasis - Conditions - GTR - NCBI". www.ncbi.nlm.nih.gov. Archived from the original on 2018-05-26. Retrieved 2017-06-09.
- 1 2 3 4 5 "Chronic Mucocutaneous Candidiasis: Background, Pathophysiology, Epidemiology". Medscape. 3 May 2017. Archived from the original on 10 June 2017. Retrieved 8 June 2017.
- ↑ James, William D.; Berger, Timothy G. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 978-0-7216-2921-6.
- ↑ MD, A. Wesley Burks; MD, N. Franklin Adkinson Jr , Jr; MD, Bruce S. Bochner; MD, William W. Busse; Holgate, Stephen T.; MD, Robert F. Lemanske, Jr; MD, Robyn E. O'Hehir (18 October 2013). Middleton's Allergy 2-Volume Set: Principles and Practice (Expert Consult Premium Edition - Enhanced Online Features and Print). Elsevier Health Sciences. p. 1135. ISBN 978-0-323-08593-9. Archived from the original on 29 October 2021. Retrieved 28 October 2021.
- 1 2 "OMIM Entry - % 114580 - CANDIDIASIS, FAMILIAL, 1; CANDF1". omim.org. Archived from the original on 31 March 2021. Retrieved 9 June 2017.
- ↑ "Chronic Mucocutaneous Candidiasis - Immune Disorders". Merck Manuals Consumer Version. Archived from the original on 3 October 2021. Retrieved 23 October 2021.
- ↑ Holland, Steven M.; Rosenzweig, Sergio D.; Schumacher, Richard F.; Notarangelo, Luigi D. (1 January 2017). "78 - Immunodeficiencies". Infectious Diseases (Fourth Edition). Elsevier. pp. 705–722.e2. ISBN 978-0-7020-6285-8. Archived from the original on 29 August 2021. Retrieved 27 October 2021.
- ↑ Kirkpatrick, C. H. (May 1989). "Chronic mucocutaneous candidiasis". European Journal of Clinical Microbiology & Infectious Diseases: Official Publication of the European Society of Clinical Microbiology. 8 (5): 448–456. doi:10.1007/BF01964059. ISSN 0934-9723. Archived from the original on 2 February 2021. Retrieved 5 November 2021.
- ↑ Kirkpatrick, Charles H. (February 2001). "Chronic mucocutaneous candidiasis". The Pediatric Infectious Disease Journal. 20 (2): 197–206. doi:10.1097/00006454-200102000-00017. PMID 11224843.
- ↑ "Autosomal dominant candidiasis familial chronic mucocutaneous | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Archived from the original on 14 April 2021. Retrieved 25 October 2021.
- ↑ Wise, James L.; Murray, Joseph A. (1 June 2002). "Esophageal manifestations of dermatologic disease". Current Gastroenterology Reports. 4 (3): 205–212. doi:10.1007/s11894-002-0064-5. ISSN 1534-312X. Archived from the original on 16 June 2018. Retrieved 4 November 2021.
- 1 2 3 "Familial candidiasis: MedlinePlus Genetics". medlineplus.gov. Archived from the original on 13 September 2021. Retrieved 30 October 2021.
- 1 2 Reference, Genetics Home. "familial candidiasis". Genetics Home Reference. Archived from the original on 2017-06-27. Retrieved 2017-06-09.
- ↑ Smeekens, Sanne P; van de Veerdonk, Frank L; Kullberg, Bart Jan; Netea, Mihai G (2013). "Genetic susceptibility to Candida infections". EMBO Molecular Medicine. 5 (6): 805–813. doi:10.1002/emmm.201201678. ISSN 1757-4676. PMC 3779444. PMID 23629947.
- ↑ Teng, Joyce; Marqueling, Ann L.; Benjamin, Latanya (2016-12-15). Therapy in Pediatric Dermatology: Management of Pediatric Skin Disease. Springer. p. 265. ISBN 9783319436302. Archived from the original on 2021-10-09. Retrieved 2021-08-30.
Further reading
- Kauffman, Carol A.; Pappas, Peter G.; Sobel, Jack D.; Dismukes, William E. (2011). Essentials of Clinical Mycology. Springer Science & Business Media. ISBN 9781441966407. Archived from the original on 9 October 2021. Retrieved 9 June 2017.
- Ostler, H. Bruce (2004). Diseases of the Eye and Skin: A Color Atlas. Lippincott Williams & Wilkins. ISBN 9780781749992. Archived from the original on 9 October 2021. Retrieved 9 June 2017.
- Dominguez-Villar, Margarita; Hafler, David A. (1 April 2011). "An Innate Role for IL-17". Science. pp. 47–48. doi:10.1126/science.1205311. Archived from the original on 1 November 2021. Retrieved 1 November 2021.
External links
| Classification | |
|---|---|
| External resources |